Abstract
Aims: To evaluate the frequency, predictors and prognostic significance of elevation in cardiac troponin I (cTnI) after coronary angiography (CAG).
Methods and results: A series of 296 consecutive patients with normal pre-procedural cTnI levels and undergoing elective CAG at our centre were prospectively analysed. Positive cTnI elevation was defined as >0.06 ng/ml. Positive cTnI elevation was observed in 44 patients (14.8%), but CK-MB was elevated in only four patients (1.3%) after the procedure. The risk of cTnI elevation was independently associated with left ventricular hypertrophy (odds ratio [OR] 5.52; 95% confidence interval [CI], 2.54 to 12.02; P<0.001), inexperienced operator (OR 10.83; 95% CI, 2.47 to 47.43; P=0.002) and the amount of contrast agent (OR 1.12; 95% CI, 1.03 to 1.23; P=0.009 for each 10 ml increase), whereas it was not associated with the severity of coronary artery disease. At one year, however, postprocedural elevation of cTnI was not associated with an increased risk of death (2.3% vs. 0.8%, P=0.384) or myocardial infarction (2.3% vs. 2.0%, P=0.623).
Conclusions: A minor elevation of cTnI is observed commonly after CAG, which might be associated with left ventricular hypertrophy, operator’s experience and the amount of contrast used; however, it does not influence 1-year events rates.
Introduction
Both cardiac troponins I (cTnI) and T are preferred biomarkers for the diagnosis of myocardial injury and necrosis because they have nearly absolute myocardial tissue specificity as well as high clinical sensitivity1, thereby reflecting even microscopic zones of myocardial necrosis2. Prior studies have demonstrated that troponin elevation after percutaneous coronary intervention (PCI) is common, occurring in up to 48% of patients3-10, which may result from recognisable periprocedural events, such as side-branch occlusion, disruption of collateral flow, distal embolisation, intimal dissection, coronary spasm, slow flow or no-reflow, and microvascular plugging 1,4,8,10,12,13. Furthermore, several trials highlighted that troponin release may lead to an increased risk of late adverse events such as death and myocardial infarction, even with minor elevations in these cardiac enzymes3-7. At present, diagnostic coronary angiography (CAG) is considered to be one of the most reliable tools to evaluate the severity of coronary artery disease. Its safety has been well established since mortality related to the procedures themselves has been reported to be very low, at 0.1% or less14,15. The most frequent cardiac complication reported is a 0.05% to 0.1% incidence of acute myocardial infarction13-15, but minor myocardial damage has been likely underestimated given the lack of routine enzyme determinations after CAG. During CAG, the manipulation of the diagnostic catheters and repeated injection of contrast medium can lead to subtle myocardial injury because of dislodgement of atherosclerotic debris from the aortic wall, thrombus arising from catheters, coronary dissections, air embolisation, the reduction in coronary flow reserve, and shear stress-induced endothelial damage13,16-21. However, no reliable data to date has definitively demonstrated on the topic of CAG-related myocardial injury, leading to the elevation of troponin levels despite large numbers of procedures in many countries and centres. Accordingly, the aim of this study was to investigate the incidence, predictors, and clinical significance of elevated cTnI after CAG in a consecutive series of patients with normal pre-procedural cTnI.
Materials and methods
Patient population
The present study included all consecutive patients from January 2007, when routine measurements of cTnI were initiated for our patients undergoing elective CAG, through November 2007. Inclusion criteria were a normal pre-procedural cTnI and creatine kinase-MB fraction (CK-MB). Exclusion criteria were evolving or recent myocardial infarction; presence of unstable symptoms accompanied by abnormal cardiac serum markers warranting emergency coronary angiography; renal insufficiency with serum creatinine >2.0 mg/dl; or an unavailability of serum markers or follow-up data. Patients who underwent PCI immediately after CAG were also excluded. Of the 467 patients undergoing elective CAG during the study period, 171 patients were excluded – 89 underwent PCI immediately after CAG, 41 had elevated baseline cTnI or CK-MB, 22 had renal insufficiency with creatinine >2.0 mg/dl, and 19 had only pre-procedural sample – leaving 296 patients who were considered to be eligible for analysis (Figure 1). The study protocol was approved by an appropriate institutional ethics committee.

