Abstract
Aims: We sought to evaluate rates and mechanisms of myocardial injury and type 4a myocardial infarction (MI) after an elective diagnostic coronary angiography (CAG) as detected by high-sensitivity cardiac troponin T (hsTnT) assay.
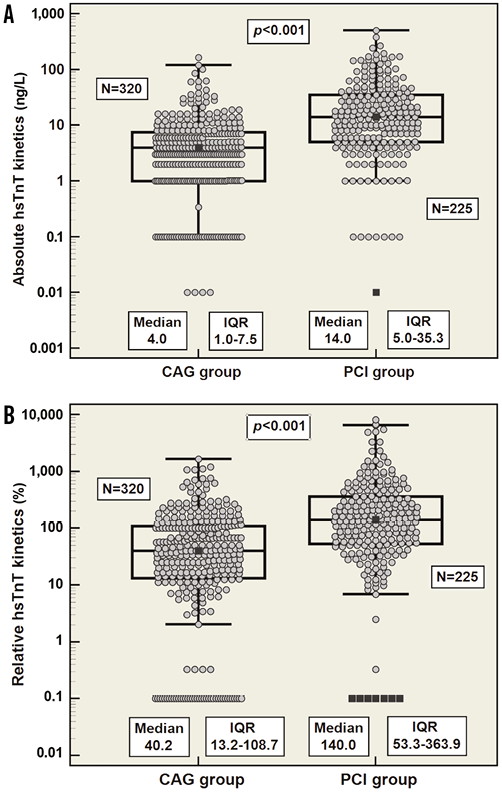
Methods and results: Cardiac troponin concentrations were measured in consecutive patients before and after undergoing an elective CAG –with or without coronary intervention (PCI)– using an hsTnT assay. The study population consisted of 545 patients: 320 (58.7%) patients received only an elective CAG and another 225 patients (41.3%) received an additional PCI. Significant hsTnT increases occurred in 97 (30.3%) cases within the CAG group and in 152 (67.6%) cases within the PCI group. Rates of normal baseline hsTnT values (<99th percentile upper reference limit) were 75.9% in the CAG group and 71.6% in the PCI group. In cases with normal baseline hsTnT values, peak levels meeting criteria of MI type 4a according to the second or third version of the universal MI definition were observed in five (1.6%) and one (0.3%) cases within the CAG group, as well as in 32 (14.2%) and 22 (9.8%) cases within the PCI group, respectively.
Conclusions: Use of the hsTnT assay may allow identification of myocardial injury during an uneventful diagnostic coronary angiography in the absence of any coronary or non-coronary interventions.
Abbreviations
CAD: coronary artery disease
CAG: coronary angiography
CT: computed tomography
cTn: cardiac troponin
ECG: electrocardiogram
hsTnT: high-sensitivity troponin T
IQR: interquartile range
LV: left ventricular
LVEF: left ventricular ejection fraction
MI: myocardial infarction
PCI: percutaneous coronary intervention
URL: upper reference limit
Introduction
Cardiac troponin (cTn) is regarded as the biochemical reference standard for the diagnosis of myocardial infarction (MI)1. The substantially higher analytical sensitivity of novel assays now allows detection of hitherto undetectable cTn levels in the absence of MI in an apparently healthy population, which stimulates new hypotheses for the mechanisms of myocardial injury2.
Troponin elevations after percutaneous coronary intervention (PCI) are common3. Mechanisms include incidental minor side branch occlusion or microvascular obstruction from distal embolisation of plaque contents including platelets, thrombus, and/or atheroma4, which all lead to myonecrosis, myocardial injury or MI type 4a1.
Occasionally, increases of cTn are noted among patients undergoing diagnostic coronary angiography (CAG) with unclear frequency and mechanisms. Therefore, we sought to investigate rates and potential mechanisms for myocardial injury or MI type 4a among patients undergoing elective CAG.
