Abstract
Aims: Lower limb angioplasty is usually performed by transfemoral access despite the risk of local complications. Transradial access (TRA) has gained acceptance for coronary interventions. The aim of this study was to evaluate the feasibility and safety of TRA for above the knee (ATK) angioplasty.
Methods and results: Twenty-five consecutive patients (eight females; mean age 72, range 55-85 years; seven symptomatic for critical limb ischaemia, 18 for claudication) underwent ATK angioplasty by left (19) or right (6) TRA. A total of 32 lesions were addressed; 16 stents were positioned in 12 patients with an overall success rate of 81%, and a success rate of 38% on occlusions and of 96% on stenoses. The overall success rate on the 16 supra-inguinal lesions was 81%, (success rate 60% on occlusions and 91% on stenoses). The overall success rate on the 16 infra-inguinal lesions was 81%, (success rate 0% on occlusions and 100% on stenoses). Any haemorrhagic complications or local complications needing surgery were observed in the cohort of patients.
Conclusions: TRA can represent a feasible and safe alternative for ATK angioplasty in case of difficult femoral access.
Introduction
Percutaneous angioplasty is frequently performed for the treatment of symptomatic peripheral arterial disease, and the common femoral artery is the access of choice1.
Stenoses or occlusions in above the knee (ATK) arteries can be treated via transfemoral access by retrograde ipsilateral approach or by the cross-over technique. However, the retrograde ipsilateral approach encounters the problem of cannulating a hypoperfused femoral artery while with the cross-over technique it can sometimes be difficult to cross the aortic bifurcation, especially in patients with very acute aortic bifurcation and calcific vessels. Both femoral artery access techniques retain a substantial risk of local complications, which persist despite the increasing use of closure devices2. With the retrograde ipsilateral femoral access, only lesions of the same-side supra-inguinal tract can be treated. With the cross-over technique, ipsilateral and contralateral lesions of the supra-inguinal tract and contralateral lesions of the infra-inguinal tract can be treated in the same session.
Transradial access (TRA) enjoys more popularity from interventional cardiologists for percutaneous coronary interventions, since it is associated with similar results in target lesions, but less haemorrhagic complications, and lower morbidity and mortality3,4. TRA for lower limb angioplasty could theoretically offer several advantages. First, femoral arteries of patients scheduled for lower limb angioplasty are often involved in the atherosclerotic process and TRA avoids their puncture and compression after the procedure. Second, TRA avoids the local haemorrhagic complications associated with the femoral access, as demonstrated by studies in percutaneous coronary interventions5. Lastly, TRA allows addressing ATK lesions of both legs during the same session, avoiding a second arterial puncture.
Until now, percutaneous interventions on lower limb arteries by TRA have been limited by the inadequate length of devices. Recently, balloons and stents with long shafts have become available and lower limb interventions can be done also by TRA.
In our institution, TRA is routinely used for percutaneous coronary interventions. Therefore, we decided to evaluate the feasibility and safety of ATK angioplasty by TRA (Figure 1).
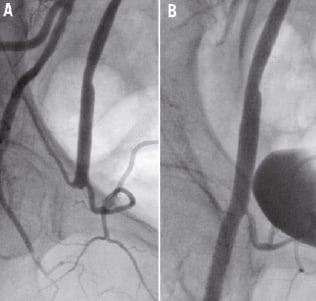
Figure 1. Occlusion of a right common femoral artery successfully treated by TRA with dilatation and stenting. The patient had an occlusion device positioned in common femoral artery two months before. A) Before treatment. B) After treatment.
Methods
Patient population
Starting May 1, 2010, a series of 25 consecutive patients scheduled for ATK angioplasty were proposed for TRA. All the patients had been informed of the experimental nature of this study and signed a written, informed consent.
Patients were selected on the basis of their symptoms, both in the form of claudication or critical limb ischaemia (rest pain and/or tissue loss), and in the presence of echo colour Doppler and/or CT angiography evidence of stenoses or occlusions in arterial segments deemed to justify the symptoms. Symptoms were rated according with the Rutherford classification6.