Figure 1. Study profile.
Sample collection
Preprocedural samples for cTnI and CK-MB were collected within 24 hours before CAG. A postprocedural cTnI and CK-MB were measured 16 to 22 hours after CAG. Samples of cTnI were analysed by a chemiluminescent enzyme immunoassay (Access 2; Beckman Coulter, Brea, CA, USA). The upper limit of normal (ULN) for cTnI was 0.06 ng/ml, which represented the 99th percentile of the distribution of a reference control group with an analytical imprecision of no more than 10%. The analytical sensitivity for cTnI assay was 0.01 ng/ml. Positive cTnI elevation was therefore defined as >0.06 ng/ml after CAG. CK-MB was measured by the chemiluminescence assay using specific monoclonal antibodies against CK-MB. Laboratory ULN was 6.4 ng/ml for CK-MB.
Procedures and definition
Diagnostic coronary angiography was performed according to standard methods of manual contrast injection via a femoral or radial approach, with arterial introducers of size 4 to 6 Fr, and 2000 IU of heparin was given before the procedure. Each angiographic sequence was preceded by intracoronary injection of nitroglycerine. Low osmolality contrast medium was used in all patients. Coronary arteries with at least 50% stenosis were defined as diseased. The severity of coronary artery disease was also estimated by calculating the Gensini score3. The experienced operator was defined as having performed a minimum of 300 CAG procedures. Left ventriculography were routinely performed immediately after CAG, if possible. Left ventricular (LV) end-diastolic volume and LV end-systolic volume were measured using Simpson’s method, and then the ejection fraction was calculated.
Echocardiograms were performed using standard 2-dimensional measurements. The LV measurements included ventricular septum thickness (VST), the posterior wall thickness (PWT) and LV internal dimension (LVID) at end-diastole, which were obtained from 2-dimensional echocardiographic guided M-mode from the parasternal long-axis view. LV mass was calculated using the regression equation described by Devereux et al5: LV mass=1.04×([VST+PWT+LVID]3–[LVID]3)–13.6 g, and was divided by body surface area to determine the LV mass index. Sex specific LV hypertrophy was defined as LV mass index ≥110 g/m2 in women and ≥134 g/m2 in men.
Estimated glomerular filtration rate (eGFR) was determined by the Modification of Diet and Renal Disease calculation (eGFR [ml/min/1.73 m2]=186.3×serum creatinine [mg/dl]–1.154×age [years]-0.203×0.881×0.742 [if female])6. In this formula, 0.881 is the coefficient used for an eGFR specific to the Japanese population, as recommended by the Japanese Society of Nephrology6.
Myocardial infarction during follow-up was defined by a new ST/T wave changes or Q-wave on the electrocardiogram, and an increase of cardiac biomarker (CK-MB or cTnI) levels above the ULN associated with chest pain, according to the consensus statement of the joint European Society of Cardiology, the American College of Cardiology Foundation, the American Heart Association and the World Heart Federation task force for the redefinition of myocardial infarction1. All deaths were considered cardiac unless an unequivocal non-cardiac cause could be established. Diabetes was defined by current use of insulin or oral hypoglycaemic agents, or known and untreated high blood sugar (fast blood sugar level ≥126 mg/dl). Hypertension was defined by current use of antihypertensive medication or known and untreated hypertension. Hypercholesterolaemia was similarly defined by use of cholesterol-lowering medication or known but untreated high cholesterol (total cholesterol ≥240 mg/dl or low-density lipoprotein ≥160 mg/dl). Hypertriglyceridaemia was defined as a fasting triglyceride concentration ≥200 mg/dl.
