
Abstract
Aims: Elevated levels of high-sensitivity troponin are seen in a significant proportion of stable patients undergoing elective coronary assessment. Multiple variables have been associated with troponin levels. The present analysis sought to identify variables independently associated with elevations of troponin and their relative strength of association with this biomarker.
Methods and results: Stable patients undergoing elective coronary angiography and echocardiographic assessment were enrolled. High-sensitivity troponin T (hsTnT) was determined before any diagnostic procedures. Multivariable linear regression models including angiographic and echocardiographic parameters were used to identify independent predictors of levels of troponin and to determine their relative contribution to levels of troponin. Out of 2,046 patients, 15% presented with levels of troponin above the upper reference limit of normal. In a combined analysis, gender followed by renal function, age, left ventricular ejection fraction, diabetes, and left ventricular mass showed the strongest association with levels of troponin. Coronary obstruction was also an independent predictor, but strength of association weakened following adjustment.
Conclusions: Up to 15% of patients undergoing coronary assessment outside the setting of acute coronary syndromes present with elevated levels of cardiac troponin. These changes are independently associated with multiple clinical, laboratory, and imaging variables. (ClinicalTrials.gov Identifier: NCT00457236)
Introduction
Cardiac troponin is the preferred blood marker for cardiomyocyte damage given its unchallenged myocardial tissue specificity1. For patients with acute coronary syndromes, current guidelines recommend the use of this biomarker for evaluation of diagnosis and prognosis2,3. The evolution of assays over recent years has mainly improved the sensitivity of assays1,4,5. This allows detection of troponin levels in 25-80% of stable patients depending on the high-sensitivity troponin assay used6-8. Further data suggest that even low-level elevations of troponin in stable subjects are associated with an increased risk of subsequent cardiovascular events7-9. This association might be explained by the detection of subclinical and undiagnosed cardiac pathologies, such as obstructive coronary atherosclerosis, by cardiac troponin7,8,10.
Recent data have demonstrated that a significant proportion of stable patients undergoing elective coronary angiography present with elevated levels of troponin11. However, a significant proportion of these patients are not diagnosed with obstructive coronary heart disease since multiple factors are also associated with elevated levels of troponin such as male gender, age, renal function, pulmonary embolism, sepsis, anaemia, and diabetes mellitus. Little is known about the relative contribution of these single variables to variability in levels of troponin. It is also uncertain if some of these variables are not just surrogates of other conditions more directly related to elevations of troponin (e.g., left ventricular dysfunction as surrogate of coronary heart disease). Thus, the present analysis sought to identify independent predictors of elevations of troponin, and to analyse how strongly they are associated with levels of troponin following adjustment for invasive and non-invasive cardiovascular imaging results.
Methods
STUDY POPULATION
This study represents a secondary retrospective analysis of the prospective observational EXCELSIOR trial (Impact of Extent of Clopidogrel-Induced Platelet Inhibition during Elective Stent Implantation on Clinical Event Rate; ClinicalTrials.gov Identifier: NCT00457236)12,13. In brief, stable patients with suspected obstructive coronary heart disease due to positive stress testing and/or typical symptoms scheduled for elective cardiac catheterisation were eligible for the study. The primary analysis investigated the impact of on-clopidogrel platelet function on the clinical outcome of patients undergoing coronary intervention. Major exclusion criteria were acute myocardial infarction (MI) with a rise and fall of cardiac troponin as defined by current guidelines14, signs of ischaemia at rest, known severe valvular heart disease, chronic oral anticoagulation, thienopyridine pretreatment, active cancer, haemodialysis, and haemodynamic instability. All patients underwent full cardiovascular assessment including electrocardiogram, echocardiography, and coronary angiography.
From 2003 to 2004, 2,053 patients were enrolled in this study. Blood samples for biomarker testing were missing from seven persons, leaving 2,046 patients for the present analysis. All patients gave written informed consent. The study was approved by the ethics committee of the University of Freiburg, Germany.
LABORATORY PROCEDURES
Blood samples for biomarker testing were collected in serum tubes after enrolment and before coronary angiography. Within one hour, samples were carefully processed and frozen at –80°C until assayed in a blinded fashion in the central laboratory. High-sensitivity troponin T (hsTnT) was measured with a sandwich enzyme electrochemiluminescence immunoassay (Roche Diagnostics, Mannheim, Germany) using lot number 153401 that is not affected by the recently detected shift in the low end measuring range. This assay has a limit of blank of 3 ng/L, a limit of detection of 5 ng/L, a 99th percentile of a healthy population cut-off point of 14 ng/L, and a coefficient of variation of less than 10% at 13 ng/L15. Creatinine clearance was estimated with the use of the Cockcroft-Gault formula.
