Abstract
Aims: Few data are available on outcomes of percutaneous coronary intervention (PCI) for coronary chronic total occlusions (CTO) in very elderly patients in the drug-eluting stent (DES) era. We aimed to investigate long-term survival in a single-centre cohort of elderly patients afollowing CTO PCI using DES.
Methods and results: A total of 2,002 consecutive patients who underwent PCI of a CTO at our centre between January 2005 and December 2013 were followed for a median of 2.6 years (interquartile range 1.1-3.1 years). Four hundred and nine (409) patients were older than 75 years. The absolute reduction in all-cause mortality by successful CTO PCI was numerically greater in elderly patients as compared to younger patients (22.1% vs. 7.2% at three years). In multivariate models, successful CTO PCI was significantly associated with improved survival in both elderly (adjusted hazard ratio [HR] 0.58, 95% confidence interval [CI]: 0.39 to 0.87; p=0.009) and younger patients (adjusted HR 0.59, 95% CI: 0.40 to 0.86; p=0.006).
Conclusions: In the DES era, elderly patients (≥75 years) derive a similar survival benefit from successful CTO PCI to younger patients. These findings suggest that CTO PCI, when indicated, should not be withheld from the elderly.
Abbreviations
CABG: coronary artery bypass graft
CI: confidence interval
CTO: chronic total occlusion
DES: drug-eluting stent
eGFR: estimated glomerular filtration rate
HR: hazard ratio
MI: myocardial infarction
PCI: percutaneous coronary intervention
TIMI: Thrombolysis In Myocardial Infarction
Introduction
Percutaneous management of coronary chronic total occlusions (CTO) is a rapidly evolving field and the prevalence of CTO is highest in elderly individuals1. Despite growing evidence suggesting that revascularisation is associated with improved survival in elderly patients, this population is less likely to undergo attempted CTO revascularisation as compared to younger patients2. The high prevalence of comorbidities and frailty, and the wide variation of risk, together with higher complication rates and poorer procedural success rates, may render the decision to perform CTO percutaneous coronary intervention (PCI) in aged individuals challenging.
Although more extensive coronary artery disease (CAD) and ischaemic burden are frequently encountered in the elderly, and notwithstanding the fact that this population may greatly benefit from coronary revascularisation, most clinical trials exclude older patients above the age of 753,4. Indeed, more than 50% of the CAD trials did not enrol any patients over the age of 755. Several studies have demonstrated that successful CTO PCI significantly improves cardiac function and survival in younger and middle-aged persons6-9. However, data in an elderly patient population are lacking. Thus, given the limited available data on CTO PCI in aged individuals in addition to the rapid evolution of PCI techniques as well as the improvement of PCI outcomes in the elderly, the current study was designed to compare the long-term survival benefit of successful CTO PCI in elderly patients with that of younger patients.
Methods
PATIENT SELECTION AND FOLLOW-UP
As part of the quality management programme at our institution, we maintain a database of demographics, angiographic and procedural data as well as in-hospital and long-term outcome data of all patients undergoing PCI in our catheterisation laboratory. Consecutive patients who underwent elective PCI of at least one CTO between January 2005 and December 2013 at our centre were included in this study. The indication for PCI of the CTO was the presence of symptomatic angina, and/or at least one of the following – presence of viable myocardium on cardiac magnetic resonance imaging, or inducible ischaemia either on stress echocardiography or myocardial perfusion scan.
Patients were followed prospectively by telephone interview at 30 days, one year and three years after PCI in the present study. In addition, follow-up data were obtained from hospital re-admission records, telephone contact with the referring physician or outpatient visits.
STUDY ENDPOINTS AND DEFINITIONS
A CTO was defined as angiographic evidence of Thrombolysis In Myocardial Infarction (TIMI) flow grade 0 within an occluded arterial segment of more than three months duration. In the absence of previous angiographic documentation, the duration of the occlusion was estimated clinically, based on the onset of symptoms or timing of myocardial infarction (MI) in the CTO-related artery. Successful CTO PCI was defined as recanalisation of the lesion with residual stenosis <30% and TIMI flow grade 3. After PCI, all patients were prescribed lifelong aspirin in addition to clopidogrel for at least six months after drug-eluting stent (DES) implantation.
