Abstract
Aims: Periprocedural myocardial injury (PMI) is frequently observed after percutaneous coronary interventions (PCI) for chronic total occlusion (CTO). We aimed to investigate the prognostic impact of PMI with the antegrade as compared to the retrograde crossing technique.
Methods and results: A total of 1,909 patients undergoing CTO PCI were stratified according to the presence/absence of PMI (elevation of cardiac troponin T [cTnT] >5x99th percentile of normal), and divided according to tertiles of the difference between peak and baseline cTnT within 24 hours (∆cTnT). The primary endpoint was all-cause mortality at a median follow-up of 3.1 (interquartile range 3.0-4.4) years. PMI occurred in 19.4% and 25.4% after antegrade (n=1,447) and retrograde (n=462) procedures (p<0.001). PMI was significantly associated with mortality after antegrade (adjusted HR 1.39, 95% CI: 1.02-1.88, p=0.04), but not retrograde CTO PCI (adjusted HR 0.93, 95% CI: 0.53-1.63, p=0.80, pint=0.02). With the antegrade, but not with the retrograde approach, mortality also increased with tertiles of ∆cTnT (T1: 11.0%, T2: 18.6%, T3: 21.6%, log-rank p<0.001).
Conclusions: Periprocedural myocardial injury was significantly associated with all-cause mortality following antegrade, but not retrograde CTO PCI. Hence, the higher risk of PMI following retrograde procedures did not translate into worse survival.
Abbreviations
CI: confidence interval
cTnT: cardiac troponin T
CTO: chronic total occlusion
HR: hazard ratio
OR: odds ratio
PCI: percutaneous coronary intervention
PMI: periprocedural myocardial infarction
SD: standard deviation
Introduction
Chronic total occlusions (CTO) are frequently encountered in patients with significant coronary artery disease1,2. Although the development of novel devices and the advances in procedural techniques in recent years, along with accumulating operator experience, have substantially increased procedural success rates in this particularly challenging patient subset, technical complexity and complication rates remain higher as compared to percutaneous coronary intervention (PCI) in non-occluded vessels3.
Some degree of myocardial injury, mostly caused by side branch occlusion or distal embolisation and mirrored by cardiac biomarker release, is frequently observed after coronary revascularisation procedures. Also, minor asymptomatic increases of cardiac biomarker levels have been associated with worse clinical outcomes4,5. In those undergoing CTO PCI, periprocedural myocardial infarction (PMI) is reported to occur in about 10% of patients6,7, with an increased prevalence observed with the retrograde as compared to the antegrade crossing technique6,8-10. However, the clinical relevance of PMI following CTO PCI is the subject of controversial debate6,11,12. Data in this patient subset are scarce and mostly limited to rather small patient cohorts and short-term follow-up. Further, whether PMI differentially affects outcomes following antegrade as compared to retrograde procedures is still uncertain.
The aim of this study was therefore to assess the clinical significance of PMI in patients undergoing CTO PCI comparing antegrade versus retrograde crossing techniques.