All the patients were pre-treated, starting at least one day prior to the procedure, with a single dose of 300 mg of clopidogrel and 300 mg of aspirin. Double antiplatelet therapy was continued at least for one month after the procedure, with 75 mg of clopidogrel and 100 mg of aspirin, both once daily7. Single antiplatelet therapy with 100 mg of aspirin was advised lifelong.
Technique of ATK angioplasty
Cannulation of the radial artery was performed using standard procedure, with an 11 cm long, 6 Fr, radial introducer (Avantix; Cordis Corporation, Bridgewater, NJ, USA)3. After cannulation, 5.000 IU of heparin, 2.5 mg of verapamil, and 1 mg of nitroglycerine were injected into the radial introducer. During the procedure heparin was re-injected as appropriate to maintain the ACT between 200 and 250 sec.
Wiring of the descending aorta was obtained in the 35° left anterior oblique projection, by a 260 cm long, 0.035 inch, hydrophilic wire (Terumo Corporation, Tokyo, Japan) directly or with the aid of a curved, 4 Fr, coronary diagnostic catheter (Judkins left, Judkins right, internal mammary; Cordis Corporation, Bridgewater, NJ, USA).
Cannulation of the common iliac arteries for angioplasty was obtained by a 125 cm long, 6 Fr Multipurpose guiding catheter (Cordis Corporation, Bridgewater, NJ, USA) inserted within the radial introducer, or by a 120 cm long, 5 Fr introducer (Epsylar; OptiMed, Ettlingen, Germany) exchanged for the radial introducer.
Lesions were crossed using 300 cm long wires with a pre-mounted 0.018 In, over-the-wire balloon with a 180 cm long shaft (Pacific Extreme; Invatec, Brescia, Italy) that were subsequently used to dilate the lesions. We used 0.014 in wires (Pilot 200, Abbott Vascular, Redwood City, CA, USA; PT Graphix, Boston Scientific, Natick, MA, USA; Miracle 6 or 12, Asahi Intecc, Aichi, Japan) or 0.018 in wires (V18 [Boston Scientific, Natick, MA, USA; Treasure 12 or Astato 30, Asahi Intecc, Aichi, Japan). After having crossed the lesion, the position was maintained by a 0.018 in, soft tip, 400 cm long wire (Plywire; OptiMed, Ettlingen, Germany) exchanged for the previous wires by advancing the balloon beyond the lesion. Dilatations of the lesions were performed using 0.018 in, over-the-wire balloons with a 180 cm long shaft (Pacific Extreme; Invatec, Brescia, Italia). Stenting was done by an 0.018 inch compatible, self-expanding nitinol stents with a 180 cm long shaft (OptiMed, Ettlingen, Germany).
After the completion of the procedure, the introducer was immediately removed and haemostasis was obtained with a dedicated device (TR Band; Terumo Corporation, Tokyo, Japan).
Four weeks after the procedure, all the patients underwent a follow-up visit to re-evaluate the symptoms of peripheral arterial disease and evaluate the patency of the radial artery. Clinical successful was defined, as suggested in “recommended standards for reports dealing with lower extremity ischaemia”6.
Feasibility endpoints were:
– possibility to reach and address the lesion to be treated;
– angiographic success defined as less than 30% residual stenosis in the culprit lesions;
– clinical success defined as at least one Rutherford category improvement at four week follow-up visit.
Safety endpoints were:
– major and minor haemorrhagic complications defined according to the TIMI bleeding classification8;
– any surgical intervention to correct a local vascular complication.
Results
Demographic and clinical characteristics of patients are shown in Table 1. In summary, mean age of patients was 72 years, range 55-85 years; eight patients were females; seven patients were symptomatic for critical limb ischemia, 18 for claudication; 12 patients had diabetes mellitus; eight patients had chronic renal failure and two of them were on haemodialysis; seven patients were current smokers.