The primary endpoint was all-cause mortality. The secondary endpoint was the cumulative incidence of major adverse cardiovascular events (MACE), defined as the composite of all-cause death, non-fatal myocardial infarction, and target vessel revascularisation (TVR) including PCI and CABG. For in-hospital events, the MACE definition has been previously published in detail
STATISTICAL ANALYSIS
For the purposes of the current analysis, we defined patients aged ≥75 years as elderly. Continuous variables are presented as mean±standard deviation (SD), or as median (interquartile range). Categorical variables are presented as frequencies (percentages). The Kolmogorov-Smirnov test was used to test for normality of distribution. Continuous variables were compared with the unpaired Student’s t-test or the Mann-Whitney U test, and categorical variables with Pearson’s χ² test or Fisher’s exact test, as appropriate. We derived hazard ratios (HR) with associated 95% confidence intervals (CI) from univariable and multivariable Cox proportional hazards models. Apart from CTO PCI success/failure, we selected baseline variables that showed a significant association with CTO PCI success as independent variables for the multivariable Cox models. As published previously, the selected variables were: diabetes, hypertension, estimated glomerular filtration rate, prior myocardial infarction, prior CABG, left ventricular ejection fraction <40%, multivessel disease and moderate/severe calcifications9. A Cox proportional hazards regression test of interaction (elderly/younger status by procedural success/failure status) was performed to elucidate potential differences between elderly and younger patients in terms of the effects of procedural success on the outcome measures. Kaplan-Meier survival curves and the log-rank test were used to provide comparisons among groups. A two-sided p-value of <0.05 was considered statistically significant. For the statistical analyses, SPSS software package, Version 18 (SPSS Inc., Chicago, IL, USA), was used.
Results
STUDY POPULATION AND PROCEDURAL OUTCOME
A total of 409 (20%) patients were aged ≥75 years and were at higher baseline risk (Table 1). Elderly patients were more frequently male (<0.001), had a higher prevalence of comorbidities including hypertension (<0.001) and chronic kidney disease (<0.001), and more frequently had left ventricular systolic dysfunction (0.02).
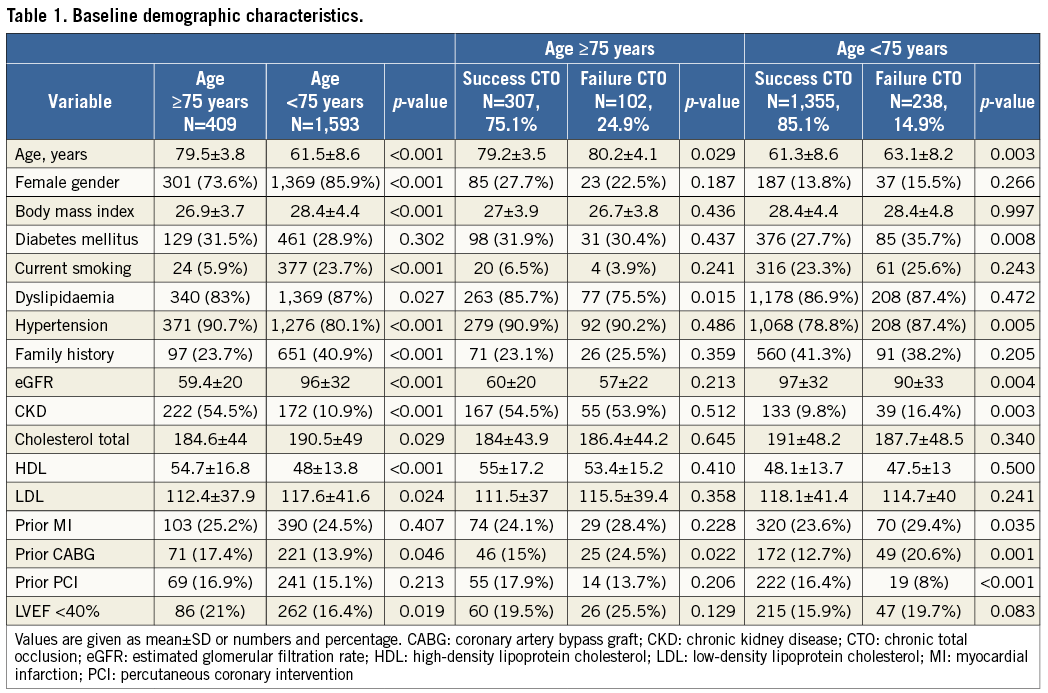
Successful CTO PCI was achieved in 307 (75%) patients. Elderly patients with failed CTO PCI were older, more often had a history of prior CABG and were less frequently diagnosed with dyslipidaemia. Furthermore, they more often had moderate/severe calcified lesions and longer fluoroscopic time (Table 2). In patients <75 years, those with successful CTO PCI were younger, had a higher mean estimated glomerular filtration rate, and less often presented with hypertension and a history of prior CABG. Furthermore, they were less likely to have multivessel disease, moderate/severe calcified atherosclerotic plaques, and long CTO lesions.