IMAGING STUDIES
Echocardiographic results, including at least basic data such as left ventricular ejection fraction and valvular status, were available from all enrolled subjects. A complete and detailed echocardiographic assessment including quantification of cardiac chamber size, ventricular mass, details of valvular anatomy, central venous filling, and estimation of pulmonary artery pressure was available from 1,072 subjects. Echocardiographic results were assessed and described according to current recommendations16. Baseline characteristics were comparable for patients with at least basic and full echocardiographic assessment. For multivariable analyses, valvular heart disease was defined as the presence of at least moderate changes at any valve.
The results of coronary angiography regarding vessels of more than 1.5 mm in diameter were divided into four groups according to grade of stenosis: <20% - no or only very minor visible coronary changes; 20-49% - minimal coronary changes; 50-74% - intermediate coronary obstruction; and ≥75% (or left main disease ≥50%) - haemodynamically relevant coronary obstruction.
To analyse the extent of atherosclerotic burden in more detail, the Gensini score was calculated for all patients as previously described17. This score represents one of the most commonly used scoring systems to quantify the angiographic burden of coronary heart disease18.
STATISTICS
Discrete variables are reported as counts (percentages) and continuous variables as mean±standard deviation. Continuous variables with non-Gaussian distribution identified by Kolmogorov-Smirnov test were described as median (interquartile range). For discrete variables, we tested differences between groups with the χ2 test or Fisher’s exact test when expected cell sizes were less than five. We used the two-tailed t-test to compare continuous variables, or the Mann-Whitney U or Kruskal-Wallis test for non-Gaussian variables. In the two-sided test, a p-value <0.05 was regarded as significant.
Multivariable linear regression models were used to identify independent predictors of levels of hsTnT and to determine their strength of association with levels of hsTnT derived from partial η2. In these models, partial η2 describes the proportion of variance in hsTnT explained by a specific variable. Levels of hsTnT at presentation were entered as dependent variable and dichotomous variables as fixed factors. Results of hsTnT were entered log-transformed given their non-parametric distribution. To separate between generally available clinical variables and parameters only available by specific testing such as echocardiography or angiography, three different regression models were created (1st: only including clinical variables; 2nd: only including imaging variables; 3rd: all available variables). Statistical analyses were run with IBM SPSS Statistics, Version 22 (IBM Corp., Armonk, NY, USA).
Results
STUDY POPULATION
The distribution of hsTnT values on admission of the analysed 2,046 patients undergoing elective coronary angiography is shown in Figure 1. There was an exponential decrease in frequency with rising troponin levels. While 1,061 (52%) patients presented with hsTnT above the lower limit of detection (5 ng/L), only 315 (15%) had an hsTnT above the 99th percentile of a healthy population cut-off point (14 ng/L).
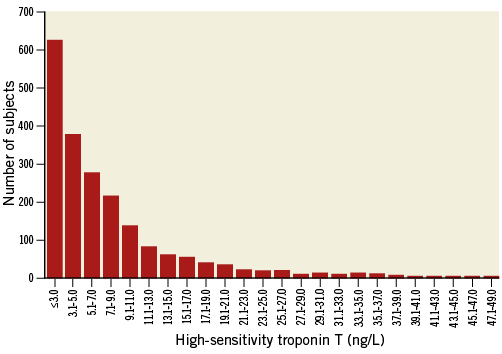
Figure 1. Distribution of high-sensitivity troponin T values.
Patients with hsTnT ≥5 ng/L at presentation were significantly older, more often male, had a higher proportion of clinical symptoms and cardiovascular risk factors such as diabetes mellitus and arterial hypertension, were more frequently on cardiovascular drugs such as ACE inhibitors and statins, and more often had a history of previous coronary events (Table 1). These patients were also more frequently diagnosed with obstructive coronary heart disease and demonstrated a higher proportion of reduced left ventricular (LV) ejection fraction, higher LV mass as well as more significant valvular heart disease and pulmonary hypertension during echocardiographic assessment.
