Abstract
Aims: Anatomic and physiologic changes that are induced by radial access may lead to a decrease of upper limb function at long-term follow-up; however, this has never been studied. We aimed to study the long-term effect of transradial catheterisation on upper limb function.
Methods and results: Between January 2013 and April 2014, upper limb function was assessed in a total of 348 patients with complete one-year follow-up after coronary catheterisation. Upper limb function was assessed with the self-reported shortened version of the DASH questionnaire. The presence and severity of upper extremity cold intolerance was assessed with the self-reported CISS questionnaire. Both questionnaires were completed before the catheterisation and at one-year follow-up. Higher scores represent worse upper limb functionality or symptoms. The non-parametric Wilcoxon signed-rank test was used to assess the change of upper limb function and symptoms over time. Extremity complaints were reported at one-month and one-year follow-up. At one-year follow-up, upper limb function did not change over time when catheterisation was performed through the radial artery (p-value 0.20). Upper extremity was also not affected by cold intolerance at one-year follow-up (p-value 0.09). Extremity complaints were reported equally in both access groups and diminished significantly over time (p-value <0.001).
Conclusions: Upper limb function was not affected at long-term follow-up after transradial procedures.
Abbreviations
ACS: acute coronary syndrome
CABG: coronary artery bypass graft
CAD: coronary artery disease
DM: diabetes mellitus
MCID: minimal clinically important difference
TF: transfemoral
TR: transradial
VAS: visual analogue scale
Introduction
The radial artery is recommended as the primary access site for coronary procedures because of the lower rate of access-related bleedings and possibly lower mortality rate1-3, cost-effectiveness4 and patient preference5 as compared to access via the femoral artery.
Along with the experience of the operator and improvement of materials and anticoagulation, complications with transradial (TR) procedures have decreased over time. Radial artery occlusion (RAO) is still the most common complication after TR access6. However, RAO rarely leads to acute ischaemic complications due to the double circulation of the hand and extensive collateralisation7,8. Still, disabling ischaemic hand problems have been reported when collateral circulation appeared to be insufficient9. Insufficient blood supply may be present in up to 57% of all patients due to incompleteness of the palmary arch10, which may explain symptomatic RAO in a significant number of patients6. TR catheterisation may also affect non-vascular structures, which can potentially lead to complaints and dysfunction of the upper extremity11. Previously we reported that, at one-month follow-up, upper extremity function was not affected after TR access12. However, upper limb function might still be compromised at a later stage, for example by the development of cold intolerance13, chronic intimal thickening14 and endothelial dysfunction15. We therefore investigated the self-reported upper limb function and cold intolerance with two validated questionnaires (Online Appendix 1, Online Appendix 2) at baseline and at one-year follow-up.
Methods
STUDY DESIGN AND POPULATION
The Assessment of disability after Coronary procedures using Radial Access (ACRA) study was designed to evaluate the consequence of TR coronary catheterisation on upper limb function at one month as previously published12. In the present manuscript we present data on the secondary analysis of upper limb function at one-year follow-up.
The type of vascular access was left to the discretion of the operator, who was blinded to all study-related tests (including the result of the Allen test). The study protocol was approved by the local ethics committee. Patients with ST-elevation myocardial infarction or haemodynamic instability or those not willing or unable to answer the questionnaires were not included in the study.
Between January 2013 and April 2014, a total of 348 patients with complete follow-up were included (TR access: n=300, transfemoral [TF] access: n=48), as shown in Figure 1. Follow-up was incomplete or missing in 34 patients. Four of them died before one-year follow-up, seven patients refused further participation and 22 were non-responders because of incorrect contact information or no response at all, even after several phone calls. Before the study was initiated we performed a power calculation12. We extended inclusion for the ACRA study by two months to reach the minimum number of 285 analysable patients with TR access at one-year follow-up, assuming a higher non-responder rate at prolonged follow-up.