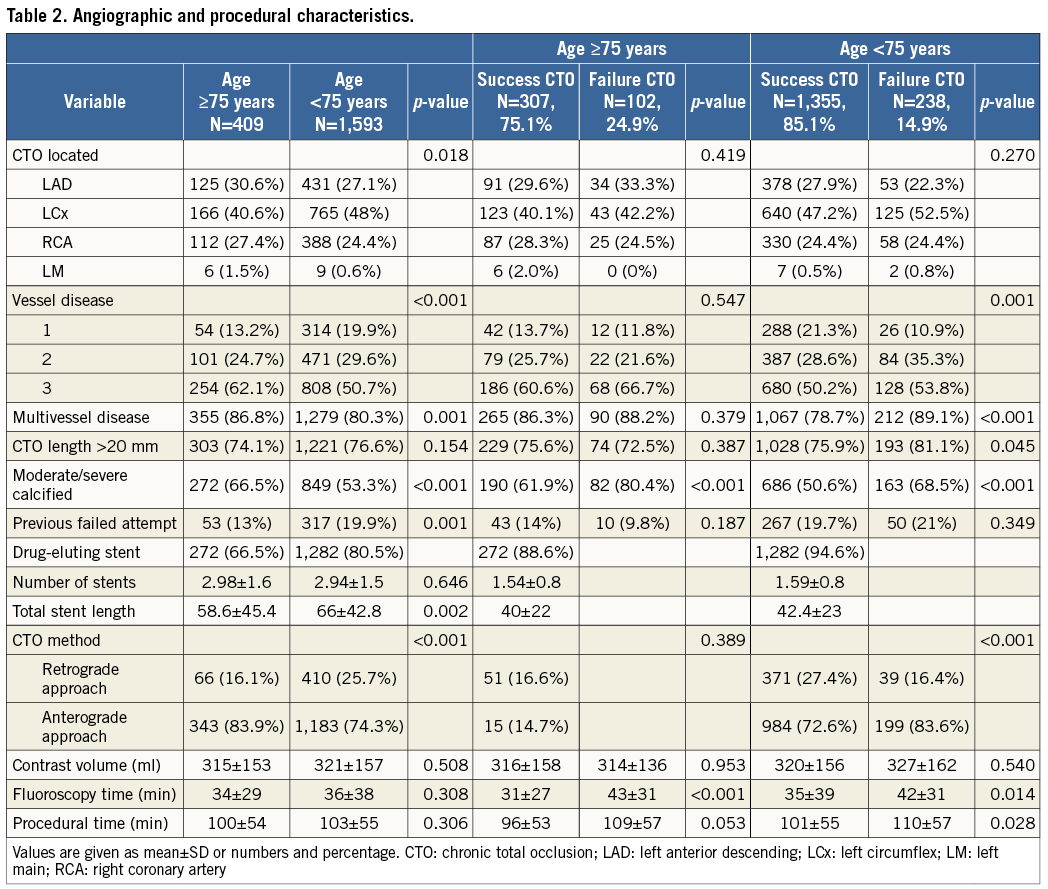
A retrograde attempt was tried more frequently in younger patients and fluoroscopy time was shorter (Table 2). The success rate of CTO PCI was significantly higher than with elderly patients (85% vs. 75%; p<0.001).