Methods
STUDY DESIGN
We interrogated our clinical database, enrolling patients undergoing elective PCI at our institution for inclusion in the CTO registry13-15. A total of 1,909 stable patients who underwent elective PCI for at least one CTO between January 2005 and December 2013, who had baseline and post-procedural troponin levels available, and who survived to hospital discharge without cardiac tamponade or need for coronary artery bypass grafting, were included in this analysis (Figure 1). All information derived from the standardised follow-up protocol, hospital admission records, the referring physician, or from the outpatient clinic is entered into our clinical database. Blood samples were collected at baseline, as well as at 6, 8, and 24 hours after the procedure. All procedures were performed by highly experienced CTO operators. The decision to perform CTO PCI was based on angina symptoms and/or the presence of viable myocardium (on cardiac magnetic resonance imaging) or inducible ischaemia (on stress echocardiography or myocardial perfusion scintigraphy). Informed consent was obtained from each patient and the study was approved by our institution’s ethics committee. The study conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
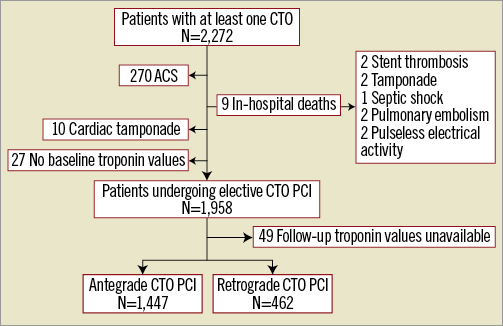
Figure 1. Study flow chart. ACS: acute coronary syndrome; CTO: chronic total occlusion; PCI: percutaneous coronary intervention
Patients were stratified according to the presence/absence of PMI16, and were further divided into tertiles (T1, T2, T3) based on the difference between peak conventional (2005-2009, n=1,017) or high-sensitivity cardiac troponin T (2010-2013, n=891) values within 24 hours and the baseline values (∆cTnT)17.
DEFINITIONS
Chronic total occlusion was defined as total occlusion of a coronary artery (Thrombolysis In Myocardial Infarction [TIMI] flow grade 0) of ≥3 months18. Occlusion duration was estimated based on the onset of angina symptoms, known myocardial infarction in the territory of the occluded vessel, and comparison with previous angiograms if available. Procedural success was defined as successful CTO recanalisation with antegrade blood flow (TIMI flow grade 3) and residual diameter stenosis of ≤30% by visual assessment on coronary angiogram. Periprocedural myocardial injury was defined as elevation of cTnT values >5x99th percentile URL according to the third universal definition of myocardial infarction16. The primary endpoint was all-cause mortality.
STATISTICAL ANALYSIS
Continuous variables are expressed as mean±standard deviation (SD) or median (interquartile range), and categorical variables reported as numbers (%). The Kolmogorov-Smirnov test was used to test for normality of distribution. Continuous variables were tested for differences with the unpaired Student’s t-test or the Mann-Whitney U test, and categorical variables with the Pearson’s χ² or the Fisher’s exact test. Survival curves for time-to-event variables were generated with the Kaplan-Meier method, and the log-rank test was used to provide a formal statistical assessment of the differences between groups. Univariable and multivariable logistic regression and Cox proportional hazards models were utilised to determine independent predictors of the outcome variables. The following preselected variables known to be associated with outcomes following CTO PCI were included in the multivariable models: age, diabetes, prior myocardial infarction, prior coronary artery bypass grafting, left ventricular systolic dysfunction (left ventricular ejection fraction <40%), estimated glomerular filtration rate (Cockcroft Gault formula), multivessel disease, moderate/severe calcifications, and procedural success. The Cox proportional hazards regression test of interaction (presence/absence of PMI status by antegrade/retrograde procedure status) was used to investigate differential effects of periprocedural myocardial injury by the crossing technique. A two-sided p-value of <0.05 was considered statistically significant. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS), Version 21 (IBM Corp., Armonk, NY, USA).
Results
PATIENT AND PROCEDURAL CHARACTERISTICS
Median age was 66 (57-73) years (83.8% male). Baseline characteristics according to the crossing technique and the presence/absence of PMI are given in Table 1. Antegrade and retrograde procedures were performed in 1,447 (75.8%) and 462 (24.2%) patients, respectively. The use of the retrograde approach increased significantly during the course of the registry (2005-2007: 27 [5.8%], 2008-2010: 91 [19.7%], 2011-2013: 344 [74.5%]) as compared to the antegrade approach (2005-2007: 583 [40.3%], 2008-2010: 395 [27.3%], 2011-2013: 469 [32.4%]; p<0.001).