Clinical follow-up examinations were conducted on an outpatient basis at least once a month until one year after the procedure. All adverse events at one year were confirmed by reviewing the medical records of the patients followed at our institution, and by telephone contact with patients or the next of kin or information from referring physicians when patients were followed elsewhere. Follow-up data on clinical events at one year were available in all cases.
Statistical analysis
Data were expressed as mean±SD for continuous variables and as percentages for discrete variables. Student’s unpaired t test or Mann-Whitney U test was used to compare continuous variables between groups. Categorical variables were compared by χ2 test or Fisher’s exact test, as appropriate. Odds ratios and 95% confidence intervals (CI) assessing the independent predictors of the positive cTnI elevation according to potential confounding variables were determined by a logistic regression analysis. The following parameters were evaluated first in a univariate model: gender; age; diabetes; hypertension; history of heart failure and myocardial infarction; LV hypertrophy; use of aspirin, ticlopidine/clopidogrel, beta-blockers and statins; cTnI and CK-MB levels at baseline; procedure time; contrast agent dose: inexperienced operator; left anterior descending lesion; multivessel disease; and left ventriculography. Variables with a P value <0.20 in a univariate analysis were then entered into a multivariable logistic regression analysis using stepwise selection. For the stepwise procedure, an entry criterion P value of 0.05 and a stay criterion of 0.10 were used. The Hosmer-Lemeshow test was used for assessing overall model fit. All calculation was performed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA). A 2-sided P value <0.05 was considered statistically significant.
Results
Among the 296 patients, baseline and post-procedural cTnI levels were 0.021±0.011 ng/ml and 0.061±0.285 ng/ml, respectively (P=0.016) (Figure 2).
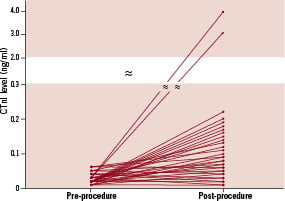
Figure 2. Changes in troponin I values between pre- and postprocedure.
As a result, positive cTnI elevation (>1×UNL) was observed in 44 patients (14.8%). The incidences of cTnI elevation greater than 2×, 3× and 5×UNL were 4.4%, 2.0%, and 0.7%, respectively. Additionally, CK-MB was elevated (>1×UNL) in only four patients (1.3%) after the procedure.
Clinical characteristics
The clinical characteristics of patients with and without positive cTnI elevation are listed in Table 1.
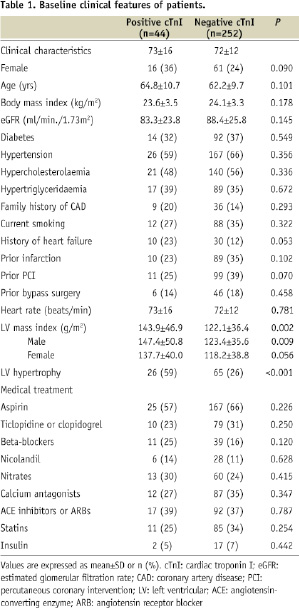
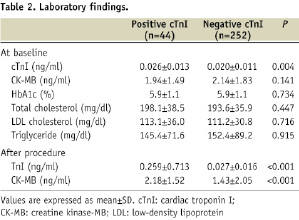
Postprocedural cTnI positive patients were more likely to have LV hypertrophy. There was no significant difference in prevalence of cardiovascular risk factors or medical therapy in the two groups. Patients with positive cTnI elevation had greater cTnI value at baseline than in those without, which also showed greater cTnI and CK-MB values after the procedure (Table 2).
Procedural characteristics
Table 3 compares the procedural and angiographic characteristics of the positive and negative cTnI group.