IN-HOSPITAL OUTCOME
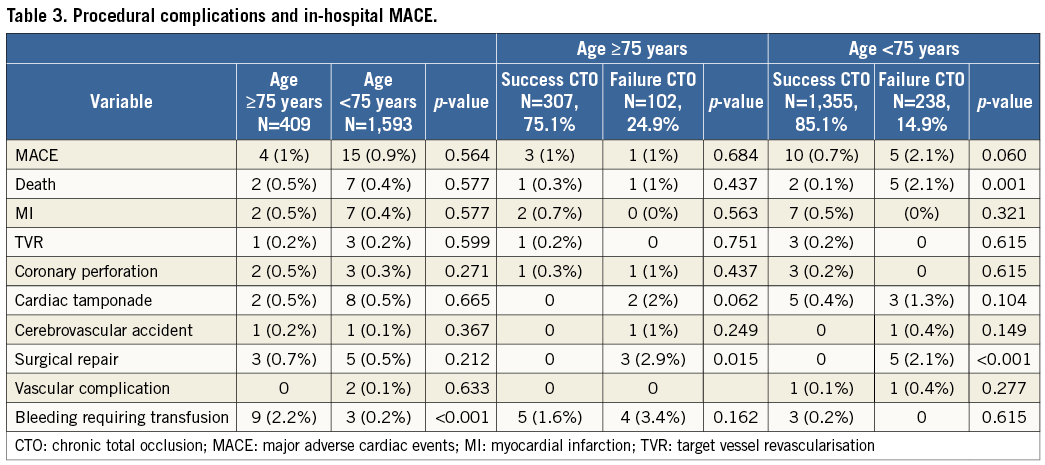
In-hospital complications are summarised in Table 3. Nine patients (0.4%) died: eight cardiovascular deaths and one death due to septic shock were observed. There were no significant differences in terms of in-hospital MACE rates between elderly and younger patients. Bleeding requiring transfusion was more frequently encountered in elderly as compared to younger patients (p<0.001).
LONG-TERM SURVIVAL
After a median follow-up of 2.6 years (interquartile range 1.1-3.1 years), 238 patients had died. All-cause mortality was significantly higher in the elderly patients as compared to the younger patients (26.7% versus 8.3%, p<0.001) (Figure 1A). This difference in all-cause mortality between groups persisted after multivariable adjustment for baseline characteristics (adjusted HR 1.98, 95% CI: 1.47-2.66, p<0.001). Compared with younger patients, elderly patients had higher rates of MACE (39.6% versus 28.6%, p<0.001) (Figure 1B), of the combined endpoint all-cause death and myocardial infarction (31.3% versus 10.9%, p<0.001), as well as of target vessel revascularisation (12.7% versus 20%, p<0.001). The adjusted incidence of MACE was similar in both groups (adjusted HR 1.15, 95% CI: 0.93-1.41, p=0.19). Figure 2 shows the cumulative mortality according to success or failure of recanalisation of CTO PCI stratified for patient age. In both groups, there was a significant survival benefit of successful CTO PCI. Without adjustment, the absolute reduction in mortality by successful CTO PCI was numerically greater in elderly as compared to younger patients (22.1% vs. 7.2% at three years, respectively). Successful CTO PCI was associated with lower rates of all-cause mortality in both the elderly (HR 0.55, 95% CI: 0.37-0.82; p=0.003) and younger (HR 0.43, 95% CI: 0.29-0.62; p<0.001) patient groups (pint=0.30) (Figure 2A, Figure 2B). These associations remained significant after multivariable adjustments in both the elderly (adjusted HR 0.58, 95% CI: 0.39-0.87; p=0.009) and the younger (adjusted HR 0.59, 95% CI: 0.40-0.86; p=0.006) patient groups. While in the group <75 years the rate of MACE was significantly reduced in patients with procedural success (adjusted HR 0.70, 95% CI: 0.55-0.88, p=0.002), differences were not significant in the ≥75 group (adjusted HR 0.84, 95% CI: 0.59-1.20, p=0.34) (Figure 3A, Figure 3B).