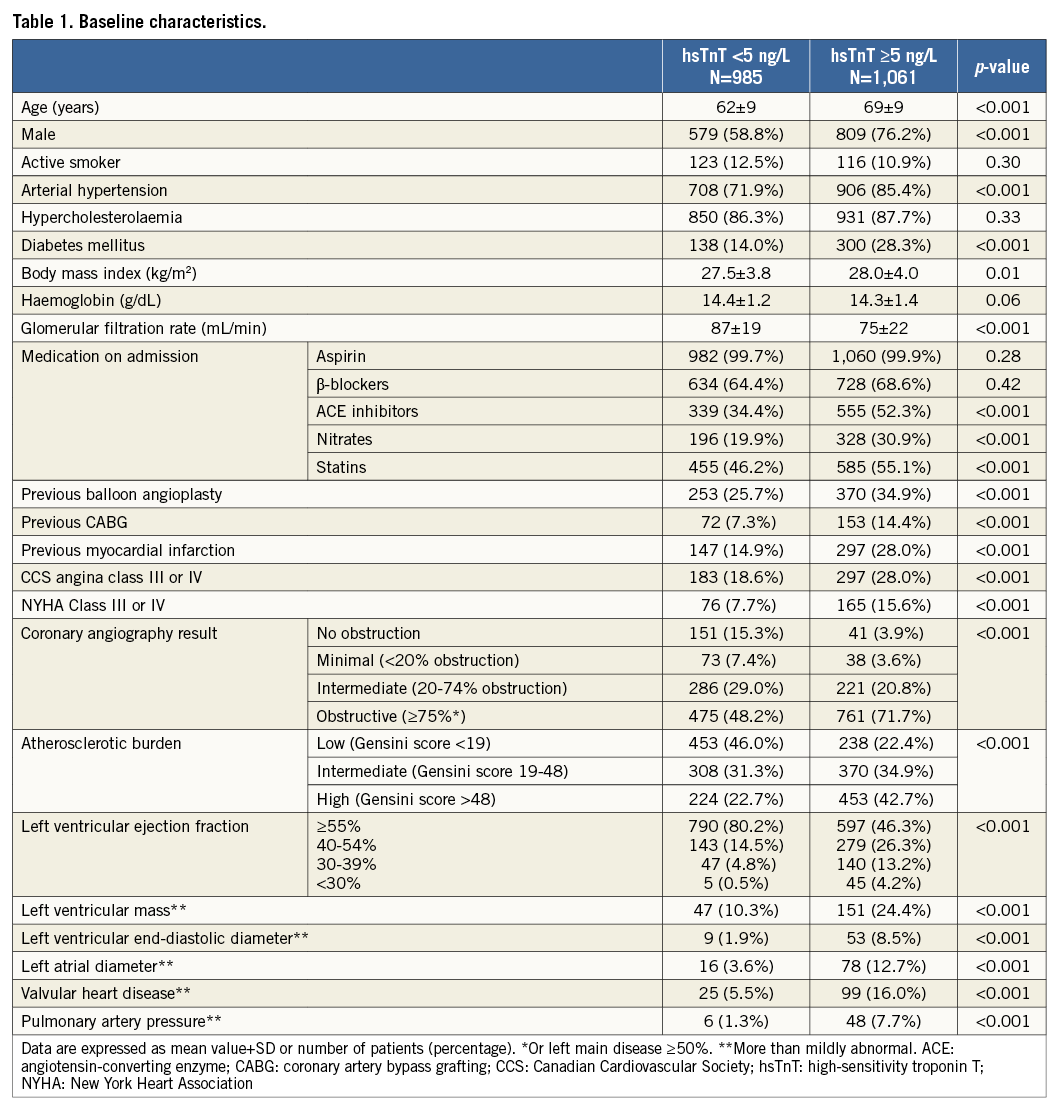
From the 15% of patients with hsTnT above the 99th percentile of a healthy population cut-off point, 19% were diagnosed without obstructive coronary heart disease.
UNADJUSTED ANALYSES
The distribution of troponin levels according to levels of various variables is shown in Figure 2 and Figure 3. For most variables, significant differences between different strata were found. However, these differences were numerically small for many of the evaluated variables. Only in patients with haemoglobin ≤10 g/dL, creatinine clearance of less than 30 ml/min, LV ejection fraction of less than 30%, severe valvular heart disease, or severe pulmonary hypertension were median hsTnT levels above the 99th percentile of a healthy population (14 ng/L).