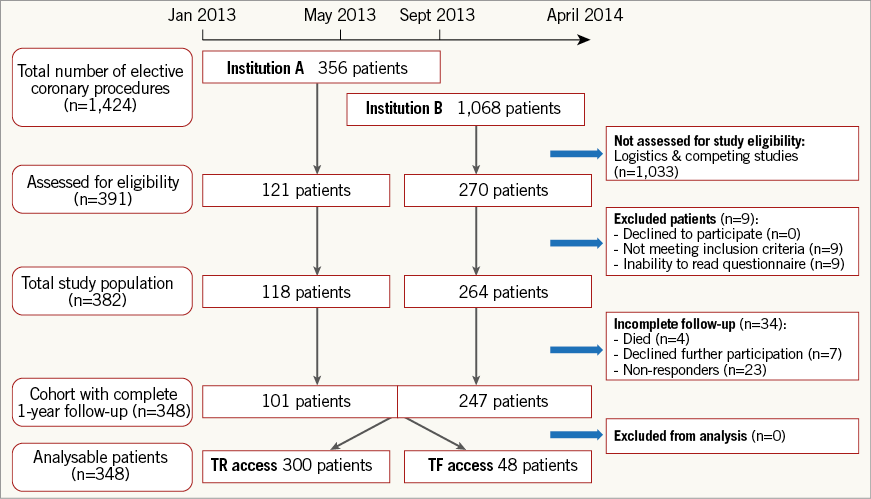
Figure 1. Enrolment flow chart. TF: transfemoral; TR: transradial
DATA
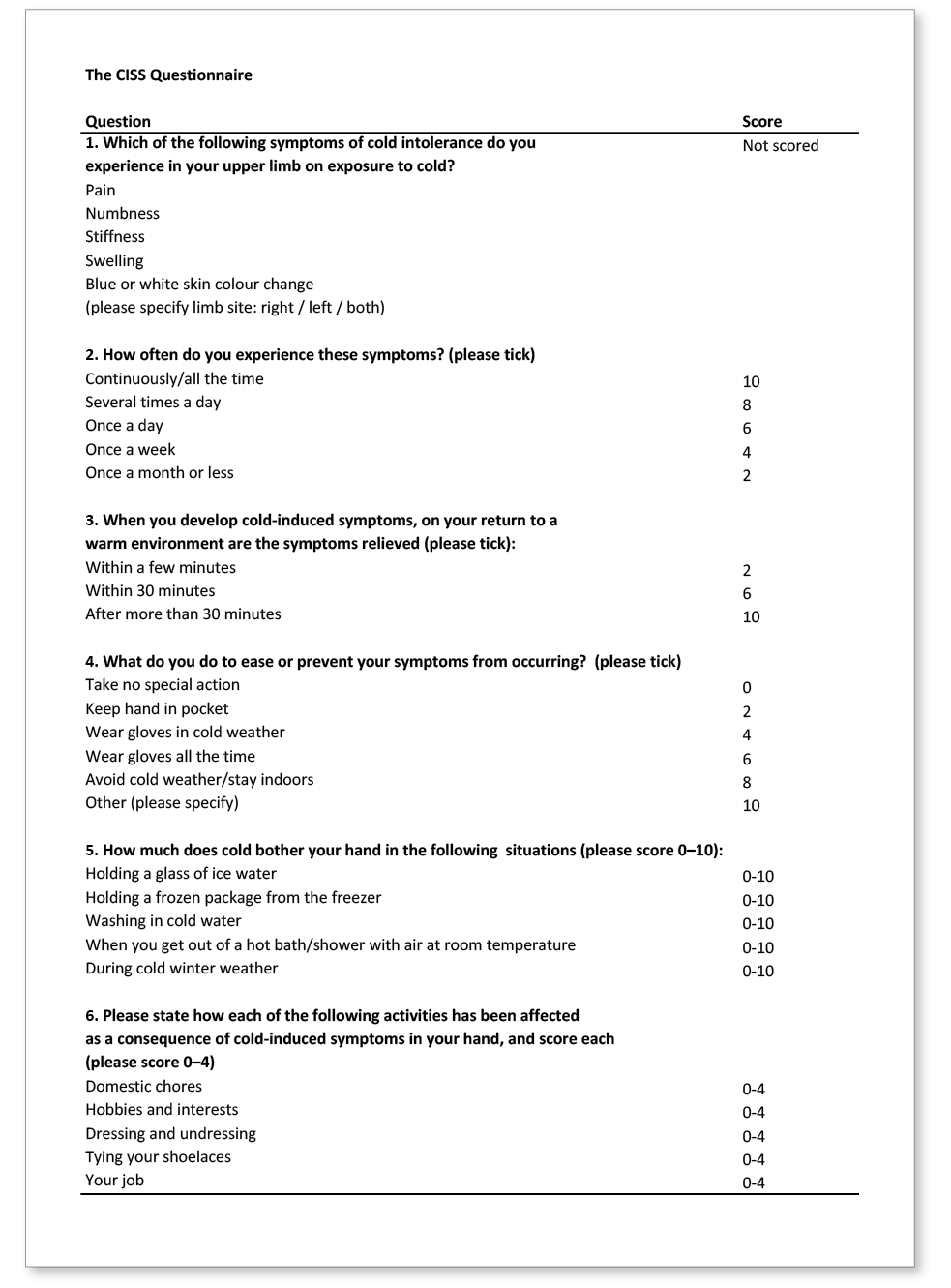
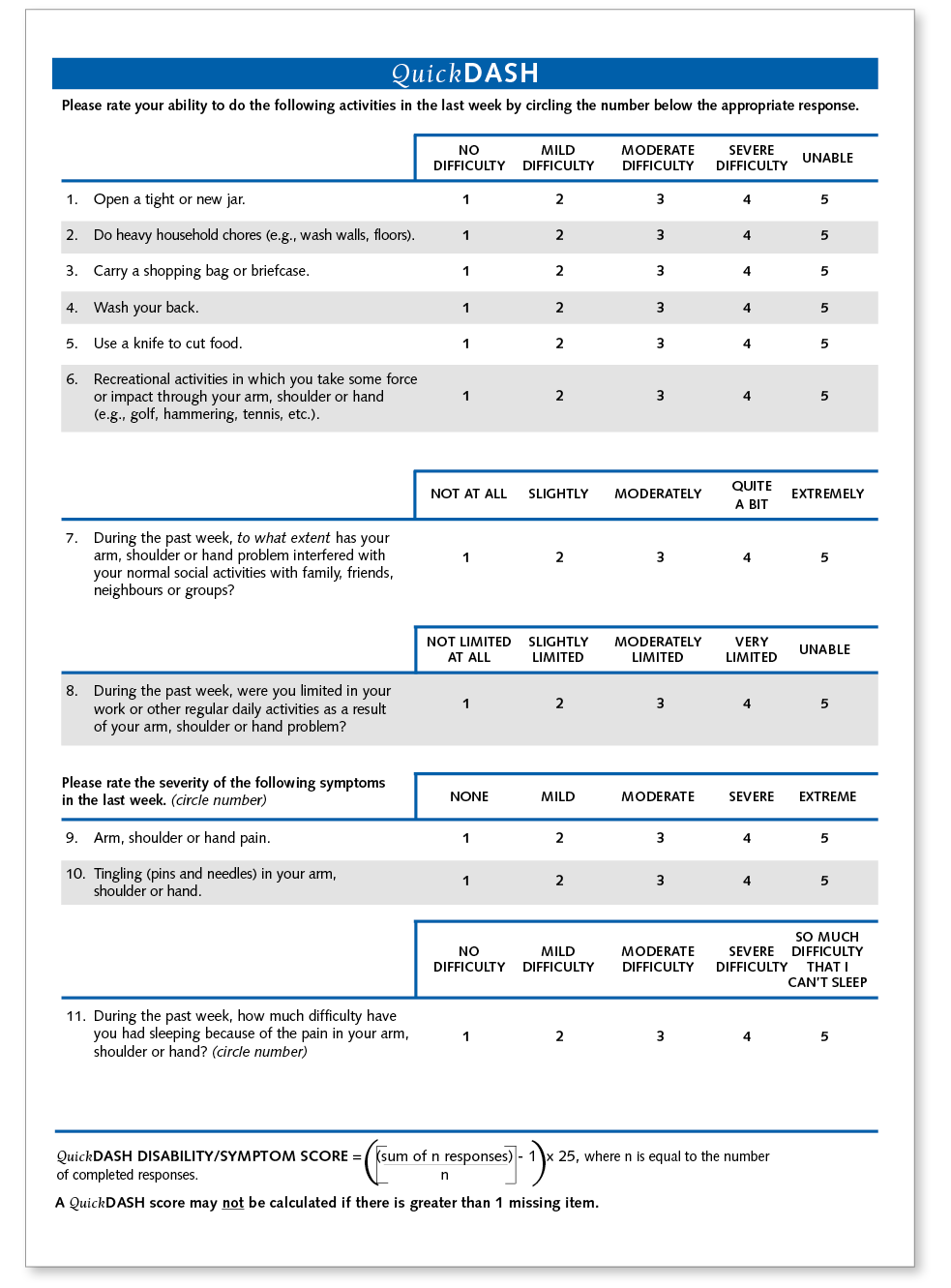
A dedicated electronic database was used to record the clinical and study-related parameters that have been previously described12. The QuickDASH is a shortened version of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire16, and was used to compare upper extremity functioning at baseline and follow-up, because it is completed more often and maintains its internal consistency/inter-rater reliability compared to the full version of the DASH17. The QuickDASH (Online Appendix 1) has been validated in a variety of conditions and in a normative population18. The minimal clinically important difference (MCID) that would correspond to a change in clinical status of upper extremity functioning varies between 819 and 1420 points. The Cold Intolerance Symptom Severity (CISS) questionnaire (Online Appendix 2) is a validated method to detect cold intolerance21 after a variety of upper extremity injuries, especially when neurovascular structures are involved22. Cold intolerance is defined as abnormal pain of the hand and fingers after exposure to cold that leads to significant functional impairment23.