Methods
STUDY DESIGN
This prospective study (NCT01735500) included consecutive patients scheduled for elective CAG at the Cardiology Department of Heidelberg University Hospital between February and November 2010. Patients who presented with signs of acute coronary syndrome or who received any additional intervention or instrumentation other than PCI (e.g., myocardial biopsy) were excluded, as cTn release is likely to occur due to direct myocardial trauma. Upon procedure, patients were classified into the CAG or the PCI group. All procedure-related decisions including PCI were left to the discretion of the interventional cardiologist.
High-sensitivity troponin T (hsTnT) was measured before (baseline), as well as three to six and 12-24 hours after CAG. Peak value was defined as the highest post-procedural measurement. A 12-lead electrocardiogram (ECG) was registered before and after the procedure, and patients were asked actively for angina onset.
LABORATORY MEASUREMENTS
cTn was measured on Cobas® E411 using a novel hsTnT assay (Roche Diagnostics, Rotkreuz, Switzerland). The 99th percentile value (upper reference limit [URL]) was determined at 14 ng/L5. Kinetic metrics were calculated from serial measurements including relative δ-change ([hsTnTpeak-hsTnTbaseline]/hsTnTbaseline×100) given as percentage change from baseline, and absolute δ-change between highest post-procedural hsTnT concentration and baseline (hsTnTpeak-hsTnTbaseline) expressed as ng/L.
A relevant increase of normal baseline hsTnT was defined as an elevation above the 99th percentile URL. Values and concentration changes below the URL were disregarded due to considerable assay imprecision below the level of quantitation (13 ng/L). For baseline hsTnT values >URL, a relative kinetic change (rise/fall) of 20% or more has been recommended to discriminate acute from chronic cTn elevations1.
STATISTICAL METHODS
Continuous data were expressed as mean±standard deviation (SD) or as median (interquartile range [IQR]) if not distributed normally (Kolmogorov-Smirnov test). Group comparison was performed either by the t-test or by the two-tailed Mann-Whitney test, as appropriate. Categorical variables were expressed as absolute number (percent) and were tested using the χ2 or Fisher’s exact test. Rank correlation was carried out using Spearman’s test. Associations between cTn releases and clinical and procedure-related variables were tested using univariate or multivariate logistic regression analysis. All tests were two-tailed and p-values <0.050 were considered statistically significant. Statistical analysis was carried out using MedCalc®, Version 12.2.1.0 (MedCalc, Mariakerke, Belgium).
CORONARY ARTERY DISEASE
In order to investigate the association between cTn releases and the extent of coronary artery disease (CAD), SYNTAX score values and risk categories (low: <23 points, intermediate: 23-32 points, high: >33 points) were calculated6. Coronary lesions were also categorised according to the ACC/AHA classifications.
SYNTAX score and ACC/AHA lesion types were assessed in cases within the CAG group with at least one coronary lesion with ≥50% luminal obstruction and normal baseline hsTnT.
PCI-RELATED MYOCARDIAL INFARCTION (MI TYPE 4a)
According to the second universal definition of MI, MI type 4a is arbitrarily defined by an elevation of cTn >3x URL7. In the current third version, MI type 4a is defined as an elevation of cTn values >5x URL, or a rise of cTn >20% if baseline values are elevated and stable or falling. In addition, symptoms, ECG changes, angiographic findings or imaging evidence of new loss of viable myocardium are required1.
Results
A total of 545 consecutive patients were enrolled in this study. The clinical and angiographic characteristics of the study population subdivided into CAG group and PCI group are shown in Table 1.