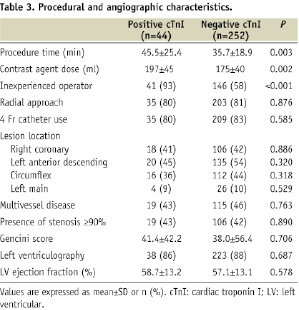
Procedure time was significantly longer and the dose of contrast agent used was higher in the cTnI positive group than cTnI negative group. Interestingly, cTnI positive patients underwent CAG by inexperienced operators more often compared with cTnI negative patients. There were no significantly differences in terms of LV ejection fraction, catheter size, lesion location or severity of coronary artery disease in the two groups. During the procedure, there were no coronary dissections, perforation or ventricular tachycardia/fibrillation in either group. Angiographically visible air embolisation occurred in two patients in the cTnI positive group, which was induced by inexperienced operators, but none in the cTnI negative group. Emergency bypass surgery was not required in either group.
When the results were analysed in terms of the operator experience, positive cTnI elevation occurred in three of 109 patients (2.6%) in the experienced operators and 41 of 187 patients (21.9%) in the inexperienced operators (P<0.001). Furthermore, the rate of positive cTnI elevation in the inexperienced operator having performed less than 100 CAG procedures was extremely high, at 26.7%. As compared with the experienced operators, the inexperienced operators showed similar baseline clinical characteristics of patients but needed greater procedure time (41±22 vs. 31±14 min, P<0.001) and higher dose of contrast medium (186±42 vs. 164±37 ml, P<0.001).
Predictors of elevated troponin I levels
Table 4 summarises predictors of postprocedural cTnI elevation in the study patients.
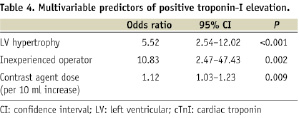
Overall model was fitted according to the Hosmer-Lemeshow test (P=0.404). According to multivariable analysis, inexperienced operator (odds ratio, 10.83; 95% CI, 2.47 to 47.43; P=0.002), LV hypertrophy (odds ratio, 5.52; 95% CI, 2.54 to 12.02; P<0.001), and the amount of contrast medium used (odds ratio, 1.12; 95% CI, 1.03 to 1.23; P=0.009 for each 10 ml increase) were the independent predictors of positive cTnI elevation after non-urgent CAG alone.
Clinical outcomes
Cardiac event rate at 1-year post index procedure is presented in Table 5.

Three patients died during the study period (all cardiac-related deaths): one patient (2.3%) in the cTnI positive group at 197 days after the procedure and two patients (0.8%) in the cTnI negative group at 224 days and 334 days after CAG. There was no significant difference in the rate of occurrence of myocardial infarction in the two groups. However, none of myocardial infarction events were related to periprocedural myocardial damage. The rates of non-urgent bypass surgery and PCI were similar in the two groups. As a result, no significant difference was observed in terms of composite rate for all adverse cardiac events between patients with and without cTnI elevation (20.5% vs. 22.6%, P=0.750). In addition, incidences of death and myocardial infarction were similar between the inexperienced and experienced operator (1.1% vs. 0.9%, P=0.694 and 2.1% vs. 1.8%, P=0.610, respectively).
Discussion
In this current era, CAG is recognised as a safe and reliable tool to assess the severity of coronary artery disease because of extremely low rate of major complications such as death and acute myocardial infarction13-15. However, the frequency and clinical relevance of subtle myocardial injury related to the CAG procedures still remains uncertain, presumably due to the lack of routine enzyme determinations in a clinical practice and large confirmatory studies. In 53 consecutive patients, Katritsis et al demonstrated that no patients had any increase in cTnI after CAG, with the exception of a minor increase in one patient13. Unfortunately, sample size of this study was much smaller than our study and the analytical sensitivity for cTnI assay was 0.1 ng/ml in this study (0.01 ng/ml in our study). Hypothetically, CAG-related myocardial damage can occur through several potential mechanisms13,16-21,25. Platelet thrombi can be formed on the luminal and external surfaces of catheters and on their guidewires during coronary arterial catheterisation, which may lead to occlusion of a coronary artery16. Coronary air embolisation, which occurs in 0.1% to 0.3% of cases, is another recognised cause of myonecrosis during cardiac catheterisation21. A previous report by Keeley et al demonstrated that in more than 50% of PCI procedures, catheter placement was associated with scraping debris from the aortic wall19. It is possible that atheromatous debris is inadvertently flushed forward during contrast injection, resulting in coronary embolisation. Another study revealed that the increase in shear stress induced by forceful injection could damage the endothelial surface and promote plaque rupture18. Furthermore, frequent injection of contrast medium can reduce coronary flow reserve17, resulting in subsequent cardiac biomarker elevation25. These previous findings suggest that minor myonecrosis related to CAG may be present in a significant proportion of patients, even in those without diagnosis as periprocedural myocardial infarction.