ENDPOINTS
The change of upper extremity function from baseline to one-year follow-up was assessed with the QuickDASH score. A change in cold intolerance was assessed with the CISS score at baseline and one-year follow-up. The number of procedure-related extremity complaints during follow-up was compared between transradially and transfemorally treated patients.
STATISTICAL ANALYSIS
The Kolmogorov-Smirnov test was used to test the variables in our study sample for normality. The Wilcoxon signed-rank test was used to assess the change of upper extremity function (QuickDASH) and cold intolerance (CISS) over time, and the Mann-Whitney U test was used to compare these outcome parameters between patient groups (non-normally distributed continuous variables). Logistic regression analyses were applied to test the association between the access route and the development of cold intolerance or loss of upper extremity function. Logistic regression analyses were also used to test the association between vascular communication or patency and clinically relevant loss of upper extremity function or development of pathological cold intolerance. Non-normally distributed continuous variables are presented as median±interquartile range (IQR). Normally distributed continuous variables are presented as mean±standard deviation (SD) and categorical variables are expressed as percentages. Comparisons among clinical and procedural characteristics were performed using Pearson’s chi-square test for categorical variables and the independent samples t-test for continuous variables.
All statistical tests were two-tailed, and a p-value of <0.05 was considered statistically significant. All statistical analyses were performed with SPSS for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA).
Results
STUDY SAMPLE
Between January 2013 and April 2014, a total of 382 patients were prospectively enrolled. Complete one-year follow-up was achieved in 348 patients. TR access was applied in 300 patients and TF access in 48 patients (Figure 1). The mean age of the study sample was 64 years and 72% were male.
