Abstract
Aims: Percutaneous coronary intervention for chronic total coronary occlusions (CTO) becomes increasingly more complex with the transcollateral retrograde approach. This study assesses the effect of the retrograde approach on markers of ischaemia and clinical events.
Methods and results: Four hundred and ninety-two consecutive procedures in 392 patients were prospectively evaluated. Before and within 18-24 hours after the PCI creatine kinase (CK) and cardiac troponin I (cTnI) were obtained. A CK increase of greater than three times the upper limit of normal (ULN) was considered a periprocedural MI. Patients with initially elevated cTnI were excluded. In 106 patients with a retrograde wire passage of the septal collaterals, the incidence of a CK or TnI increase was higher as compared to the antegrade group. Patients with septal dilatation or passage of a dilatation catheter (Corsair) showed the highest cTnI. There was no difference in cardiac death or cerebral complications between the groups with antegrade and retrograde approach within the first 30 days.
Conclusions: Complex retrograde recanalisation procedures for CTOs lead to an increased periprocedural ischaemic burden, most likely due to obstruction of the collateral pathway, and to the increased plaque burden of complex lesions treated with the retrograde approach.
Introduction
An increase of markers of myocardial ischaemias has been observed in five to 30% of percutaneous coronary interventions (PCI) after stent implantation for non-occlusive lesions1,2. The main cause of this increase is believed to be side branch occlusions and distal microembolisation. Confirmation of such embolic particles was obtained with high-intensity transient Doppler ultrasound signals during balloon and stent dilatation3.
The recently modified universal definition of myocardial infarction (MI) puts more weight on the more sensitive increase of troponin levels after PCI, thus increasing the detection of a periprocedural MI type 4a4. With a large plaque load in chronic total coronary occlusions (CTO) one may expect a higher incidence of troponin increase during PCI, but this was not observed in comparison to non-occlusive lesions5. A recent meta-analysis of 18,941 published CTO procedures reported a periprocedural MI rate of less than 3%6, but systematic monitoring of periprocedural ischaemic markers was not established in any of these reports.
As procedural strategies to treat complex CTOs are getting more complex with retrograde passage of collaterals7-9, this may cause prolonged ischaemia during PCI for CTOs. Furthermore, these new techniques enable the operator to be successful in even more complex lesions10. The extent of troponin increase during PCI for CTOs has not been mentioned or assessed, even in recent reports focusing on complication rates11,12. The present study therefore investigated prospectively the periprocedural increase of markers of cardiac injury comparing the new strategies of transcollateral retrograde approach with conventional antegrade techniques in a large, consecutive series of CTOs.
Methods
STUDY POPULATION
In a prospective analysis we assessed 392 consecutive patients (age 64.3±10.9 years; 329 men, 63 women) with a total of 492 CTO recanalisation procedures at our institution between March 2006 and September 2011. The procedures were performed by one operator with a high previous experience of >500 CTO procedures at the beginning of the study period. In 38 patients, two different CTOs were treated, in 49 patients a second attempt was made after an initial failure, and in six of these 49 a third procedure was carried out. Inclusion criteria were: 1) duration of the occlusion greater than three months, 2) TIMI 0 coronary flow, 3) evidence of ischaemia related to the occluded vessel, or viable myocardium in an akinetic segment assessed by magnetic resonance imaging.
The recanalisation was performed via the femoral approach using 6 Fr to 8 Fr guiding catheters. The interventional strategy was to use drug-eluting stents in all patients to cover the lesion with a stent/artery ratio of at least 1:113. Angiographic success was defined as a final angiographic residual stenosis of less than 20% by visual estimation and TIMI 3 flow.
All patients regularly took 100 mg aspirin per day. During the intervention, a bolus of 100 IU/kg intravenous heparin was given. Subsequent boluses of heparin were administered according to a check of activated clotting time every 30 minutes. Patients not already on dual antiplatelet therapy received clopidogrel 600 mg as loading dose on the morning of the intervention, and subsequently 75 mg per day for one year. All other medications were given at the discretion of the attending physician. Platelet glycoprotein IIb/IIIa receptor inhibitors were not used.