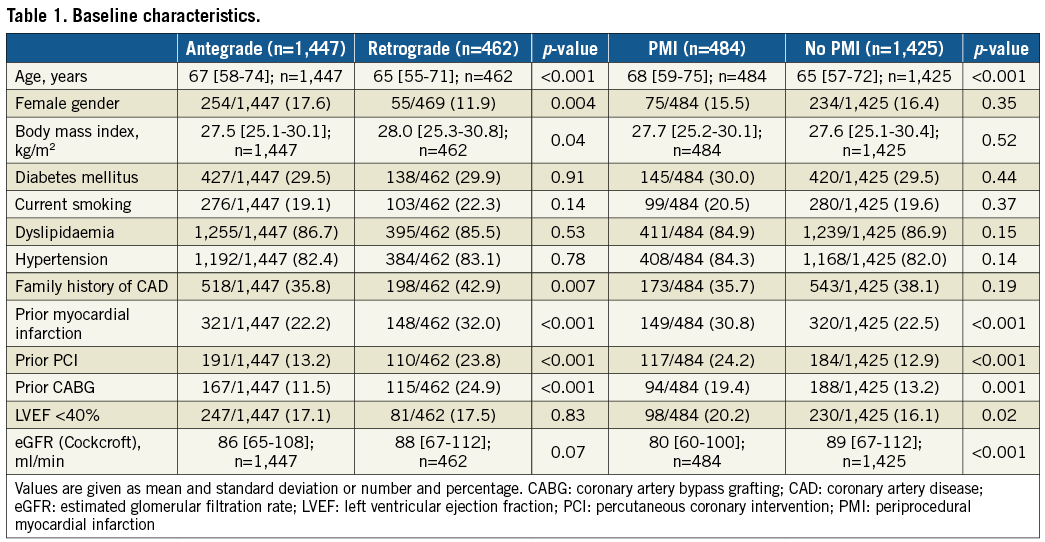
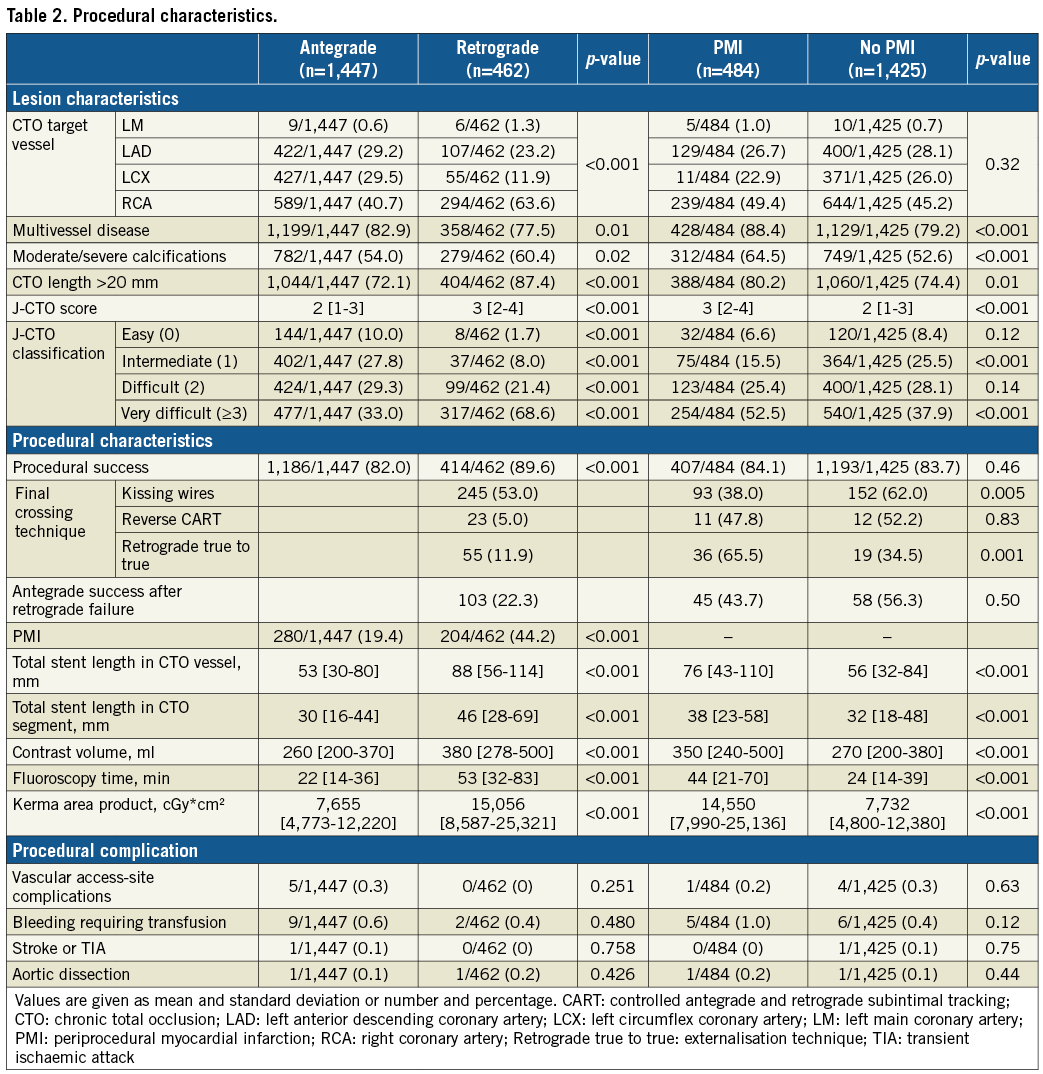
Procedural success was achieved in 82.0% and 89.6% of patients in the antegrade and retrograde groups (p<0.001), and in 84.1% and 83.5% of patients with and without PMI (p=0.46) (Table 2).
PERIPROCEDURAL MYOCARDIAL INJURY
Periprocedural myocardial injury occurred in 19.4% and 44.2% of patients after antegrade and retrograde CTO PCI (p<0.001), and in 25.4% and 24.9% of successful and unsuccessful procedures (p=0.89). The degree of post-procedural cTnT increase according to the crossing technique is displayed in Figure 2.
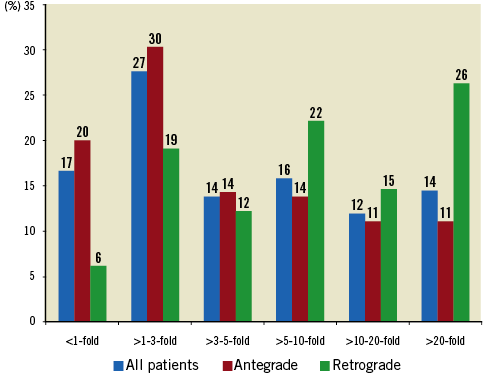
Figure 2. Degree of cardiac troponin T (cTnT) increase after percutaneous coronary intervention (PCI) for chronic total occlusion (CTO). Percentages of patients are shown in the total patient cohort as well as divided according to the crossing technique (antegrade and retrograde).
In the antegrade group, multivessel disease (odds ratio [OR] 2.39, 95% CI: 1.68-3.38, p<0.001), age (OR 1.02, 95% CI: 1.01-1.03, p=0.002), and lower body mass index (OR 0.97, 95% CI: 0.95-1.00, p=0.03) emerged as independent predictors of an increased troponin release (∆cTnT T3). In the retrograde group, moderate to severe calcifications (OR 2.00, 95% CI: 1.10-3.51, p=0.023) and fluoroscopy time (OR 1.04, 95% CI: 1.03-1.05, p<0.001) independently predicted an increased troponin release (∆cTnT T3).
LONG-TERM CLINICAL OUTCOMES
Median follow-up was 3.1 (interquartile range 3.0-4.4) years. All-cause mortality was 17.0% and 12.8% in the antegrade and retrograde groups (adjusted HR 0.87, 95% CI: 0.65-1.17, p=0.35). In the entire cohort, PMI emerged as an independent predictor of mortality (unadjusted hazard ratio [HR] 1.70, 95% CI: 1.31-2.20, p<0.0001; adjusted HR 1.31, 95% CI: 1.03-1.70, p=0.047).