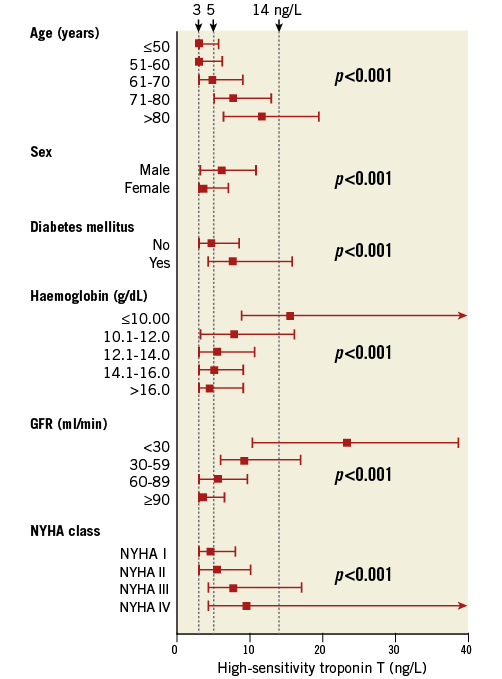
Figure 2. High-sensitivity troponin T level according to age, laboratory, and angiographic variables. Data presented as median with quartiles. GFR: glomerular filtration rate; NYHA: New York Heart Association
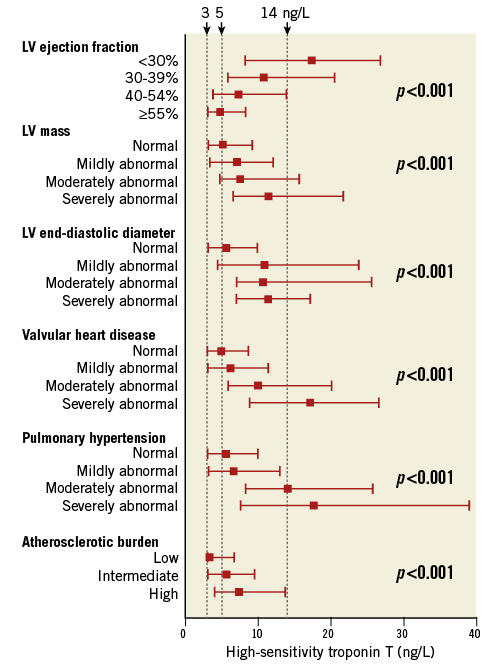
Figure 3. High-sensitivity troponin T level according to clinical variables. Data presented as median with quartiles. Atherosclerotic burden quantified by Gensini score. LV: left ventricular
ADJUSTED ANALYSES
To identify predictors generally available in clinical routine, the first multivariable model included only clinical variables. In this model, gender followed by age, renal function, diabetes, history of myocardial infarction, and haemoglobin levels were the variables most strongly associated with levels of cardiac troponin (Table 2). The second model included only angiographic and echocardiographic parameters. In this model, results of coronary angiography represented by Gensini score followed by LV ejection fraction, and LV mass demonstrated the highest strength of association with troponin levels.
