Abstract
Aims: This cross-sectional observational study was designed to evaluate the uptake and outcome of patient education after percutaneous coronary intervention (PCI).
Methods and results: A questionnaire containing 41 items was handed out to consecutive patients from randomly selected Swedish hospitals after PCI. Questions concerned the patient’s attribution of the cause of the cardiac event, perception of the information provided by physicians and nurses, and a self-assessment of changes in lifestyle post PCI regarding tobacco, physical activity, food habits and stress. Replies were obtained from 1,073 patients (reply rate 67%). Non-modifiable risk factors (age, heredity) were attributed a higher rate as the cause of disease compared to modifiable factors (smoking, physical activity, food habits). Most patients (67%) perceived they were cured, and 38% perceived from the given information that there was no need to change their habits. A mere 27% reported that they still had cardiovascular disease and needed behavioural change. After PCI, 16% continued to use tobacco; half of these were offered smoking cessation support. In spite of an 80% referral rate to cardiac rehabilitation, one out of two patients did not enrol. Fewer than half were regularly physically active. Nutritional counselling was provided to 71%, but only 40% changed food habits. Stress management programmes were rarely provided.
Conclusions: Current preventive practice scarcely meets the challenge posed by the progress in modern invasive cardiology. The Study of Patient Information after percutaneous Coronary Intervention (SPICI) motivates an in-depth revision and adaptation of cardiac rehabilitation programmes in order to improve patient understanding of the disease, and to support greater compliance with a cardioprotective lifestyle.
Introduction
It is well established that cardiovascular diseases (CVD) are strongly influenced by behavioural factors, especially the use of tobacco, an unhealthy diet, physical inactivity and psychosocial stress. According to a statement from The World Health Organization (WHO), over three-quarters of all CVD mortality could be prevented with adequate changes in lifestyle1. However, in the recently published “European Cardiovascular Disease Statistics 2012”2, it was reported that the rate of decline in smoking is now slow and rates remain stable or are increasing in some countries, particularly among women. Few adults in European countries participate in adequate levels of physical activity, with inactivity more common among women than men. The levels of obesity are high across Europe in both adults and children. The prevalence of diabetes in Europe is high and has increased rapidly over the last ten years, increasing by more than 50% in many countries2. Does this influence the behaviour of CVD patients and their willingness to adopt necessary lifestyle changes?
In recent decades, cardiac rehabilitation and prevention programmes have been recommended for patients with coronary artery disease (CAD)3. These programmes reduce cardiac mortality and improve quality of life4, and there are several specific guidelines available5,6. Cardiac rehabilitation has proven to be beneficial for female and for elderly patients7,8. However, in many countries only a minority of CAD patients are referred to programmes aimed at supporting behavioural change such as smoking cessation, increasing physical activity and adopting healthy food habits. The Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART) national registry9, providing comprehensive data on acute and long-term care of patients with acute myocardial infarction (AMI), reveals that uptake of cardiac rehabilitation is about 40%, even though the potential benefits of this intervention among patients after acute percutaneous coronary intervention (PCI) on top of cardioprotective medication have been convincingly demonstrated in the OASIS 5 study10.
The design of these programmes often dates back several decades, tailor-made for an acute care which has changed substantially over time: the introduction of PCI, shorter duration of hospital stay, and more effective medication have all contributed to a considerably less dramatic experience and to improved short to medium-term prognosis for the patients.
However, the long-term consequences with a very high readmission rate during the first five years after acute coronary syndromes, as demonstrated in the GRACE registry11, continue to impose a strain on patients and healthcare systems.
One may question whether conventional cardiac rehabilitation still meets the needs of the present-day CAD patient, since many clinicians find it hard to motivate patients to participate. Furthermore, in a recent Cochrane review there was no evidence that education/information, which is an essential component of cardiac rehabilitation, reduced cardiac mortality or morbidity, revascularisation or hospitalisation12. Therefore, the aim of our Study of Patient Information after Coronary Intervention (SPICI) was to investigate in a representative post-PCI population:
– The patients’ attribution of the cause of their acute cardiac event.
– The patients’ perception and understanding of the information provided by physicians and nurses.
– The content of the post-PCI cardiac prevention and rehabilitation programme to which patients were invited and the patients’ willingness to be enrolled.
– The patients’ self-assessed change in lifestyle post PCI with regard to smoking, physical activity, food habits and stress.
Methods
In Sweden 18,000 patients undergo PCI annually, 70-80% due to an acute coronary event. In collaboration with the Swedish Heart and Lung Patients Association (HLR), a questionnaire was sent to 29 randomly selected hospitals, stratified to include centres with and without acute PCI service. The SPICI questionnaire was compiled by the authors of the study together with two HLR members who acted as “patient research partners” in order to incorporate the patients’ perspective in all 41 questions, as these persons had personal experience of cardiac care.