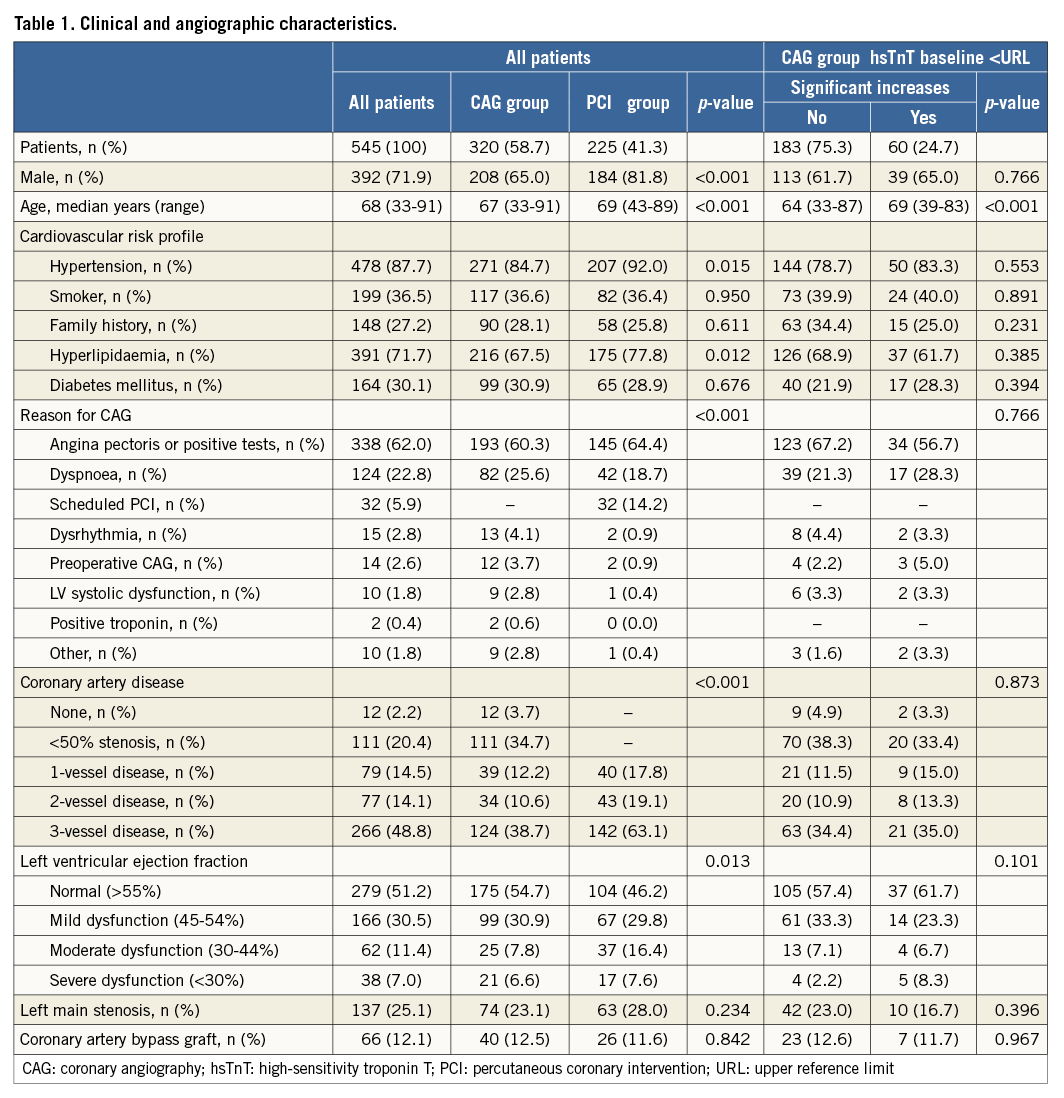
Upon procedure, patients were classified into CAG group and PCI group. Based on the 99th percentile URL, patients were further characterised according to baseline hsTnT values. In the entire study population, baseline hsTnT median was 8 ng/L (IQR 4-15 ng/L) without significant differences between the CAG group and the PCI group. Rates of baseline hsTnT values >URL were 21.4% and 28.4%, respectively. As compared to patients with normal baseline hsTnT values, those with elevations at baseline were significantly older (median age 73 [IQR 66-80] years vs. 66 [IQR 59-72] years, p<0.001), more often had CAD with stenosis ≥50% (84.4% vs. 75.0%, p=0.029), and more frequently had moderate to severe systolic left ventricle dysfunction (34.0% vs. 12.9%, p<0.001) and impaired renal function (creatinine clearance <60 ml/min/1.73 m2) (51.1% vs. 16.6%, p<0.001).
