A 59-year old male with a history of controlled hyperlipidaemia, hypertension and diabetes mellitus presented with a recurrence of angina pectoris. Previously, in August 2000, two overlapping 4 mm by 12 mm Igaki-Tamai® stents (Kyoto Medical Planning Co. Ltd, Kyoto, Japan) had been implanted in his proximal right coronary artery (RCA) (Figure 1), and in December 2000 he had two 4 mm by 8 mm Bx VELOCITY® (Cordis, Warren, NJ, USA) bare metal stents deployed into the distal RCA (Figure 2). In 2009, a multislice CT coronary angiogram (Figure 3A) was performed to investigate his recurrent symptoms, following which he underwent coronary angiography (Figure 3B). Intravascular ultrasound (Figure 4) and optical coherent tomography (Figure 5) demonstrated a widely patent coronary artery at the segment with prior biodegradable stents. Angiography demonstrated a distal RCA lesion that was not significant on fractional flow reserve assessment (0.85), and a significant lesion in the left anterior descending artery, which was successfully treated.
Figure 1. Coronary angiography of the right coronary artery during the index PCI (August 2000). (A) The index lesion. (B) The Igaki-Tamai stent is across the index lesion, and is identified by its two radio-opaque cylindrical gold markers (0.6 mm high by 0.18 mm in diameter) situated at either end of the stent (sm). The stent was mounted on a conventional angioplasty balloon, which had two standard balloon markers (bm). The stent required an 8 Fr guiding catheter because it was initially enclosed within a covered sheath that was removed once it was across the lesion. The distal tip of the covered sheath (cs) is visible just distal to the tip of the guide catheter. (C) The four markers of the two overlapping Igaki-Tamai stents. (D) The final angiographic result.
Figure 2. (A) Coronary angiography of the right coronary artery at four-months follow-up. The Igaki-Tamai stent markers (sm) are visible, and there is no angiographic evidence of restenosis. A new lesion has developed in the distal RCA (L) that was successfully treated with two bare metal stents. (B) Coronary angiography of the right coronary artery at twelve-month follow-up. The Igaki-Tamai stents identified by the stent markers (sm), and the bare metal stents (Bx) are all patent.
Figure 3. Multislice CT (MSCT) coronary angiography of the right coronary artery (RCA) nine years after the index PCI. (A) The proximal segment of the RCA previously stented with Igaki-Tamai stents was recognised on MSCT by the presence of gold stent markers (sm). In the distal RCA, the Bx VELOCITY stent struts (Bx) are clearly seen, but the luminal area cannot be appreciated because of blooming artefact. Calcium deposits (cd) are noted in the proximal and distal vessel, and furthermore a lesion (l) appears to be present. (B) The cross-sectional luminal area in the stented segment (yellow bar in panel A) was measurable by MSCT (9.4 mm2). (C) Coronary angiogram of the RCA, nine years following the index procedure. The Igaki-Tamai stent markers (sm) are clearly visible in the proximal vessel. The stents are patent and appearance are unchanged from the previous angiogram in 2001 (Figure 2B). The lesion (l) in the distal vessel was not significant on functional assessment.
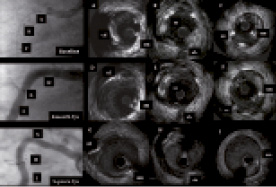
Figure 4. Intravascular ultrasound (IVUS) images from the stented right coronary artery. (A-C) Baseline IVUS images (August 2000) taken using a Boston Scientific UltracrossTM 30MHz IVUS catheter (Boston Scientific, Natick, MA, USA), and the corresponding angiogram. The stent markers (sm) are shown, together with stent struts (ss), which were 0.17mm thick at baseline (A and C). At the side branch (sb, panel B), four struts are visible located at 2, 9, 10, and 11 o’clock. Quantitative analysis showed that the mean luminal area and mean vessel area in the stented segment was 13.06 mm2, and 27.59 mm2 respectively. (D-F) IVUS images at four-months follow-up. The stent markers (sm), stent struts (ss), and a calcium deposit (cd) are all seen. Four stent struts are still visible at the side branch (B). Mean luminal area and mean vessel area were 14.00 mm2 and 31.68 mm2 respectively. (D-F) IVUS images at 9-year follow-up. The stent markers (sm) and calcium deposit (cd) are still visible 9 years after the procedure. Struts are not visible, although some high-echogenic signals may represent the remnants of some struts (10-11 o’clock at the side branch, panel H). On IVUS analysis, the mean luminal area, and mean vessel area are similar to the results at 4-month follow-up (13.7 mm2 and 26.7 mm2 respectively).