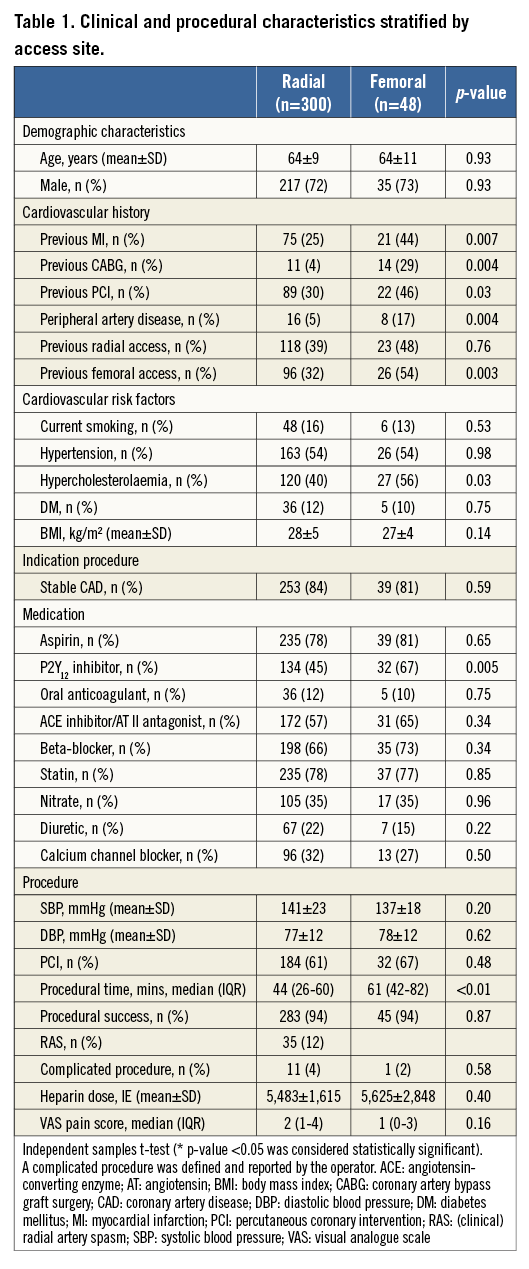
Clinical and procedural characteristics are presented in Table 1. A history of cardiovascular disease and hypercholesterolaemia was more prevalent in patients with femoral access as compared to patients with radial access. Transfemorally treated patients received a P2Y12 inhibitor at baseline more often than patients with TR access. Procedure times were longer in patients with TF access as compared to procedures with TR access. All other characteristics were the same between both access routes. Radial artery spasm was present in 12% of all TR procedures. Radial access failure occurred in five patients: three patients converted from the right RA to the left RA, one patient converted from the left RA to the right RA and one patient converted from the right RA to the right femoral artery (FA). Femoral access failure occurred in one patient who converted from the right FA to the left FA.
UPPER LIMB FUNCTION AND SYMPTOMS
Higher QuickDASH scores at baseline were present in females as compared to males (p<0.001), representing a worse upper extremity function. The median QuickDASH score was 2.27 for males and 9.09 for females (p<0.001). The QuickDASH scores at baseline were not different between both access groups (p-value 0.35).
The distribution and change of QuickDASH scores for both radial and femoral patients are shown in Figure 2. At one-year follow-up, QuickDASH scores were not statistically changed compared to pre-intervention when procedures were performed through the radial artery (baseline median: 2.39, follow-up median: 0.00; p-value 0.20) or the femoral artery (baseline median: 5.68, follow-up median: 4.55; p-value 0.63). QuickDASH scores at one-month follow-up were available for 344 patients with complete one-year follow-up. The QuickDASH scores at one month (median 2.27) and one-year follow-up were also not statistically different (p-value 0.65).
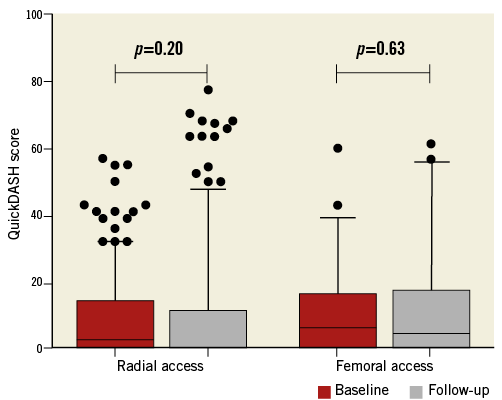
Figure 2. Upper limb function as assessed with the QuickDASH score over time. Box plots show the change of the QuickDASH score between baseline and one-year follow-up for TR- and TF-treated patients. Whiskers represent 5th-95th percentiles and p-values were calculated with the Wilcoxon signed-rank test (p-value <0.05 was considered statistically significant). A higher score for the QuickDASH indicates worse upper limb function or symptoms.