As there was to our knowledge no earlier validated questionnaire for Swedish patients post PCI with the specific items that were needed, the questionnaire had to be created de novo. Special care was given to designing a model that could be used by other investigators. Initially, the three cardiologists in the team prepared a first set of questions which were then reviewed and adapted by the two psychologists of the SPICI group who had extensive experience in the field of patient questionnaires. After two revisions, the patient research partners from HLR contributed further valuable comments, after which a third version was tested among a group of patients who had recently undergone an acute PCI. After final minor changes, the questionnaire was approved by all for use in the study. An English version can be obtained free of charge on demand from the lead author of this paper.
The questionnaire covered the following items: patients’ beliefs regarding what caused their coronary artery disease, information given to the patient at discharge and at the first follow-up visit to the out-patients clinic, information on the need for lifestyle modification, invitation to and participation in a physical training programme, level of physical activity (number of times a week the patient engaged in physical activity of low, intermediate or high intensity), availability of a smoking cessation programme at the centre and tobacco habits (number of cigarettes or packages of moist snuff per day, if any), availability of nutritional counselling and food habits (food frequency questionnaire regarding intake of vegetables, fruit/berries, fish and unhealthy snacks) after PCI, and availability of a stress management programme.
For the definitions of target values for physical activity and food habits the recommendations of the 4th Joint Taskforce on CVD Prevention in Clinical Practice were used3.
The questionnaire was handed out by a cardiac nurse to 30-70 consecutive patients at each centre, depending on the size of the centre, six to 10 weeks after the PCI at the time when patients are normally invited to join a comprehensive cardiac rehabilitation programme. The replies were sent directly and strictly anonymously to the Heart and Lung Patients Association, in order to limit any influence of caring staff on the answers. In total, 1,800 questionnaires, which represents 10% of the annual Swedish PCI population, were sent to the participating hospitals.
We have analysed the entire material and subgroups by gender and by three age groups: <60 years, 60-74 years and ≥75 years. The rationale for gender analysis was that, based on earlier observations, women have tended to be referred to cardiac rehabilitation programmes less frequently. The reason for a subgroup analysis by age was the lack of data on the increasing group of elderly patients after PCI as compared to younger patients.
The content of the material and the design of the SPICI study were approved by the regional ethics committee of Linköping University. All statistics are descriptive.
Results
Out of the 1,800 questionnaires, 1,598 were handed out by nurses consecutively within the time frame of the study. At the HLR headquarters, 1,073 valid replies were received, resulting in a reply rate of 67%: 290 females (26%), 783 males (74%), mean age 66 (34-89 years). The majority of patients were in the age group 60-74 years: 511 persons (55%: 26% female, 74% male). The age group <60 years contained 246 persons (27%: 22% female, 78% male) and the age group ≥75 years 166 persons (18%: 34% female, 66% male). Correct age data were missing for 150 patients. Most patients (83%) had undergone PCI due to an acute coronary syndrome. Replies were received within eight weeks after PCI from four out of five patients. After PCI, 28% still had chest pain complaints and in one in ten patients this resulted in limitations in their activities of daily living.
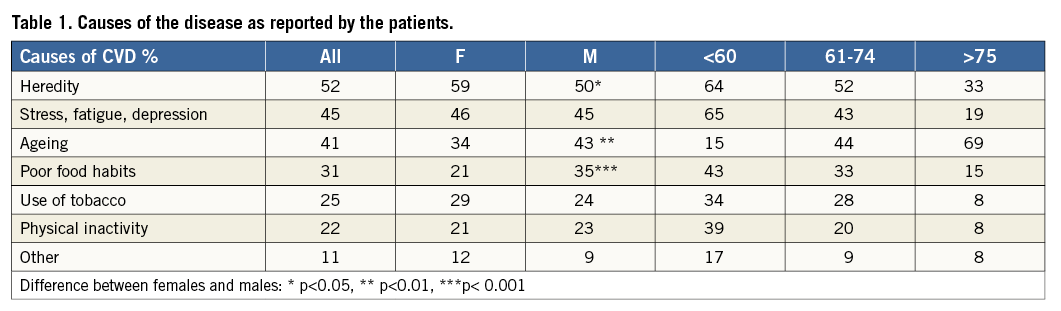
When asked what might have caused their cardiac condition patients chose non-modifiable risk factors (heredity and age) more frequently than the modifiable factors smoking, a lack of physical activity and inappropriate food habits (Table 1). Among the younger patients (<60) stress, fatigue and depression rated high as a possible cause. In this age group the modifiable risk factors were ranked higher than in the other age groups, although heredity was still seen as the main cause.