In the antegrade group, all-cause mortality was higher in patients with PMI as compared to those without (21.8% vs. 15.9%, log-rank p<0.001), but no significant differences were observed in the retrograde group (11.8% vs. 13.6%, log-rank p=0.79) (Figure 3). Periprocedural myocardial injury was identified as an independent predictor of all-cause mortality after antegrade (adjusted HR 1.39, 95% CI: 1.02-1.88, p=0.04), but not retrograde procedures (adjusted HR 0.93, 95% CI: 0.53-1.63, p=0.80). There was a significant interaction of antegrade/retrograde procedure status and PMI status on all-cause mortality (interaction p=0.02) (Figure 4). Similar results were obtained when including only patients with successful CTO recanalisation in the analysis (antegrade CTO PCI: adjusted HR 1.43, 95% CI: 1.00-2.04, p=0.047, and retrograde CTO PCI: adjusted HR 1.00, 95% CI: 0.54-1.85, p=0.98, interaction p=0.05) (Figure 4). These results were confirmed when excluding the initial experience (2005 to 2007) from the analyses (antegrade CTO PCI: adjusted HR 1.94, 95% CI: 1.31-2.86, p<0.001, and retrograde CTO PCI: adjusted HR 0.93, 95% CI: 0.53-1.66, p=0.81, interaction p<0.001).
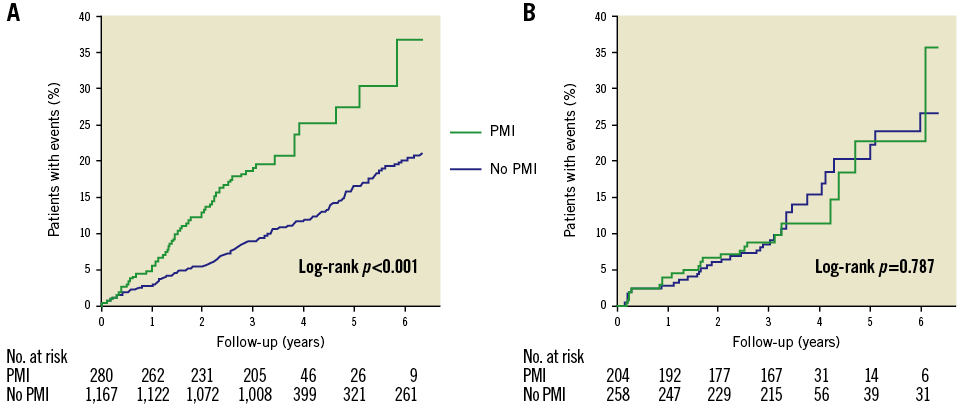
Figure 3. Kaplan-Meier estimates for all-cause mortality in patients after antegrade and retrograde percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) stratified according to the presence or absence of periprocedural myocardial injury. A) Antegrade patient cohort. B) Retrograde patient cohort.