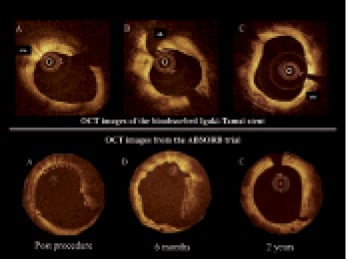
Figure 5. Top panel, A-C: Images from optical coherence tomography (OCT) at 9-year follow-up, of the Igaki-Tamai stent. The stent markers (sm) are visible on OCT (the proximal marker: A, the Distal marker: C), whilst the struts are not. The endoluminal lining of the vessel is circular and smooth. Bottom panel, A-C: As a comparison to what the Igaki-Tamai stents may have looked like when they were initially implanted, OCT images of the BVS bioabsorbable stent at baseline, six months and two years follow-up.2 (A) At baseline, the struts have a preserved box appearance. (B) At six months, the luminal surface is irregular and some struts have an open box appearance (10-11 o’clock), while some have a dissolved bright box appearance (12 o’clock). (C) At two years, the endoluminal lining is smooth and circular with some apparent struts.
The Igaki-Tamai stent was the first fully biodegradable coronary stent (BDS) to be implanted in humans; full degradation taking 18-24 months. It had a helical zig-zag design, and was composed of a poly-l-lactic acid (PLLA) coil that expanded to its original size when heated. The stent was deployed by inflating the delivery balloon to 6-14 atm for 30 seconds using contrast heated to 80°C.
The first-in-man study of the Igaki-Tamai stent (15 patients, 19 lesions, 25 stents), demonstrated no major adverse cardiovascular events (MACE) or stent thrombosis within 30-days, and only one repeat PCI at 6-months follow-up. Intravascular ultrasound (IVUS) demonstrated no significant stent recoil at day one, and as expected from the properties of PLLA continued stent expansion was observed with follow-up.1
In a larger study of 50 elective patients, IVUS demonstrated the complete absence of stent struts at 3-years follow-up, whilst angiographic analysis indicated a mean diameter stenosis of 25%; which compares well with the 27% diameter stenosis observed at two years follow-up in the ABSORB study.2 Clinical outcomes at 4-year follow-up, showed rates of overall survival, MACE free survival, and target vessel revascularisation (TLR) of 97.7%, 82.0%, and 18% respectively. One patient experienced a stent thrombosis (at day five, due to inadequate heparinisation at time of PCI).3
The arrival of drug eluting stents (DES) moved attention away from BDS, despite the promising results of initial studies of the Igaki-Tamai stent. Recently, interest has resurfaced, following the safety concerns with DES. The ability of BDS to initially prevent acute recoil, and then be fully absorbed once healing has taken place, without leaving any struts behind, may offer the definitive solution to these safety issues. The recent two-year results of the ABSORB study of the BVS everolimus eluting PLLA stent (ABBOTT Vascular, Santa Clara, CA, USA) has shown very promising results with no cardiac deaths, ischaemia-driven TLR or stent thromboses recorded. There was no angiographic evidence of restenosis, and only one myocardial infarction (non-Q wave). IVUS and optical coherency tomography demonstrated partial stent bioabsorption, and an increase in luminal area secondary to a reduction in plaque size. Finally, the restoration of vasomotion was demonstrated.2
This case is the longest available follow-up of a BDS demonstrating that their initial promising results are maintained at long-term follow-up. In particular, there was complete absorption of stent struts, no restenosis, and preservation of vessel vasomotion. BDS are worthy of the accolade of being ‘the fourth revolution’ in interventional cardiology, which is a fitting tribute and legacy to Hideo Tamai, the inventor of the Igaki-Tamai stent, who died on 10th February 2009.