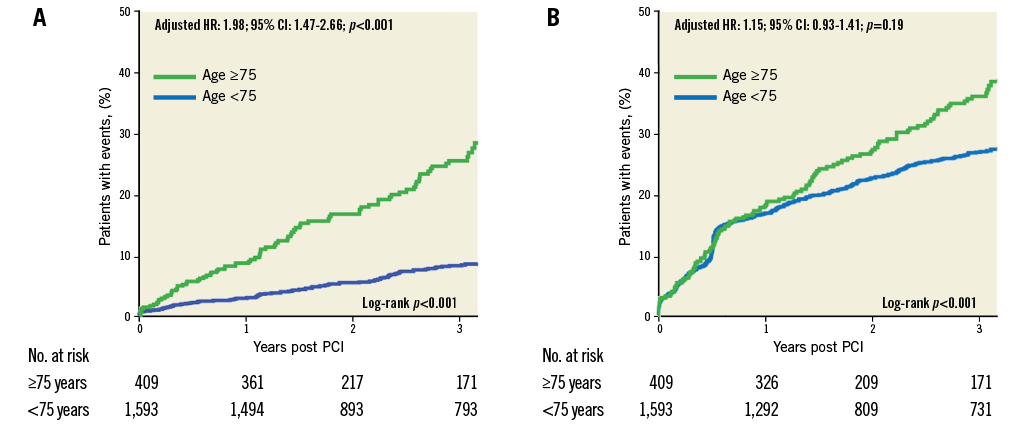
Figure 1. Kaplan-Meier curve estimates stratified by age. A) All-cause mortality. B) Major adverse cardiovascular events. MACE denotes major adverse events (the composite of all-cause death, non-fatal myocardial infarction, and target vessel revascularisation). CI: confidence interval; HR: hazard ratio
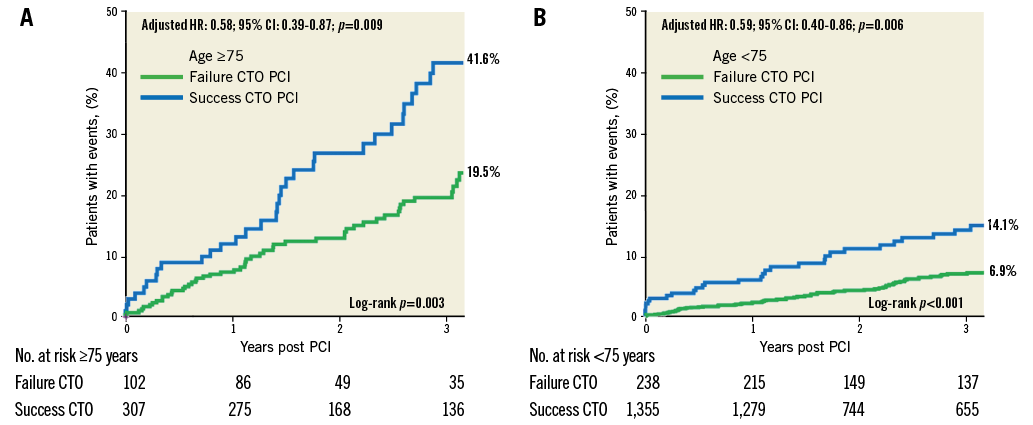
Figure 2. Kaplan-Meier curve estimates for all-cause mortality with successful and failed CTO PCI. A) Older patients. B) Younger patients. CI: confidence interval; CTO: chronic total occlusion; HR: hazard ratio; PCI: percutaneous coronary intervention
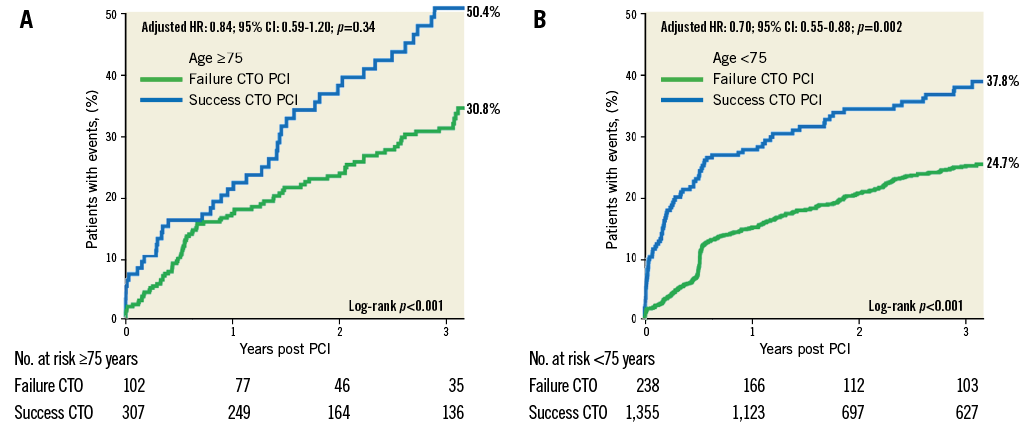
Figure 3. Kaplan-Meier curve estimates for major adverse cardiovascular events with successful and failed CTO PCI. A) Older patients. B) Younger patients. MACE denotes major adverse cardiovascular events (the composite of all-cause death, non-fatal myocardial infarction, and target vessel revascularisation). CI: confidence interval; CTO: chronic total occlusion; HR: hazard ratio; PCI: percutaneous coronary intervention
When planned CABG after failed CTO recanalisation was not considered as MACE, the incidence of MACE was not significantly different between successful and failed recanalisation in both younger and elderly patients (adjusted HR 0.95, 95% CI: 0.74-1.23, p=0.13, and 0.85, 95% CI: 0.54-1.06, p=0.35, respectively).
Discussion
This study demonstrates a similar survival benefit in elderly (≥75 years) as compared to younger patients after successful CTO PCI in the contemporary DES era, with comparable low rates of procedural complications and adverse in-hospital events. These findings strongly suggest that CTO PCI, when indicated, should not be withheld from the elderly patient population.