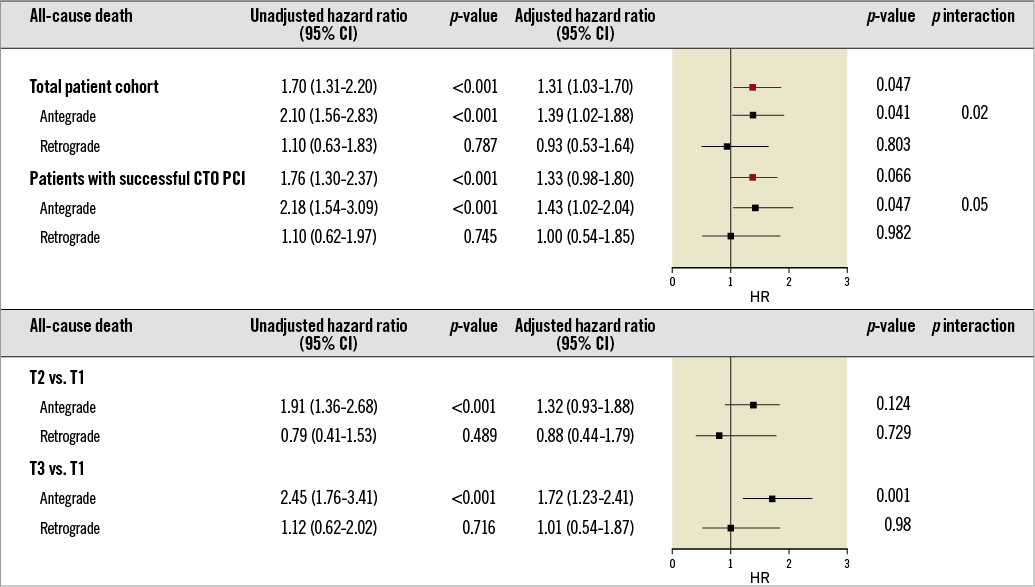
Figure 4. Forest plot showing hazard ratios for all-cause mortality associated with periprocedural myocardial damage stratified for antegrade and retrograde recanalisation of chronic coronary total occlusion. CI: confidence interval; CTO PCI: percutaneous coronary intervention for chronic total occlusion; PMI: periprocedural myocardial injury
In the antegrade group, all-cause mortality increased with higher ∆cTnT tertiles (T1: 11.0%, T2: 18.6%, T3: 21.6%, log-rank p<0.001), but the level of troponin release did not affect all-cause mortality in the retrograde group (T1: 14.2%, T2: 9.9%, T3: 14.2%, log-rank p=0.51) (Figure 5). In multivariate analysis, belonging to the highest troponin tertile (∆cTnT: T3 vs. T1) significantly predicted all-cause mortality after antegrade CTO PCI (adjusted HR 1.72, 95% CI: 1.23-2.41, p=0.001) (Figure 4). When including continuous ∆cTnT values in the multivariate model, increased troponin release was independently associated with all-cause mortality after antegrade CTO PCI (adjusted HR 1.42, 95% CI: 1.08-1.88, p=0.01). Neither belonging to the highest troponin tertile (∆cTnT: T3 vs. T1, adjusted HR 1.01, 95% CI: 0.54-1.87, p=0.98) (Figure 4) nor continuous ∆cTnT values (adjusted HR 0.77, 95% CI: 0.33-1.75, p=0.53) was associated with all-cause mortality after retrograde CTO PCI.
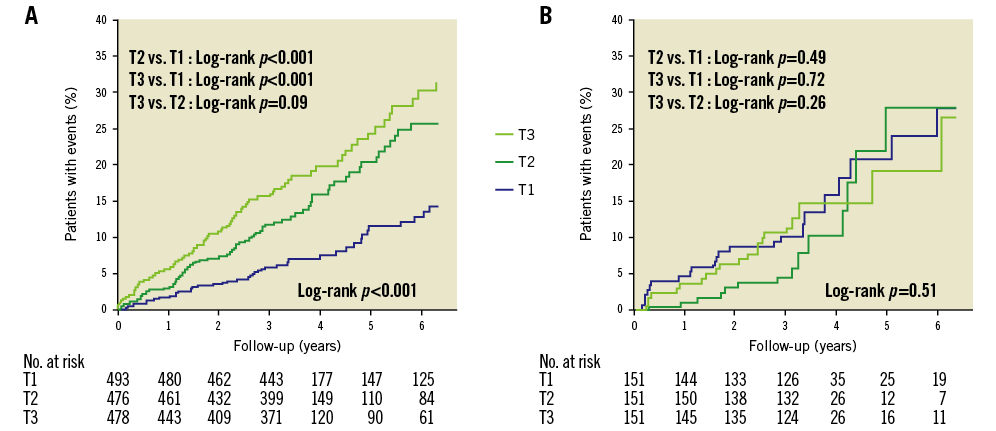
Figure 5. Kaplan-Meier estimates for all-cause mortality in patients after antegrade and retrograde percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) stratified according to tertiles of cardiac troponin T increases (∆cTnT). A) Antegrade patient cohort. B) Retrograde patient cohort. Patients were divided into tertiles (T1, T2, T3) based on the difference between peak cardiac troponin T values within 24 hours and the baseline values (∆cTnT).