An increase in the QuickDASH score at one-year follow-up was present in 75 TR-treated patients (25.0%) and 15 TF-treated patients (31.3%). The type of access route was not associated with an increase of the QuickDASH score at one-year follow-up (OR 0.73, 95% CI: 0.39-1.42, p-value 0.36). A clinically relevant increase in the QuickDASH score at one year was similar in TR-treated patients (n=33, 11.0%) and TF-treated patients (n=6, 12.5%), considering a minimal clinically important difference of 14 (p=0.76).
Procedure-related extremity complaints were reported equally in both access groups during the first month, between one month and one year, and after one-year follow-up (Figure 3). The majority of patients did not report procedure-related extremity complaints (TR: 81%, TF: 79%). Extremity complaints diminished over time in both access groups, from 19% during the first month to 3% after one year (p<0.001), with pain as the most common persisting complaint (Figure 4). The amount of pain was quantified with the visual analogue scale (VAS) during the index procedure (Table 1) and before discharge, and was not different between both access groups (TR: 1, IQR: 0-2, TF: 1, IQR: 0-2.25; p-value 0.69).
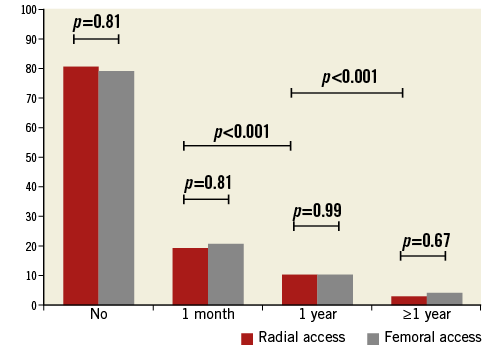
Figure 3. Procedure-related extremity complaints after TR and TF access (%).
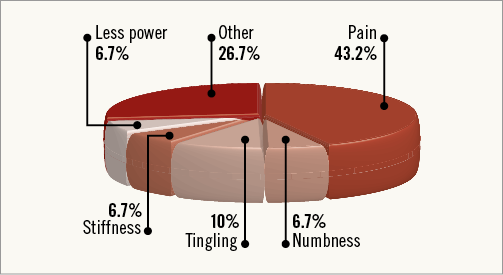
Figure 4. Types of procedure-related upper extremity complaints that persisted one year after transradial access (%).
At baseline, female patients had higher CISS scores as compared to men (8, IQR 0-27 vs. 0, IQR 0-11; p-value 0.001) and these were similar in both access groups (p-value 0.43). CISS scores did not change over time when the procedure was performed through the radial artery (p=0.09) or the femoral artery (p=0.29). The median CISS score for TR-treated patients was 0 (IQR 0-14) at baseline and 0 (IQR 0-0) at one-year follow-up. For TF-treated patients the median CISS score was 0 (IQR 0-31) at baseline and 0 (IQR 0-33) at follow-up. Pathological cold intolerance (defined as a CISS score ≥30) developed in 17 patients after TR access (6.3%), and in four patients after TF access (8.7%). The applied access route was not associated with the development of pathological cold intolerance (OR 0.70, 95% CI: 0.23-2.19; p-value 0.54).
An abnormal Allen test was present in 7.9%. A Barbeau type C response was present in 3.2% and a Barbeau type D response in 3.6%. Abnormal post-procedural patency of the radial artery was assessed with the reverse Barbeau test: type C was present in 3.2% and type D in 5.0%. Abnormal post-procedural vascular patency was not associated with the development of pathological cold intolerance (p-value 0.99) or loss of upper extremity function at one-year follow-up (p-value 0.45).
Discussion
To the best of our knowledge, this is the first study to investigate the consequences of TR access on upper extremity function at long-term follow-up. Most attention has been given to complications and complaints early after TR access. However, the primary goal of our study was to evaluate the potential change of upper extremity function at long-term follow-up.
We demonstrated that patients do not report a significant reduction of upper extremity function after TR access over time. The mean QuickDASH score as assessed pre-procedurally was not different to the score at one-year follow-up. Deterioration of upper limb function was reported by some patients after TR access. However, deterioration of upper limb function was equally reported in patients with TF access and of no clinical relevance in most instances20.