DIAGNOSTIC CORONARY ANGIOGRAPHY GROUP (CAG GROUP)
Three hundred and twenty patients (58.7%) received an elective CAG without additional PCI. Relevant increases of hsTnT occurred in 97 (30.3%) cases. Within this group, 243 cases (75.9%) had normal baseline hsTnT, of which 60 cases (24.7%) had significant hsTnT increases (Figure 1A). In 55 cases, hsTnT peak values increased from normal baseline values to the range of 1 to 3x URL. An elevation of hsTnT >3x URL was observed in four cases. One patient had an hsTnT elevation >5x URL but did not qualify for an MI type 4a diagnosis according to the third universal definition of MI due to the absence of additional indicators of myocardial ischaemia.
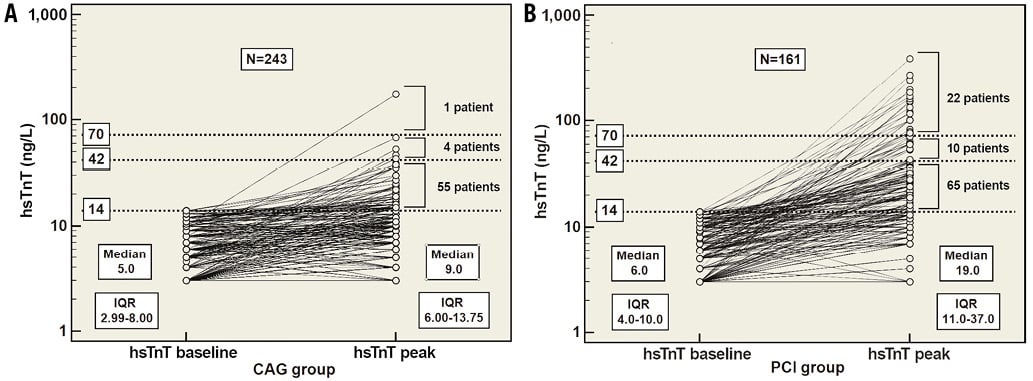
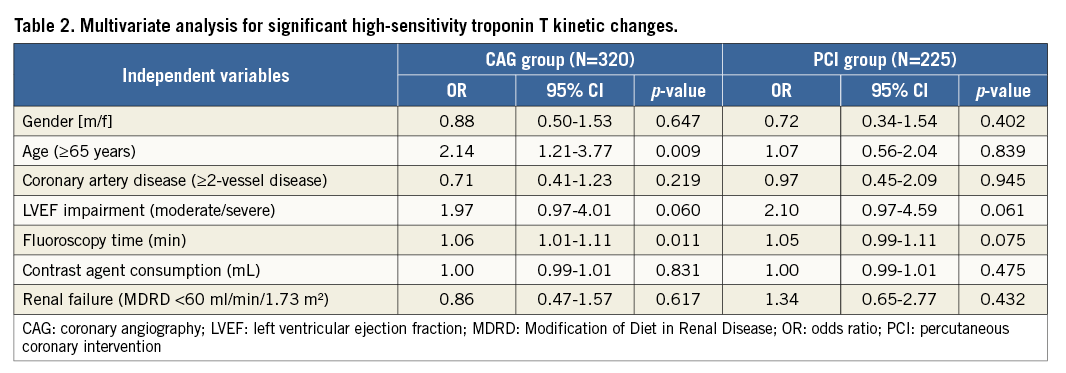
Figure 1. hsTnT level changes. A) CAG group, B) PCI group. Baseline hsTnT values CORONARY INTERVENTION GROUP (PCI GROUP) A total of 225 patients (41.3%) received a CAG with additional PCI. Drug-eluting stents (84.4%) were more frequently used. Almost half of the PCI patients (46.7%) received a single stent, and only in five cases (2.2%) did the PCI attempt end unsuccessfully. As anticipated, there was a significantly higher number of hsTnT increases within the PCI group than in the CAG group. Relevant post-interventional hsTnT increases were detected in 152 (67.6%) cases. One hundred and sixty-one cases (71.6%) had normal baseline hsTnT values, out of which 65 cases had peak hsTnT values beyond the 99th percentile URL but still below the 3x URL (42 ng/L). In 32 cases, peak hsTnT values increased beyond 3x URL (42 ng/L) and in 22 cases above 5x URL (70 ng/L) (Figure 1B). Of these 22 cases, post-procedural ischaemic ECG changes were noted in two cases and chest pain in another two cases. Angiographic evidence of incidental minor side branch occlusion associated with chest pain was registered in a single case. No imaging proof of new loss of viable myocardium was obtained. RELATIVE AND ABSOLUTE hsTnT KINETIC CHANGES Relative and absolute hsTnT δ-changes were calculated separately for both the CAG group and the PCI group. Initially, patients (n=404) with normal baseline hsTnT values were separately investigated; subsequently, all patients (n=545) were tested, with quite a comparable performance of the two approaches overall (Figure 2). CORONARY ARTERY DISEASE The SYNTAX score could be calculated in 108 patients within the CAG group: these were classified into low- (62%), intermediate- (14.8%) and high-risk (23.2%) categories. Both absolute (rho=0.057, p=0.557) and relative (rho=0.044, p=0.653) hsTnT δ-changes did not correlate well with the raw SYNTAX score. Further, 26 cases (24.1%) were sub-selected upon the defining criteria for relevant hsTnT changes, yet no significant association with the SYNTAX score was revealed. Moreover, the most narrowed coronary lesions were categorised according to the ACC/AHA classification (A - 11.1%, B1 - 14.8%, B2 - 38.9%, C1 - 22.2%, C2 - 13.0%). Spearman’s rank correlation coefficients (rho) were -0.0232 (p=0.811) for absolute and -0.0357 (p=0.714) for relative hsTnT changes, showing no association between hsTnT level changes and coronary lesion types. RADIOGRAPHIC CONTRAST AGENT Iomeprol (Imeron® 350; Bracco Imaging Deutschland GmbH, Constance, Germany) was used as radiographic contrast agent. A median of 100 mL (IQR 90-120 mL) was used in the CAG group and 200 mL (IQR 150-250 mL) in the PCI group. Absolute hsTnT δ-changes correlated significantly (r=0.016, p=0.001) with the contrast agent consumption within the CAG group. The correlation was significant, albeit less impressive, for relative hsTnT δ-changes (r=0.034, p=0.022). MULTIVARIATE ANALYSIS The logistic regression analysis was executed separately for the CAG group and for the PCI group (Table 2). Within the CAG group, there was a significant association between cTn level changes and fluoroscopy time and age >65 years. However, gender, renal dysfunction and angiographic variables, including multivessel coronary disease, impaired left ventricular ejection fraction (LVEF) and contrast agent consumption, were not predictive for cTn increases. On the other hand, there were no independent predictors found in the PCI group. Discussion The pathomechanism of cardiac troponin release in the absence of myocardial infarction is still unsettled. Some mechanisms have been suggested, such as apoptosis8, normal turnover of myocardial cells9, cellular release of troponin degradation products10, increased cellular wall permeability10,11, formation and release of membranous blebs11, and myocyte necrosis12. Reversible myocardial ischaemia, such as in strenuous cardiac exercise, has been quoted as a potential reason for transient cardiac ischaemia resulting in temporal membrane leakage or bleb formation that allows extrusion of cTn into the bloodstream11,13-15. Still, it remains controversial whether transient myocardial ischaemia may lead to a rise of troponin in the absence of MI16. Further potential reasons include myocardial injury due to pressure or volume overload and myocardial toxicity. Nevertheless, little is known about the incidence, magnitude, pathomechanism and prognostic role of cTn elevations after an uncomplicated diagnostic CAG. The major finding of this single-centre study is that myocardial injury –as detected by hsTnT assay– is common after diagnostic CAG. The causes as to why myocardial injury occurs during an uneventful CAG are largely unclear. Our findings from the multivariate analysis suggest an independent association between hsTnT increases and older age and increasing fluoroscopy time as an indicator for a prolonged examination. Other mechanisms such as embolisation of platelet microaggregates, intracoronary thrombus, or air embolisation during contrast injection are likely, but cannot be suitably addressed as CAG is less sensitive for the detection of intracoronary clot than angioscopy17, and this would lead to underdiagnosis of the presence of intracoronary thrombus, and poorer visualisation of peripheral embolisation of platelet aggregates, clots, cholesterol particles, plaque debris or air. RADIOGRAPHIC CONTRAST MEDIUM This study reveals a direct association between absolute and relative hsTnT δ-changes and volume of injected contrast agent. Interestingly, this was not the case in the regression analysis after correction for the clinical and angiographic variables. Nevertheless, contrast material may cause myocardial injury due to interference with the microvascular coronary blood flow18, increased blood viscosity19, thrombogenicity20,21, or induction of reactive oxygen species22. Iomeprol is a triiodinated, non-ionic, monomeric radiographic contrast medium, which has been demonstrated to have low chemotoxicity, osmolality, viscosity and high water solubility23. In comparison to ionic contrast media, non-ionic agents have been reported to have less but existing myocardial toxicity and were not associated with the