Procedural success was linked with survival benefit in the antegrade group (HR 0.54, 95% CI: 0.41-0.72, p<0.001; adjusted HR 0.71, 95% CI: 0.53-0.94, p=0.02), and tended to reduce mortality in the retrograde group (HR 0.42, 95% CI: 0.22-0.81, p=0.009; adjusted HR 0.52, 95% CI: 0.27-1.02, p=0.057). Procedural success was associated with reduced all-cause mortality in patients without PMI (n=1,425; HR 0.52, 95% CI: 0.38-0.70, p<0.001; adjusted HR 0.67, 95% CI: 0.50-0.91, p=0.01), but not in those with PMI (n=484; HR 0.52, 95% CI: 0.31-0.86, p=0.01; adjusted HR 0.69, 95% CI: 0.41-1.16, p=0.16).
Discussion
This study shows that the impact of PMI on outcomes after CTO PCI differs significantly according to the crossing technique. Although PMI was observed more frequently after retrograde CTO recanalisation, we could not detect a significant association with survival. On the contrary, with the antegrade approach, the occurrence of PMI and troponin elevations were strongly associated with all-cause mortality during a median follow-up of 3.1 years. After antegrade CTO recanalisation, the risk of death increased in a stepwise fashion with a higher troponin release, with a 50% increased risk in the third as compared to the first biomarker tertile. These findings suggest a differential clinical relevance of periprocedural cardiac biomarker elevations in antegrade and retrograde procedures.
MYOCARDIAL DAMAGE FOLLOWING ANTEGRADE AND RETROGRADE CTO PCI
Retrograde procedures were increasingly performed during the course of the registry. Periprocedural myocardial injury following PCI is mostly caused by side branch occlusion or distal embolisation19,20. In this patient cohort, troponin elevations signifying periprocedural myocardial damage were 2.3-fold higher following retrograde as compared to antegrade crossing techniques. The higher amount of PMI observed after retrograde procedures is consistent with previously reported data6,8-10. The increased risk of myocardial damage mostly attributed to the retrograde approach may be due to the more calcified lesions and an overall increased procedural complexity encountered in these patients8,21. In addition, the increased periprocedural ischaemic burden in retrograde interventions has previously been related to the obstruction of major collateral channels causing myocardial ischaemia of the collateral territory, particularly with septal dilatation or the use of microcatheters9,22.
MYOCARDIAL DAMAGE AND LONG-TERM MORTALITY FOLLOWING ANTEGRADE AND RETROGRADE CTO PCI
In this study, patients were dichotomised according to the presence or absence of PMI as defined by cTnT elevations according to the third universal definition of myocardial infarction and given the high myocardial tissue specificity and clinical sensitivity of this biomarker16. Further, patients were divided into tertiles of biomarker release, and continuous levels of troponin elevations were included in the multivariate models. This approach allowed assessment of the impact of different degrees of biomarker elevations on outcomes irrespective of arbitrarily defined threshold values23. As only patients with elective CTO recanalisation procedures were included in this registry, the cardiac biomarker increase is assumed to be solely related to the procedure itself and not overlaid by an acute coronary syndrome event as in other studies. Indeed, other registries investigating periprocedural myocardial injury in CTO PCI included up to one third of patients with acute coronary syndromes6,12. Similar to previously reported data in patients undergoing PCI4,5,24, the association between PMI and worse outcomes has been shown in CTO PCI irrespective of the crossing technique6. In our patient cohort, there was a proportional relationship between the extent of biomarker release and the risk of adverse outcomes after antegrade CTO recanalisation. Although the extent of periprocedural myocardial damage was higher after retrograde CTO PCI, this increase did not translate into worse clinical outcomes in this patient subset. This observation underlines the safety and efficacy of retrograde crossing strategies in selected patients. The association between the amount of myocardial damage after antegrade interventions and long-term mortality is of particular interest, and outlines the importance of minimising damage to the distal vessel territory in these patients.