The inexperienced operators are, in general, less likely to have sufficient skill in the manipulation of the diagnostic catheters and the injection of contrast material, leading to need for higher dose of contrast medium and longer procedure time26. Consequently, CAG performed by the inexperienced operator may increase the likelihood of myocardial damage and subsequent troponin release through the mechanisms that cTnI elevation is associated with macro- and micro-vascular injury. In the current study, the trans-radial approach was used nearly 80% of the procedures. Because the transradial approach is technically more demanding than the femoral approach27, the frequent use of this approach in our study might be one of the possible explanations for higher incidence of elevated cTnI by the inexperienced operators. More effective training of physicians may be required, particular when radial access is used. As expected, LV hypertrophy was associated with an increased risk of cTnI elevation in this study. Increased oxygen demand derived from increased muscle mass, coupled with reduced flow reserve due to remodelled coronary microcirculation, may lead to subendocardial ischaemic injury during CAG in this particular population28.
Focusing on the clinical outcomes, positive cTnI elevation after CAG was not associated with a significant increase in mortality and incidence of myocardial infarction at one year. Because this study excluded high-risk subsets such as patients with significant renal insufficiency and elevated baseline cTnI values (acute coronary syndrome), our results may be more applicable to a low- to moderate-risk population, which is less likely to result in poor prognosis. Moreover, the prevalence of cTnI elevation greater than 5×UNL in this study was very low 0.7% as well as CK-MB elevation (>1×UNL) occurred in only 1.3% of patients, suggesting that most of patients with positive cTnI elevation were likely to have less myocardial damage compared with patients in previous reports showing that the elevation of troponins after PCI increased risk of cardiac events3-7. Cardiac troponins can be released into the systemic circulation in the absence of myocardial necrosis and can occur in conditions that produce cardiomyocyte membrane permeability such as demand ischaemia29. It is, therefore, possible to assume that extremely small sized myonecrosis and/or potentially reversible myocardial injury related to the CAG procedures themselves, such as those reflected by minor elevation of cTnI without CK-MB release, do not influence the prognosis within a 1-year observation period. On the other hand, the high sensitivity of this biomarker in detecting myocardial cell damage may reduce its ability to predict prognosis.
In the present study, 41 patients with elevated baseline cTnI or CK-MB were excluded. Baseline pre-PCI cTnI value was shown to be associated with long-term death and myocardial infarction rates30. We therefore excluded these patients to make the clinical relevance of CAG-related cTnI elevation clear. Finally, this is a prospective single-centre trial and the sample size of the study was quite limited with low event rates. As a result, the present study might be under-powered to detect any effect on long-term evolution of cTnI release after CAG. Confirmatory studies with a larger number of patients for longer study periods are required to clarify this issue.
Conclusions
Our results demonstrate that minor elevation of cTnI related to CAG procedure alone occurs in 14.8% of our patients presenting clinically and biochemically stable coronary artery disease and undergoing non-urgent CAG. The risk of cTnI elevation is independently associated with LV hypertrophy, inexperienced operator and the amount of contrast agent used, whereas it is not associated with the severity of coronary artery disease. A minor elevation in cTnI, however, does not lead to an increased risk of adverse cardiac events wthin1-year observation.