Previously, Hoebers et al were unable to show a significant association between successful CTO PCI and mortality (during median follow-up of 890 days 19.6% vs. 24.6%, p=0.13), which might have been due to a smaller number of elderly CTO patients in this earlier study10. Nevertheless, they reported a lower incidence of MACE after successful versus failed CTO PCI in elderly patients (25.8% vs. 42.3%, p=0.02), which was mainly driven by reduced referral for CABG in patients who underwent successful CTO PCI. In our patient cohort, MACE rates did not differ between after successful versus failed procedures in elderly patients, which may at least, in part, be explained by differences in the definition of adverse events and TVR. Similarly, Tanaka et al found a significantly lower mortality after successful versus failed CTO PCI in elderly patients (≥75 years), but not in younger patients11. While our data are in agreement with their findings in elderly patients, we also observed a survival benefit in younger patients. The inconsistency may have arisen from very rigorous exclusion criteria applied in the study by Tanaka et al, as patients with prior CABG were excluded and the prevalence of multivessel disease was rather low in their study. In contrast, we used an “all-comer” design and applied wide inclusion criteria. Using rigorous exclusion criteria may have led to a reference population that represents a “too healthy” part of the population which corresponds with a limited number of adverse events, possibly leading to overfitting of multivariable models. Thus, we believe that our study represents a reasonable balance in order to have a relevant elderly reference population reflecting the real world, and is sufficiently powered to assess adverse events following CTO PCI.