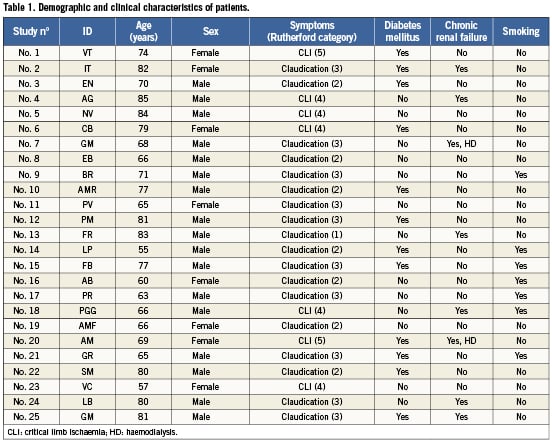
Individual angiographic characteristics and results are shown in Table 2. Six patients (24%) were approached by right TRA due to a small left radial artery, the remaining from left TRA; one patient, No. 16, AB, was initially addressed by left TRA but she was then crossed-over to right TRA due to a spasm of her small radial artery, originating from a high-bifurcating brachial artery. Direct wiring of the descending aorta was possible in 15 patients (60%); in all the others, descending aorta was reached by the aid of a curved-tip coronary diagnostic catheter.
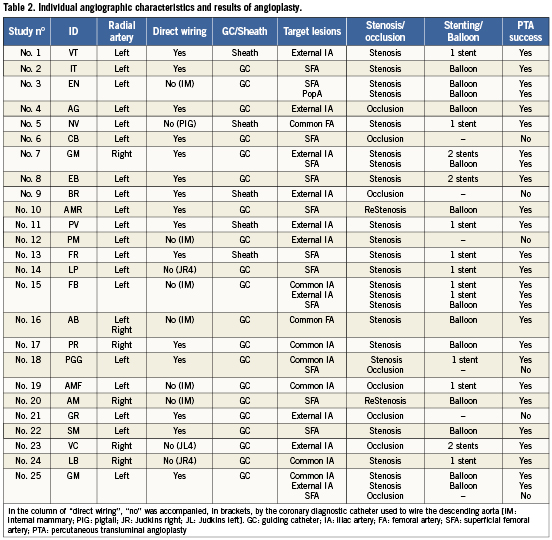
All the target lesions could be reached with a wire in all patients.
There were six unsuccessful angioplasties, five were occlusions that were not crossed by the wire, and one was a stenosis that was crossed by a 0.014 inch wire but not by any balloon.
Angiographic success rates are shown in Table 3.
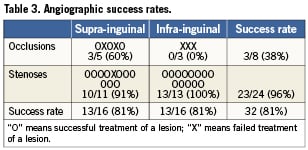
A total of 32 lesions were addressed; 16 stents were positioned in 12 patients with an overall success rate of 81%, and a success rate of 38% on occlusions and of 96% on stenoses.
The lesions addressed in the supra-inguinal tract were 16 of which five were occlusions; all of them were de novo lesions. The overall success rate on the supra-inguinal lesions was 81%, with a success rate of 60% on occlusions and of 91% on stenoses.
The lesions approached in the infra-inguinal tract were 16 of which three were occlusions and two were intra-stent restenosis. The overall success rate on the infra-inguinal lesions was 81%, with a success rate of 0% on occlusions and of 100% on stenoses.
Any haemorrhagic complications or local complications needing surgery were observed in the entire cohort of patients.
At the follow-up visit, 21/25 patients had clinical improvement, i.e., at least one Rutherford category improvement, with an overall clinical success rate of 84%.
One patient (4%) presented with an asymptomatic occlusion of the radial artery.
Discussion
Our study demonstrated that TRA is a feasible and safe access for treating lesions on arteries of lower limbs, at least for the whole ATK tract. We were able to address all the lesions we planned. Moreover, we had no local complications while for similar interventions bleeding complications have been reported to occur in up to 7% of patients treated by transfemoral approach, and 2% of those required surgery9,10.
To our knowledge, no operator uses the radial artery as the first line vascular access to treat lesions on lower limb arteries.
In 2005 Flachskampf et al11 first reported the successful treatment of a common iliac artery stenosis employing TRA.
In 2008 Sanghvi et al12 reported a selection of 15 patients From their database in whom lesions of the iliac artery or the superficial femoral artery stenosis were treated using TRA due to “severe, bilateral iliac artery disease, absent femoral pulses, morbid obesity and/or conditions prohibiting prolonged bed rest”. They successfully treated 14/15 patients with a success rate that was higher than our study (93% versus 81%). However, their paper is limited due to missing a detailed angiographic analysis with the percentage of total occlusions. also reporting no episodes of local complications.