Acute injuries to the radial artery wall are frequently seen after TR catheterisation14 with intimal thickening and vascular dysfunction as a consequence24. Concerns about the functional consequences of these anatomic and physiologic changes that are induced by radial access may partly explain the infrequent adoption of TR PCI in certain parts of the world, such as the USA and the Middle East25,26. However, these injuries do not affect post-procedural radial patency and self-reported functional impairment at one-month follow-up27. Recent studies also show that hand grip strength is not reduced after TR access28, including those patients with RAO29. Based on previous reports and the one-month results from the ACRA study12, the outcomes of the current study support the concept that upper extremity function is unaffected after TR catheterisation.
Several tests and questionnaires have been developed to assess upper extremity disability30-32, incorporating assessment at the level of body functions and structures, activities and participation. Careful selection of a specific method to determine general hand function is crucial to evaluate the consequences of a specific procedure or disease. This requires the use of reliable and validated instruments to evaluate changes. Furthermore, the setting and context of the study may help to determine which test or questionnaire should be used, considering the potential functional problems after a specific intervention (i.e., sensibility, strength, pain or mobility). Questionnaires such as the SF-3633 are too generic to evaluate upper extremity function after TR procedures, because they are less sensitive to clinical change in patients with problems in a specific anatomic region. We used the QuickDASH score as outcome measure, because it is a validated outcome measure to monitor upper extremity disability over time for both clinical and research purposes. The QuickDASH score has a good test-retest reliability and is a reliable tool to monitor upper extremity function over time in a normative population18 and in patients with a variable number of upper extremity conditions17. QuickDASH scores in our study sample were comparable to those in the general population34, with significantly higher scores in females18,35. Evaluation of upper extremity function is complex, and the timing of measurements may have a significant impact on outcome. For example, in the early phase after TR access, functional impairment will be present in most instances because of haematoma, oedema or discomfort at the access site. In our study group, most procedure-related extremity complaints were reported within the first month and decreased over time, which supports this concept.
Cold intolerance was also evaluated because as many as 85% of patients with injuries to the upper extremity (including injection/puncture) complain of some degree of cold sensitivity13. At one-month follow-up, no increase of cold intolerance could be observed after TR access, as determined with the validated CISS score36. However, the evaluation of cold intolerance at the first month might be too soon because it peaks at three months and remains constant thereafter13. The present study showed that at one-year follow-up CISS scores and the prevalence of pathological cold intolerance were unchanged after TR procedures or TF procedures (as a reference group).
Finally, it is recommended to perform the Allen test or Barbeau test before each TR procedure to evaluate the patency of the palmary arch37. However, both tests are not routinely used before TR procedures2 and do not predict ischaemic complications. In a recent paper, patients with an abnormal Allen test did not show clinical or subclinical signs of hand ischaemia around TR catheterisation28. In this study, we did not observe an association between an abnormal Allen or Barbeau test and the occurrence of upper extremity disability. Also, no association was present between abnormal RA patency and upper extremity disability or cold intolerance. Our study supports the results of the recently published Hangar study, i.e., that hand strength (as part of upper extremity function) was unchanged after RAO29.
Limitations
The paired design of this multicentre prospective study made it less prone to bias with respect to the similarity of external variables. However, response bias may have affected our study results38. Abnormal vascular patency of the RA might have been miscalculated because it was not confirmed with echo-duplex. This study was not powered to evaluate the functional consequences of RAO or specific patient groups (such as females with small RA, etc.). However, it gives a global impression of the functional consequences of upper extremity function after elective TR procedures.
Conclusions
Our study demonstrated that self-reported upper limb function at long-term follow-up was not jeopardised when coronary catheterisations and interventions were performed through the radial artery.
| Impact on daily practice Our study demonstrated that upper extremity function was not affected by TR access during long-term follow-up. The results are important to inform patients adequately about the functional consequences of TR access and may dispel part of the anecdotal fear, especially when optimal upper extremity function is essential. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
SUPPLEMENTARY DATA
Appendix 1. The QuickDASH questionnaire
Appendix 2. The CISS questionnaire