Procedural and post-procedural cerebral ischaemic events still represent the Achilles’ heel of carotid artery stenting (CAS). While the occurrence of periprocedural events has decreased with the use of embolic protection devices (EPDs) tailored to specific anatomic and clinical characteristics1, large-scale clinical data have shown that adverse neurological events in the post-procedural period still account for a significant proportion of all CAS-related neurological events.
The average risk of post-procedural ipsilateral stroke is still quite disconcerting, (i.e., 0.4% per year)2,3. This phenomenon could be related to plaque protrusion through stent struts, which occurs in up to two thirds of cases and is related to plaque morphology/symptomatic status and stent type. The risk of periprocedural cerebral embolisation in transfemoral CAS has been shown to be higher with open-cell vs. closed-cell stents, suggesting a causal relationship with the relative increased risk of post-procedural stroke with use of open-cell rather than closed-cell stent designs4. Recently, the risk of post-procedural adverse cerebral events has been definitively linked to the size of the carotid stent free cell area, indicating a robust impact of the carotid stent design on CAS outcome5. The need for an increase in plaque coverage and decrease in the risk of debris dislodgement through the stent struts has led to the design of a new generation of dual layered carotid stents.
These devices basically consist of a novel thin-strut nitinol stent combined with mesh covering (which can be made of nitinol or of polyethylene terephthalate [PET]). The smallest cell size in the mesh can have a free cell area that goes down to less than 500 μm2 (i.e., nitinol) or even to 165 μm2 (i.e., PET). This feature allows the device to trap and exclude thrombus and plaque debris so as to prevent acute and late embolic events from the target lesion. The first clinical studies evaluating these devices6,7 demonstrated device safety, but they were not sufficiently powered for device-related and clinical endpoints.
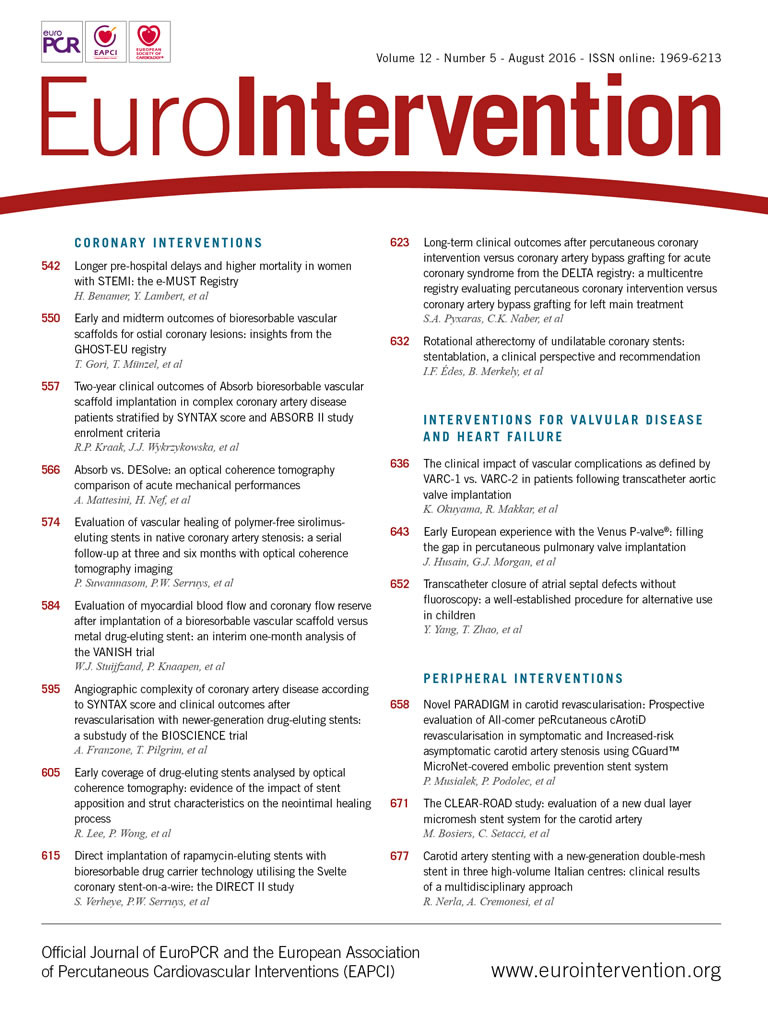
In this issue of EuroIntervention, three different studies evaluate the role of dual layered mesh-covered carotid stent systems in daily clinical practice. Musialek et al8 report the results of the PARADIGM (Prospective evaluation of All-comer peRcutaneous cArotiD revascularisation in symptomatic and Increased-risk asymptomatic carotid artery stenosis using CGuard™ MicroNet-covered embolic prevention stent system) trial, which evaluated the routine use of the dual layer PET mesh-covered carotid stent system (CGuard; InspireMD, Boston, MA, USA) in a high-volume clinical practice of carotid revascularisation in symptomatic (>50%) and increased stroke risk asymptomatic carotid stenosis. The results of this study demonstrated that the application of the CGuard can be employed in 100% of CAS procedures (independently from lesion type) and is compatible with all types of temporary neuroprotection systems. One criticism of this device type relates to stent rigidity and the possible related occurrence of post-procedural residual stenosis.