biochemical changes of cellular ischaemia24. In other observations, ionic contrast agents were linked to thromboembolic complications throughout CAG20, and were suggested to have a direct activating effect on platelets21. Another study proposed thrombotic risk as being more probably related to operator experience and type of procedure25. Further, the viscosity of contrast media seems to have an indirect impact itself, so that higher medium viscosity requires the use of larger catheters with larger lumina19. This might increase the mechanical vascular or myocardial trauma through catheter manoeuvring. Furthermore, higher-viscosity contrast media require higher injection pressure to be forced through small catheters, which would translate into a higher intravascular flow pressure. Possible vulnerable coronary plaques are in danger of rupturing on the one hand, with a theoretically enhanced possibility of microembolism on the other. SEVERITY OF THE CORONARY ARTERY DISEASE We found no correlation between hsTnT concentration changes and coronary lesion types according to the ACC/AHA classification, or CAD complexity as reflected through the SYNTAX score. Previously, an association had been reported between hsTnT concentrations and plaque morphology as delineated using multislice coronary computed tomography (CT), suggesting an association between low range elevations of hsTnT and plaque instability26. The reasons for this discrepancy are unclear, but could be related to the different methodology for assessment of plaque morphology between CT and the angiography-derived SYNTAX score, as well as exclusion of patients with coronary lesions with <50% stenosis. Thus, the contribution of early stage coronary atherosclerosis to myocardial injury was not investigated. De Bruyne et al27 reported that early stage coronary atherosclerosis without focal stenosis, which usually remains invisible at angiography, is often associated with abnormal resistance of the epicardial coronary arteries before a segmental stenosis is apparent at angiography, resulting in a continuous decline of pressure gradient and reduction of coronary flow reserve, potentially causing myocardial ischaemia and abnormal perfusion during exercise or pharmacological vasodilation. OTHER PREDICTORS FOR CARDIAC TROPONIN RELEASES For as yet unknown reasons, elderly patients show a trend towards more myocardial injury during CAG, even after correction for renal function, volume of contrast material and fluoroscopy time. Ventricular compliance has been reported to decline with age, whilst the prevalence of diastolic dysfunction or heart failure in the presence of preserved ejection fraction is increasing in elderly patients28. In addition, patients with a depressed LVEF seem to be more likely to develop myocardial injury. Potential reasons include increased left ventricular (LV) strain due to an acute increase of LV volumes and pressure, which could result in release of troponin in the absence of myocardial ischaemia due to myocardial injury in consequence of ventricular wall tension29. Further, it has been assumed that progressive myocardial wall stress may lead to decreased subendocardial perfusion, leading to troponin elevation and decline in LV systolic function15,28,29. Based on this theory, myocardial strain and increased preload have been reported as potential mechanisms for troponin release in acute30 and chronic heart failure31, aortic stenosis32, hypertensive crisis33, and pulmonary embolism34. RATES