PROCEDURAL STRATEGY
The procedural strategy to open the CTO was generally an antegrade approach with the use of contralateral injections in 75% of cases, whenever ipsilateral collateral filling was not present. A recanalisation wire was always supported by a microcatheter. A gradual increase of wire stiffness was applied in case of failed wire advancement beyond the proximal occlusion cap. In case of a subintimal wire position, the first wire was left in place and a parallel wire approach was applied using a second, stiffer wire. If the initial antegrade strategy failed, the patient was rescheduled for a second attempt using the retrograde approach, if feasible collateral connections were identified. In referred patients with an already failed antegrade approach and no additional options of extended antegrade strategies such as parallel wiring, patients were primarily attempted via the retrograde approach. In 20% of procedures the retrograde procedure followed immediately after an initial antegrade attempt.
GROUP COMPARISON
Patients who underwent an antegrade recanalisation procedure were compared to patients who underwent a transcollateral complex recanalisation procedure. Within the latter group, we compared patients with a transseptal wire passage without any further catheter advancement through the collateral channel, including those in whom a wire passage was not successful, with those with either a dilatation of the septal collateral channel or advancement of a dilatation catheter (Corsair®; ASAHI Intecc, Aichi, Japan) available since 2009, which had replaced collateral channel dilatation.
All patients were prospectively followed regarding periprocedural complications (Q-wave MI, death or need for urgent revascularisation) during hospitalisation and within 30 days after discharge.
Cardiac biomarkers
Venous blood samples were taken before the procedure (baseline), and the second sample 16-24 hrs after conclusion of the PCI. Creatine kinase (CK), and cardiac troponin I (cTnI) were analysed in these samples. CK (upper limit of normal value [ULN] for women 170 U/L, for men 190 U/L) was enzymatically determined according to the supplier’s instructions using a cobas c 502 machine, the test kit provided by Roche Diagnostics (Mannheim, Germany). cTnI was measured as previously described in more detail5 by a two-site immunoenzymatic (sandwich) immunoassay (Dimension EXL 200; Siemens Healthcare Diagnostics Inc., Newark, DE, USA). The 99th percentile of the cTnI level in a reference population was at 0.07 ng/mL, and the threshold determined by the local clinical chemistry lab was 0.14 ng/ml.
Definition of procedure-related myocardial injury
The new universal criteria were applied to define the incidence of periprocedural MI4. cTnI is now considered as the defining marker of choice, with an increase of >5 times ULN to indicate post-procedural MI. We also categorised our patients according to a CK increase, as this is used frequently in routine practice to assess periprocedural MI, where CK-myocardial band (CK-MB) assessment is not in routine use.
Statistical analysis
Continuous numeric data are given as mean value±standard deviation when they were normally distributed; otherwise, median and interquartile ranges are shown. Categorical data are shown as percentages. In order to analyse differences between groups, we used the Mann-Whitney U test for steady numeric data and Fisher’s exact test for categorical data. A logistic regression analysis was carried out to assess determinants of cardiac biomarker elevation. A two-sided p-value <0.05 was considered to indicate a significant difference. All calculations were performed using the statistical software NCSS 2007 by Jerry L. Hintze.
Results
CLINICAL AND PROCEDURAL DATA
In this study population, the duration of CTOs was known in 248 patients and ranged from three to 336 months (mean 63 months, median 30 months). Table 1 shows the clinical characteristics of the antegrade and retrograde approach groups. There were younger patients, longer occlusion duration, and a double proportion of second attempts in the retrograde as compared to the antegrade group.