As observed in the PARADIGM trial, the use of CGuard allows angiographic optimisation of the CAS result to achieve optimal angiographic results with minimal residual stenosis.
In the other two studies, the clinical results of the use of dual layer nitinol mesh-covered carotid stent systems are reported. Nerla et al9 report the clinical results of a large real-world population of patients receiving a Roadsaver® stent (Terumo, Tokyo, Japan) to treat carotid artery disease. Their findings suggest that the Roadsaver stent is safe and can be implanted in a wide variety of anatomies and lesions. The 30-day clinical outcome is assured when the procedure is performed by expert operators performing CAS in high-volume centres.
Since the use of a dual layer stent has been advocated to reduce post-procedural cerebral embolisation by reducing plaque material prolapsing between stent struts, the investigators assessed the amount of plaque prolapsing from the struts by OCT measurement10. The reported frequency of plaque prolapse after CAS, as assessed by OCT, has been estimated as occurring in one out of three patients receiving a stent with a closed-cell design and in two out of three patients receiving one with an open-cell design11. Nerla et al reported that, using a dual layer stent, plaque prolapse occurred in less than a tenth of the patients and, in most cases, plaque material was entrapped between the two layers of struts, thus explaining the sustained antiembolic action of the stent, which is clinically demonstrated by the lack of cerebrovascular events at 30-day follow-up. Moreover, in this Italian registry, it has been proven definitively that, despite the presence of a double-layered mesh across the external carotid artery ostium, this remained well patent in all cases.
In the remaining manuscript on this topic within this issue of the journal, Bosiers et al12 report the results of the CLEAR-ROAD (Physician-initiated Carotid Trial Investigating the Efficacy of Endovascular Treatment of Carotid Arterial Disease With the Multi-layer RoadSaver Stent) trial, which evaluated the clinical outcomes at 30 days of 100 patients at high risk for carotid endarterectomy requiring carotid revascularisation treated by means of stenting with the Roadsaver carotid stent. The CLEAR-ROAD study results not only demonstrate that CAS by means of a dual layer nitinol mesh-covered carotid stent system is a safe and effective alternative treatment for patients considered at high risk for surgery but also support a striking hypothesis.
It is well accepted that the use of EPDs does eliminate the risk of cerebral embolisation, and in addition some investigators believe that the stent design could have a more important impact on the resulting complications in CAS than in EPDs. Large-scale multicentre registries have demonstrated that the majority of the clinical events related to cerebral embolisation occur in the first 24 hours after the procedure13 when the stent is the only device in place to contain plaque debris embolisation. Almost half of the patients enrolled in the CLEAR-ROAD trial were treated without cerebral protection. Despite this, the rate of clinical events related to cerebral embolisation was not significantly affected by the use of EPDs.
These findings will fuel the fire of the debate on the need to use EPDs for CAS. In the case of a patient with extracranial carotid artery stenosis, the magnitude of the procedure-related and long-term risk of ipsilateral stroke will ultimately determine whether surgical, endovascular or medical treatment is preferable. In new symptomatic patients, this choice will be determined by the timing of symptoms, the age of the patient, and comorbidities14.
The treatment of asymptomatic carotid artery stenosis is a controversial issue, since the available literature suggests that the annual rate of ipsilateral stroke among medically treated asymptomatic patients has declined over the past two decades and is now <1%, a rate that is very similar to that observed in ACT I and CREST after stenting14. A wise approach is to reserve revascularisation for patients with symptomatic severe stenosis or for asymptomatic patients who are shown to be at higher risk for stroke with medical therapy than with intervention. A phenomenon that is common to almost every medical trial is that, when completed, it provides data that are obsolete for current medical practice. The NASCET and the ACST trials established the need for carotid revascularisation by comparing a modern surgical strategy to an outdated medical therapy and, for this reason, their results have been criticised in the last twenty years by medical therapy believers.
Due to the data reported in this issue, we are now going to see a similar scenario when the results of the Carotid Revascularization and Medical Management for Asymptomatic Carotid Stenosis Trial (CREST-2) become available. Endovascular therapy believers will criticise the trial design because it compared modern medical therapy with an outdated endovascular strategy. As of today, we should consider the combination of EPD, dual layered carotid stents and operator experience15 the most modern and efficient strategy to minimise CAS-related neurologic complications. Only a proper comparison between modern medical therapy and modern endovascular therapy will definitively identify which patients will benefit from an intervention rather than medical therapy alone. Unfortunately, this trial is not yet underway.
Conflict of interest statement
The authors have no conflicts of interest to declare.