OF MYOCARDIAL INJURY AND INFARCTION TYPE 4a ACCORDING TO THE SECOND OR THIRD VERSION OF THE UNIVERSAL DEFINITION OF MI According to the second version of the universal definition of MI, the incidence of significant cTn increases within the CAG group and PCI group was 30.3% and 67.6%, respectively, while MI type 4a occurred in five (2.1%) and 32 (19.9%) cases with baseline cTn values <99th percentile URL, respectively. Applying the current third version of the MI definition abolished the diagnosis of MI type 4a within the CAG group, while five (3.1%) cases within the PCI group continued to be classified as MI type 4a. Myocardial injury was still observed in cases with normal baseline values in 60 (24.7%) cases within the CAG group and in 92 (57.1%) cases within the PCI group. Upon applying the criteria of the third universal definition of MI, fewer procedure-related cTn elevations are now being diagnosed with MI type 4a, resulting in an increased labelling of these cTn kinetics as myocardial injury. Limitations This study was not intended to provide prognostic data but had the primary scope to investigate incidence and mechanisms behind troponin release after diagnostic coronary angiography. The SYNTAX score was assessed only in the CAG group for patients with normal baseline hsTnT values upon SYNTAX selection criteria. SYNTAX score was not assessed within the PCI group; thus, a possible correlation between SYNTAX score values or risk categories and PCI-related cTn increases has yet to be investigated. Conclusions Use of novel high-sensitivity cTn assays allows detection of myocardial injury in different new settings. The mechanisms for hsTnT increases following diagnostic coronary angiography remain unclear, although our findings provide several hypotheses that need to be substantiated in forthcoming studies. Our findings underline the capability of hsTnT for sensitive and accurate detection of myocardial injury and thus may be helpful for our understanding of pathophysiological processes associated with the progression of atherosclerosis. Impact on daily practice The substantially higher analytical power of novel high-sensitivity cardiac troponin assays allows detection of hitherto undetectable cTn levels in different clinical settings. The major finding of this study is that cTn releases are common after an apparently uneventful diagnostic coronary angiography. Therefore, several hypotheses were debated that could be helpful in understanding this process. Moreover, rates of myocardial injury and type 4a infarction were analysed upon applying the criteria of the second and third universal definitions of MI, which demonstrated that currently fewer procedure-related cTn elevations are being diagnosed with MI type 4a, resulting in an increased labelling of these cTn kinetics as myocardial injury, which might require more attention and adjusted therapy modalities. Conflict of interest statement E. Giannitsis has received financial support for clinical trials from Roche Diagnostics Ltd., Switzerland. He is consultant to Roche Diagnostics and BRAHMS Biomarkers and has received speaker’s honoraria from Roche Diagnostics, Siemens Healthcare, BRAHMS Biomarkers, and Mitsubishi Chemicals. H.A. Katus has developed the cTnT assay and holds the patent jointly with Roche Diagnostics. He has received grants and research support from several companies and lecture honoraria from Roche Diagnostics. The other authors have no conflicts of interest to declare.