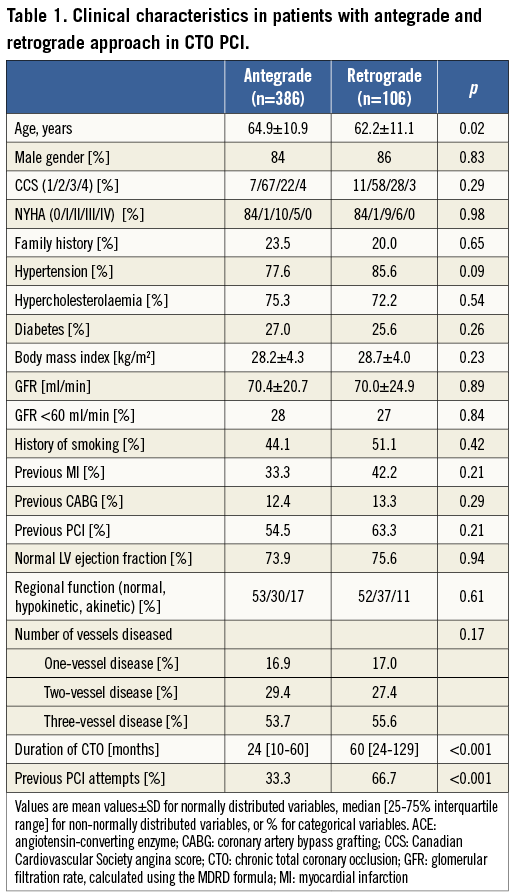
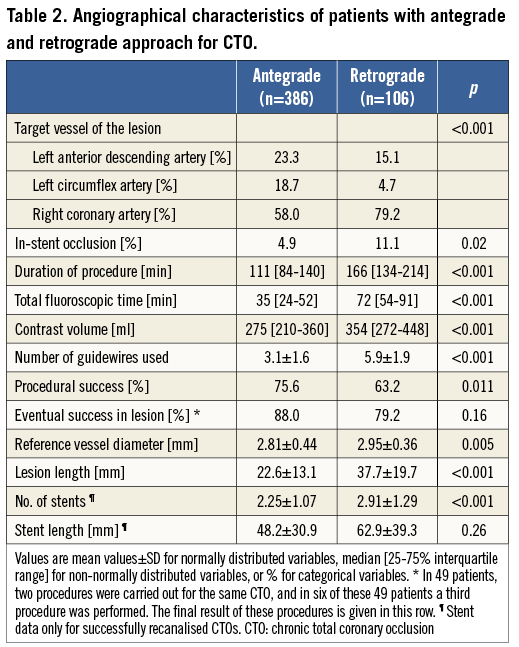
The right coronary artery as target was more frequent in the retrograde group. The duration of the procedure, as well as fluoroscopy time and contrast use, was significantly higher with the retrograde approach, and lesion length and stent number were higher with a trend for a longer overall stent length (Table 2). The overall per patient success rate including repeat attempts was 86% during this time period.
CARDIAC BIOMARKERS AFTER RECANALISATION PROCEDURES
The baseline level of cardiac markers was similar in both groups, but after 24 hours the CK and cTnI increase was significantly higher in patients who had undergone a retrograde procedure (Table 3). If we took the cut-off value for CK of >3 times ULN to identify a periprocedural MI, we observed a 4.7% incidence in the retrograde group as compared to only 0.8% in the antegrade group. A cTnI increase above the value of 0.14 ng/ml was frequently observed with the antegrade approach as well, but it was observed more often in patients with the retrograde approach. An increase above 0.7 ng/ml (five times ULN) was observed in 53.1% in the retrograde group, more than double the frequency in the antegrade group (Table 3).