We can only speculate about the pathophysiological mechanisms underlying the observation that PMI has a prognostic impact in antegrade, but not retrograde procedures. First, as elevated biomarker levels were not linked to adverse events in retrograde interventions, the high procedural success rates associated with a reduced size of the ischaemic area and a reduced severity of ischaemia seem to outweigh the increased periprocedural ischaemic burden observed in the retrograde cohort. Second, the distal vessel territory of the coronary artery may be particularly sensitive to side branch occlusion and distal embolisation when treated by the antegrade approach, as wire passage in these patients may cause more downstream dissection to the important vessel periphery. Side branch occlusion and distal embolisation may, however, be less relevant in retrograde procedures as mostly septal branches are affected, possibly leaving the distal vessel territory of the CTO coronary artery intact. Third, prolonged myocardial ischaemia due to obstruction of collateral channels and microcatheter/wire passage might enhance troponin release without causing structural damage, as has been described previously25. Accordingly, duration of fluoroscopy time was associated with an increased troponin release in patients undergoing retrograde but not antegrade CTO recanalisation. Fourth, collateral channels observed in patients selected for retrograde procedures may allow the myocardium to recover and maintain viability after the intervention26. However, pathophysiological mechanisms linking myocardial injury to adverse events need to be elucidated, and future clinical trials are needed to investigate the benefits of adjunct pharmacological treatments in the reduction of myocardial injury following CTO PCI.
As procedural success was independently associated with survival benefit in patients without PMI, but not in those with PMI, these findings suggest that procedural success translates into improved survival in selected subgroups of CTO patients only. Comparisons between groups may, however, be limited by the lower number of patients in the PMI group, and future studies are needed to address this issue fully.
Study limitations
This study comprising long-term follow-up of a large CTO PCI patient cohort has some limitations that need to be addressed. First, the study is limited by its retrospective, single-centre observational design. However, comprehensive clinical and procedural data were available, and baseline and post-procedural troponin levels systematically measured in all patients. Second, unmeasured variables not taken into account in the multivariate models may have affected the results, and differences in the degree of myocardial injury and mortality rates between groups may have had an influence. Third, biomarker analyses included both conventional and high-sensitivity troponin assays, and imaging evidence of new loss of viable myocardium or regional wall motion abnormalities was not available in this patient cohort. Further, the lower number of patients in the retrograde cohort reduces the statistical power for this subset.
Conclusions
This study reports the association between PMI and long-term mortality following antegrade, but not retrograde CTO recanalisation, and underlines the clinical relevance of only minor biomarker elevations in comparison to more unusual high-level increases. Future large-scale randomised trials are needed to confirm these results, and attempts to minimise myocardial damage after CTO PCI are to be encouraged, particularly when antegrade crossing strategies are applied.
| Impact on daily practice As the higher risk of periprocedural myocardial damage following retrograde procedures does not translate into worse clinical outcomes, these findings underline the safety of the retrograde approach in clinical practice. |
Conflict of interest statement
M. Ferenc reports receiving speaker honoraria from Abbott Vascular, Boston, Medtronic, and Biotronik. C. Gebhard has received grant support from the Novartis Foundation, the Swiss National Science Foundation, the Olga Mayenfisch Foundation, the OPO Foundation, and the Swiss Heart Foundation (all Switzerland). The other authors have no conflicts of interest to declare.