Overall, in-hospital MACE rates were low. These numbers compare well with previous reports and mirror the high survival rate following procedural success in this study population12. Notably, although more extensive and calcified CAD along with tortuous anatomy and more severe coronary calcification were observed in older patients, no significant difference was found for in-hospital mortality between older and younger patients. Bleeding requiring transfusion was significantly more common in elderly than in younger patients. It is well described that post-procedural bleeding is one of the most common critical complications occurring in elderly patients following PCI3,13. A transradial approach has been suggested to reduce bleeding complications during PCI14,15. Indeed, in CTO PCI, the transfemoral approach is still the most extensively used access route, since CTO procedures usually require the introduction of a larger lumen guiding catheter and wider device application. Moreover, dual catheter deployment for contralateral contrast injections and the retrograde approach can be managed more easily via the femoral access. Notably, a recent meta-analysis16 has shown that the majority of patients with bleeding complications experienced non-access-site bleeding, indicating that only a minor proportion of bleeding complications could have been prevented by a radial approach. In addition, it has to be borne in mind that the impact of access-site bleeding on survival is substantially lower than that of non-access-site bleeding
Historically, elderly patients undergoing elective PCI have consistently shown lower rates of procedural success and higher rates of complications including in-hospital mortality, stroke, vascular complication, and recurrent MI compared to younger cohorts17-19. Moreover, they show more extensive coronary artery disease, tortuosity, and severely calcified atherosclerotic plaques. In addition, elderly patients often have multiple comorbidities including chronic kidney disease, which increase the risks associated with PCI20,21. Consistent with this notion, we found a higher percentage of systolic dysfunction, chronic kidney disease, prior CABG and coronary multivessel disease in the advanced age group, which may have accounted for the lower CTO PCI success rate observed in elderly patients as compared to younger ones. Nevertheless, the procedural success rate of 75% in elderly patients was still high in the present study and comparable with three other recent reports in elderly patients10,11,22.
The greatest absolute risk reduction (22.1%) for all-cause mortality following successful CTO PCI was found in patients ≥75 years of age. In younger patients, successful CTO PCI led only to a 7.2% absolute risk reduction, indicating that the absolute risk reduction is largely dependent on baseline risk which was substantially higher in elderly patients10,23. Nevertheless, HRs for survival after successful versus failed CTO PCI were not significantly different between elderly and younger patients. Thus, contrary to what may be assumed, elderly patients compared with younger patients did not appear to profit more from recent advances in PCI technologies such as the widespread use of DES, or from more intensified post-procedural medical treatment such as the administration of high-dose statins and platelet inhibitors. Nevertheless, these recent advances may have contributed to the overall success of CTO recanalisation by PCI. Indeed, recent US registries have shown that, compared with BMS implantation, the use of DES for revascularisation of CTOs is associated with a lower long-term mortality rate24. Higher rates of multivessel PCI and more prolonged dual antiplatelet therapy at the index procedure in the DES-treated patients may contribute to a lower burden of ischaemia and an improved ventricular function.
Limitations
There are limitations to this study that should be pointed out. First, our study carries the inherent limitations of a retrospective single-centre study. Second, only patients undergoing CTO revascularisation were included, and patients receiving only medical treatment were not studied. Although we show survival benefits by successful CTO PCI in both elderly and younger patients, it has to be borne in mind that these findings based on registry data cannot settle the issue. Specifically, we cannot exclude that additional confounding factors that were not measured in the present study might have influenced the outcome measures.
Conclusions
We found that successful CTO PCI is an independent positive predictor of long-term survival in patients above the age of 75 years. Because the population has become an ageing society with a consequent increase in the prevalence of CAD, the clinical significance of improved outcomes in elderly patients after successful CTO PCI is very important. Thus, revascularisation CTO PCI therapy should be indicated in elderly patients when appropriate, and should not be withheld owing to higher age or greater morbidity.
Large randomised trials will be required to test whether CTO PCI will improve long-term outcomes in elderly patients as compared to medical standard-of-care treatment or CABG. In addition, risk predictors for procedural failure will have to be identified in this population in order to optimise patient selection and reduce complications further.
| Impact on daily practice Elderly patients undergoing CTO PCI show the same survival benefit as younger patients. Thus, patients should not be denied percutaneous revascularisation of CTO because of advanced age. |
Conflict of interest statement
The authors have no conflicts of interest to declare.