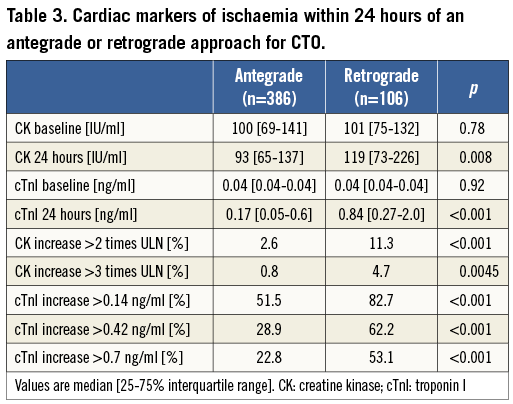
Of the 106 retrograde procedures, 91 were performed via the transseptal collateral route. Among these transseptal procedures, in 31 only a wire was passed through the collateral for the so-called marker or touching wire technique, whereas in 60 procedures a septal dilatation or the passage of a Corsair catheter was carried out. The septal dilation did not increase the incidence of significant CK increase after the procedure, but led to a significantly higher increase of cTnI levels (Figure 1). The procedures using septal dilation tended to last slightly longer than those without collateral dilation (Table 4).
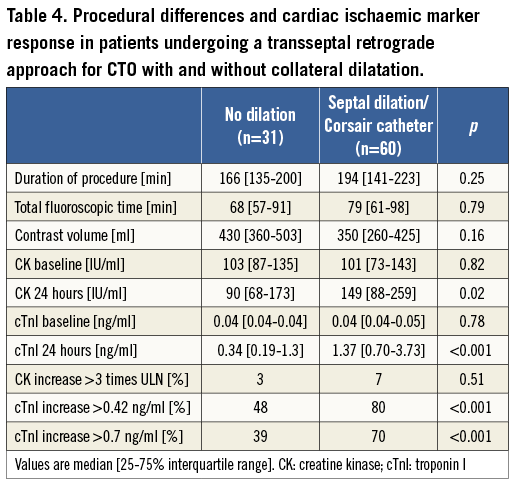
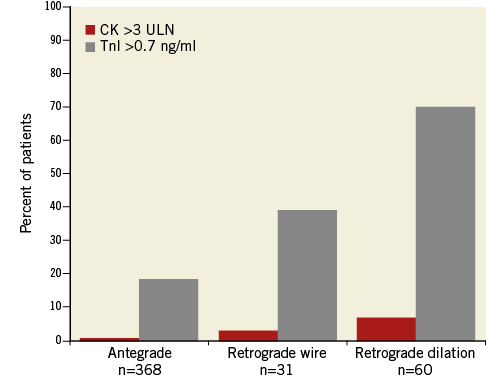
Figure 1. The relation of the applied technique and the incidence of periprocedural infarctions (without development of new Q-waves) defined as a CK increase >3 times ULN within 24 hours of the PCI of a CTO, and the incidence of periprocedural troponin increase above 0.7 ng/ml within 24 hours. Only retrograde procedures involving the transseptal pathway are shown.
In 15 patients with epicardial wire passage this included the passage of a microcatheter, in 10 cases the Corsair catheter. The incidence of cTnI increase beyond 0.42 ng/ml was 53%, and beyond 0.7 ng/ml it was still observed in 47%, which was in the range of the transseptal approach without dilatation. There was no incidence of a CK increase >3 times ULN in these transepicardial procedures.
During the procedure with retrograde passage of a catheter through the collateral pathway, 45 of 60 patients (75%) complained about a persistent chest discomfort of various degrees, and in five patients EKG changes of acute ischaemia were also observed. This was always followed by an increase of cTnI after the procedure.
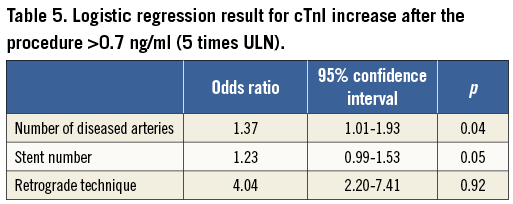
A logistic regression analysis with the independent variables of number of diseased coronary arteries, number of stents implanted, and the retrograde technique showed the latter as the major determinant to predict cTnI >0.7 (Table 5). There was also no significant correlation between stent length and cTnI or CK increase, the respective correlation coefficients being 0.20 and 0.09.