In 2009 Trani et al13 reported a retrospective series of 12 patients with in-stent restenosis of the superficial femoral artery treated with plain balloon angioplasty by TRA, matched with 12 patients treated by transfemoral access. They had, by TRA, the same, 100% success rate as transfemoral access, but using 30% less amount of contrast media. They had no local complications in both groups. Our study had a 100% success rate in the treatment of in-stent restenosis of the superficial femoral artery, although we treated only two patients.
In 2010 Staniloae et al14 published a retrospective series of aorto-iliac interventions in 68 patients, of whom 27 (33 lesions) were treated by TRA and 41 (47 lesions) by transfemoral access. In the group treated by TRA they had a success rate similar to our study with supra-inguinal lesions (87.9% versus 81%). Notably, they reported a 7.3% access-site complications in patients treated by transfemoral access but no complications in those treated by TRA. Patients treated by TRA had also a 31% shorter time to discharge.
Our study is the first study that prospectively evaluated the feasibility and safety of TRA to treat all-comer patients with all spectrums of ATK lesions.
A deeper analysis of our data suggests that supra-inguinal stenoses can be addressed and treated safely by TRA. In fact, stents with 180 cm long shafts that can progress within a 6 Fr guiding catheter or a 5 Fr sheath are now available in 8, 9 and 10 mm diameters (sinus-SuperFlex-518; OptiMed, Ettlingen, Germany) and can be used to treat lesions in common and external iliac arteries. Occlusions of supra-inguinal tracts can also be treated by TRA and the successful rate of our series is encouraging. In fact, our 60% success rate is very close to the 56% success rate that Staniloae et al14 had in a comparable cohort of patients.
Also SFA lesions can be approached safely by TRA. In particular, de novo stenosis on SFA can be treated safely as stents of adequate diameters (6, 7 and 8 mm: sinus-SuperFlex-518; OptiMed, Ettlingen, Germany) are now available in long shafts to cover flow-limiting dissections after dilatation with balloons. TRA can become the approach of choice for treating intra-stent restenosis. In fact a 100% success rate on this kind of lesions has been obtained in our series as in the series reported by Trani et al13. On the contrary, the successful rate of the treatment of chronic occlusions of SFA in our study was disappointing. By TRA, only 0.018 inch wires can be used and, to support the progression of the wires, only the 0.018 inch balloons are available. Therefore, our results seem to suggest that the current armamentarium is inadequate to address occluded SFAs.
Interventions on arteries in lower limbs by TRA can offer several advantages. First, TRA avoids puncturing usually diseased femoral arteries of these patients and avoids groin compression after the procedure that can precipitate ischaemia or thrombosis. Second, TRA avoids the local haemorrhagic complications that can be associated with femoral artery puncture. Lastly, employing TRA, lesions in arteries of both legs can be treated during the same session.
In the past, trans-brachial access has been used for angioplasty in the lower extremities in case of a difficult transfemoral access15. However, although this conduit can solve the length limitations of TRA, it retains the same risk of local complications in transfemoral access16.
In conclusion, TRA can be considered the alternative to transfemoral access to address lesions on ATK arteries. In the future, randomised studies could be planned to compare the efficacy/safety ratio of TRA versus transfemoral access for ATK angioplasty.
Acknowledgements
Many thanks to Miss Elena Fontana for having revised the manuscript.
Many thanks to our nurses: Mrs. Alessandra Matteucci, Mrs. Elisabetta Motroni, Mrs. Luciana Giampaoli, Mrs. Agnese Micheletti, and Mrs. Barbara Corrieri. Many thanks to our RX technicians: Mrs. Valeriana Marcheschi, Miss Francesca Morgantini, Miss Elisa Nieri, Mr. Roberto Dondoni, Mr. Giorgio Cipollaro, and Mr. “the professor” Michele Fruzzetti.
Without their daily, precious help this paper could not have been written.
Conflict of interest statement
The authors have no conflict of interest to declare.