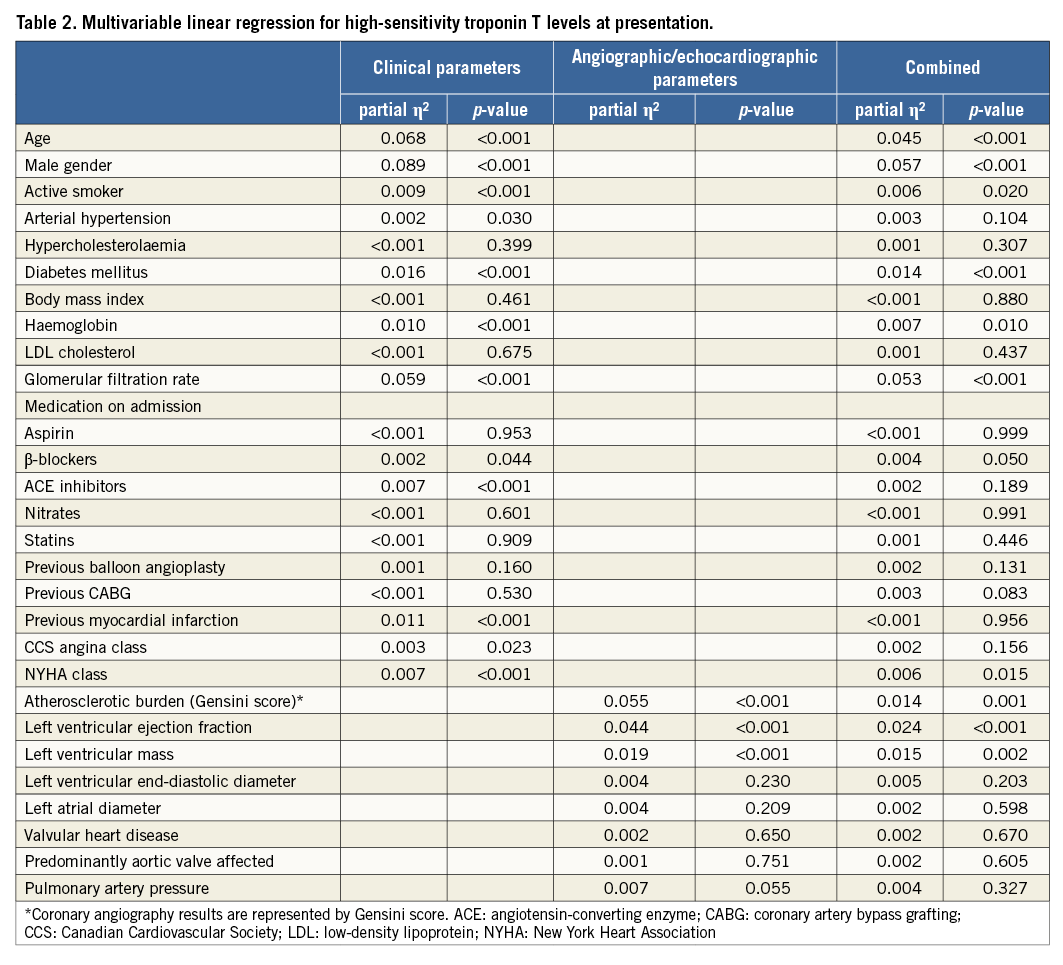
In the combined analysis of all available variables (3rd model), gender followed by renal function, age, LV ejection fraction, LV mass, diabetes, and coronary angiography results showed the strongest association with levels of hsTnT. Further independent predictors of levels of hsTnT were haemoglobin, NYHA class, and smoking status.
Discussion
The implementation of high-sensitivity cardiac troponin assays into clinical routine did not only improve the diagnosis of acute MI1, but also for the first time allowed the detection of troponin levels in a significant proportion of stable patients6-8. In some of these stable patients even troponin levels above the 99th percentile of a reference population were seen – the cut-off usually used for diagnosis of MI14. In patients presenting at an emergency department with acute diseases outside the setting of acute coronary syndromes, the proportion of patients with high-sensitivity cardiac troponin levels above the 99th percentile can be up to 44%19. Since elevated levels of troponin can indicate acute MI or at least increased risk of cardiovascular events7-9,11, many of these patients undergo coronary assessment, which might be unnecessary in a significant proportion of these patients.
The present study demonstrated that more than half of stable patients undergoing elective coronary angiography have detectable levels of cardiac troponin and approximately 15% of patients present with troponin levels even above the 99th percentile of a reference population – without having acute MI according to current definition14. Roughly 30% of patients with detectable levels of cardiac troponin and 20% of patients with troponin levels even above the 99th percentile did not have an obstructive coronary heart disease. Important features of the present analysis are the use of a large cohort with more than 2,000 patients, the availability of echocardiographic and angiographic data, and multivariable analyses identifying the strength of association of variables with levels of cardiac troponin. Key findings are that changes in cardiac troponin were statistically significant but numerically small for many variables. Only haemoglobin ≤10 g/dL, creatinine clearance of less than 30 ml/min, LV ejection fraction of less than 30%, severe valvular heart disease, and severe pulmonary hypertension were associated with median hsTnT levels above the 99th percentile of a reference population. Multivariable analyses demonstrated that strength of association weakened for multiple previously described variables after adjustment for clinical and imaging data. The variables most strongly associated with levels of cardiac troponin after adjustment were age, gender, renal function, and LV ejection fraction.