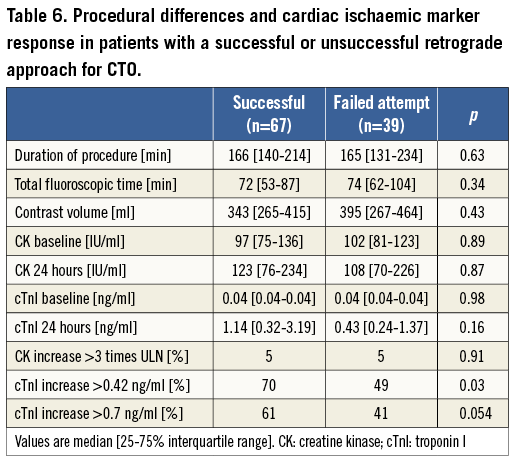
The comparison between successful and failed attempts showed more of an increase of cTnI after successful procedures (Table 6).
Clinical events
Clinical follow-up was available in all patients within 30 days after the procedure. There was no increased rate of post-procedural clinical events in the retrograde group. None of the patients experienced prolonged or recurrent angina during an overall 48 hours post-procedural hospitalisation period. There was one cardiac in-hospital death in a patient with failed retrograde transseptal approach (0.2% of all procedures). There was one major perforation requiring pericardiocentesis in the antegrade group (0.3%) and three in the retrograde group (2.3%), two of them related to damage of a collateral pathway. None of these four patients required further treatment after removal of the drainage within 48 hours. No new Q-wave infarction was detected in the post-procedural EKG taken on the day after the procedure. There was no relation between these low numbers of in-hospital and 30-day adverse events and the incidence of post-procedural increase of markers of myocardial injury.
Discussion
In this study we showed that the incidence of troponin increase after recanalisation of CTOs is a more frequent observation after complex retrograde procedures than after antegrade interventions. The obstruction of collateral channels with either small balloons or the Corsair channel dilator led in both cases to a significant increase of cardiac markers of periprocedural ischaemia. We had reported previously that CTO PCI did not lead to more cardiac marker increase than PCI of non-occluded arteries in a series from 1999-2004, when the retrograde technique had not been adopted5. The observed increase in CK and cTnI in the antegrade group of this study was in a similar range to our previous study. The main difference now was the increasing number of retrograde procedures enabling us to treat more complex CTOs.
There may be several mechanisms leading to periprocedural ischaemia, specifically in the retrograde approach. With the retrograde approach, an obstruction of major collateral channels by the retrograde wire and microcatheter system occurs during a long period of the procedure time. This causal relationship is also supported by the more pronounced increase of markers during procedures with septal dilatation as compared to septal wire passage alone. Another observation from our study was the higher incidence of cTnI increase in successful versus unsuccessful procedures, because the mode of failure was the inability to cross the collaterals, and therefore less ischaemia was caused in unsuccessful procedures.
When a Corsair catheter or a microcatheter is kept in position within the collaterals with a diameter of well below one mm, it will no longer contribute to the collateral supply. Despite parallel collateral channels, the acute obstruction of one of the major supplies to the collateralised territory is not fully compensated by other collaterals14,15.
An alternative mechanism of cardiac biomarker elevation could be the extent of atherosclerosis which is especially pronounced in chronically occluded coronary arteries16. The lesion characteristics were more complex in the retrograde group with longer lesions and longer stented segments, so this could have contributed to the marker increase. A higher incidence of microembolism can occur during the procedure due to more atherosclerotic burden, detectable as small spots of myocardial necrosis by magnetic resonance imaging17-19. We recently showed that high-intensity transient signals as indicators of embolic particles can be detected by intracoronary Doppler ultrasound and occur frequently during PCI, especially after stent implantation3. The higher number of stents used in the retrograde group led to more individual inflations, and thus more microembolisation as one of the contributing factors to the observed differences between the groups.
Another factor involved in the post-procedural increase of cardiac markers could be vessel complications such as side branch occlusions20. In antegrade CTO procedures, side branch occlusion appeared to be the major cause of periprocedural enzyme increase21. This may also serve as an additional explanation in the present study, as the predominant retrograde technique of reverse CART (controlled antegrade and retrograde tracking) involves an often extensive subintimal pathway from the distal true lumen position of the wire to the proximal re-entry, which is then covered by stents7. However, we have no information on the periprocedural incidence of cardiac marker increase from these previous studies from Japan, other than the report of periprocedural infarct rates below 3% based on the cut-off of a threefold increase of CK11. The number of reports on the retrograde experience is increasing steadily, but only a few assess periprocedural ischaemia, such as a small report from Spain with a moderate increase of troponin observed in all 11 patients22, whereas most reports did not assess CK, CK-MB or troponin systematically23-25.
Limitations
This study was a prospective analysis based on a single-centre experience with only one lead operator. This may be considered a limitation, but it also eliminates the variance between different operators in the technical approach to a CTO. The study period includes the time when the retrograde approach was being developed and adopted with iterations of the procedural steps. However, the analysis shows that there was no reduction of periprocedural troponin increase over time, but rather an increase with even more complex cases taken on with improved devices and techniques.
The timing of the blood sampling to detect periprocedural ischaemia was according to the normal setting of a daily hospital routine, which meant that the first blood sample was taken on the morning following the PCI, which is about 16-24 hours after the conclusion of the procedure. Thus, a transient increase of CK might have been missed, but the more sensitive troponin increase would not have been missed, as the increase is persistent over more than 24 hours. We did not assess CK-MB as the second standard of detecting specific myocardial injury, as this assessment is no longer implemented in daily routine in favour of the more sensitive troponin assays in German hospitals.
Clinical relevance
Periprocedural infarcts type 4a (according to the initial classification26) occur frequently after PCI; however, the clinical impact of this observation in PCI of stable angina pectoris is still under debate1,2. Using CK-MB, only a severe increase >5 times ULN seems to have a considerable impact on clinical outcome27. Using the more recent definition with cTnI as the discriminating marker4, the rate of type 4a infarctions is even as high as 70% in complex retrograde procedures. As an additional qualifying factor to define a periprocedural infarction, EKG signs of ischaemia are required, or angina, and evidence of side branch occlusions. Both EKG signs of ischaemia and angina occur frequently during the placement of a retrograde microcatheter within the collaterals, as well as side branch occlusions with the CART technique.
One may debate whether the new universal definitions of MI are discriminatory regarding possible late events in this specific interventional setting. At least within the first 30 days we did not find an increase in adverse events between the two groups. Nevertheless, this high frequency of enzyme leaks should be recognised for future clinical trials, which may then also enable obtaining a long-term follow-up and prognostic assessment.
There is growing evidence of the clinical benefit of CTO revascularisation28, and therefore the observed increase of periprocedural ischaemic markers should not be a reason to withhold a potentially beneficial intervention. However, in certain haemodynamic and anatomical situations, where the donor artery also is obstructed, the additional and continuous ischaemia during the retrograde approach may lead to a severe haemodynamic compromise, even without the obvious complication of a donor artery injury or thrombosis.
| Impact on daily practice Percutaneous coronary intervention for chronic total coronary occlusions (CTO) becomes increasingly more complex with the retrograde transcollateral approach. The increasing complexity of the procedure leads to an increased periprocedural ischaemic burden, most likely due to obstruction of the collateral pathway, and increased plaque burden of complex lesions treated with the retrograde approach. In certain haemodynamic and anatomical situations, where the donor artery is also obstructed, the additional and continuous ischaemia during the retrograde approach may lead to a severe haemodynamic compromise even without the obvious complication of a donor artery injury or thrombosis. |
Conflict of interest statement
The authors have no conflicts of interest to declare.