Several previous studies have investigated the association of levels of cardiac troponin with multiple variables. Cardiovascular disorders linked to elevations of troponin are, among others, left ventricular wall stress and dysfunction, heart failure with preserved ejection fraction, aortic stenosis, hypertension, acute heart failure, and coronary artery disease20-23. For example, a recent study demonstrated that more than 50% of patients with heart failure with preserved ejection fraction had troponin levels above the cut-off for diagnosis of myocardial infarction20. In patients with aortic valve disease, the mean level of cardiac troponin was found to be higher as compared to patients without aortic valve disease22. Troponin levels have also been associated with the severity of coronary artery disease outside the setting of acute coronary syndromes24, and with the presence of vulnerable plaques23. A recent imaging study using CT and SPECT demonstrated that levels of cardiac troponin can be used for discrimination of patients with and without structural heart disease in general25.
Apart from cardiovascular disorders, variables such as age, gender, renal function, chronic obstructive pulmonary disease, anaemia, and diabetes have been linked to elevated levels of cardiac troponin21,26-30. For example, patients with stable chronic obstructive pulmonary disease were found to have more than twofold higher levels of cardiac troponin as compared to the general population28. In the setting of acute exacerbation of chronic obstructive pulmonary disease, an approximately fourfold increase in levels of troponin was found as compared to patients with stable disease31. The mechanisms behind elevations of troponin in patients apparently without cardiovascular disease are not completely understood, but might include subclinical myocardial injury caused by stress, hypotension, or –as demonstrated by a recent analysis– impaired coronary flow reserve reflecting microvascular dysfunction32.
The results of the present analysis are in line with most of the previous findings. However, after adjustment for echocardiographic and angiographic parameters, several variables were not predictive for levels of hsTnT anymore such as drugs commonly prescribed for heart failure, history of myocardial infarction, and imaging parameters such as diameters, and valvular heart disease. Other parameters such as findings of coronary angiography demonstrated a weaker strength of association with levels of cardiac troponin after adjustment for clinical variables but prevailed as independent predictors. The variables most strongly associated with elevated levels were male gender followed by renal function, age, LV ejection fraction, diabetes, LV mass, and coronary status.
Limitations
This analysis is retrospective with all the adherent limitations. Since only patients admitted for elective coronary angiography were enrolled, the present data cannot be extrapolated to the overall population. Only parameters available from the clinical records could be analysed. Thus, transient and/or undiagnosed alterations such as hypertension or tachycardia not recorded by the staff and potentially leading to a rise in cardiac troponin cannot be fully excluded.
Conclusions
Approximately 15% of stable subjects admitted for elective coronary angiography present with hsTnT levels above the upper reference limit of normal. However, a fifth of these patients are not diagnosed with obstructive coronary heart disease. The variables most strongly associated with elevated levels were male gender followed by renal function, age, LV ejection fraction, diabetes, LV mass, and coronary status. The significant variation of troponin levels according to different variables shown in this analysis might provide some guidance for a more differentiated interpretation of this biomarker.
| Impact on daily practice Approximately 15% of stable subjects admitted for elective coronary angiography present with hsTnT levels above the upper reference limit of normal. However, a fifth of these patients are not diagnosed with obstructive coronary heart disease. The variables most strongly associated with elevated levels were male gender, renal function, age, LV ejection fraction, diabetes, and LV mass, followed by coronary status. Since, in daily routine, elevated levels of hsTnT are often seen as a trigger for invasive coronary assessment, the present data might provide some guidance for a more differentiated interpretation of the association of this biomarker with various clinical variables and outcomes. |
Funding
This work was supported by Roche Diagnostics by provision of laboratory kits for high-sensitivity troponin T.
Conflict of interest statement
C. Stratz reports receiving speaker’s honoraria from Eli Lilly. D. Trenk reports receiving speaker’s honoraria from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Daiichi Sankyo, Eli Lilly, MSD, and Pfizer; and consulting fees from AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly and Otsuka. M. Ferenc reports receiving speaker’s honoraria from AstraZeneca, Eli Lilly, Biotronik, Medtronic, Abbott Vascular, and Biosensors. W. Hochholzer reports receiving speaker’s honoraria from Daiichi Sankyo, AstraZeneca, and Boehringer Ingelheim. The other authors have no conflicts of interest to declare.