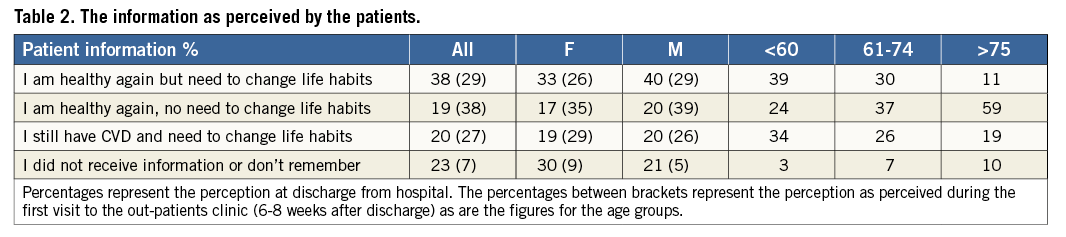
Many patients perceived the core message from the given information to be that they had been cured from their CAD through the PCI procedure (Table 2). Barely one in five patients believed that they still had a cardiovascular disorder and that they should consider lifestyle modification (one in three patients in the younger age group). Patient information at discharge from hospital was mainly given without the presence of a family member or friend (71%), and this improved only slightly at the first follow-up visit (63% informed alone). When comparing patients who were informed with an accompanying person as opposed to alone there was no significant difference in the perception of the provided patient education. Even though 65% expressed satisfaction with the information from the hospital staff, 54% sought further information from relatives and friends. In the younger age group 56% tried to find additional knowledge through the internet, as compared to 38% in the 60-74 years age group and 14% among the elderly patients.
Before PCI, the use of tobacco (mainly cigarette smoking) was three times more common than in the general Swedish population (39%). After PCI, this diminished to 16%, still above the national level. Among males <75 years, one in five patients continued to use tobacco. The majority of smokers failed to be referred to a smoking cessation programme according to the replies received (Table 3). When comparing patients who believed that they had been cured with those who understood that CAD is a chronic illness, there was a tendency to greater tobacco cessation in the latter group (61 vs. 49%, p=0.05).
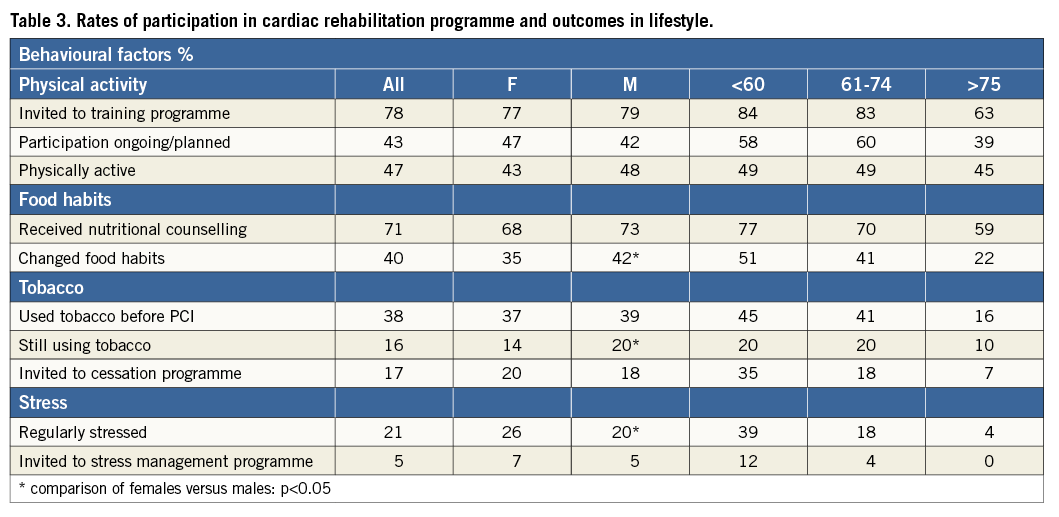
In Sweden, all hospitals offer physical training programmes for groups of CAD patients. This is reflected in the outcome of the questionnaire: only one in six was not invited to join and there were no gender differences. The majority did actually participate: 58% among patients up to 60 years of age, 60% among patients in the age group 60-74 years, respectively, and 39% among the elderly. Most of these had already joined the training sessions at the time of replying to the questionnaire. However, when asked for their present daily physical activity, fewer than 50% attained the recommended levels of the guidelines (Table 3). There were no differences in attaining these levels among groups with differing perceptions of the patient education, i.e., between those believing that CAD is a chronic illness and those believing they were cured after PCI.
Three-quarters of the patients received nutritional counselling, commonly through an educational meeting with a dietician. After that, 40% decided to change and improve food habits, 50% among the younger patients, and 22% among the elderly (Table 3). Almost half (45%) did not consume fruit and vegetables daily as recommended in the prevention guidelines. There was a highly significant difference (53 vs. 25%, p<0.001) in adopting healthier food habits among those who were recommended to change diet as compared to those who perceived that no behavioural changes were needed.
Finally, stress was reported by the patients as one of the main causes of CAD with 39% of the younger patients complaining of being regularly stressed. Stress management programmes are not widely used in Swedish hospitals and a mere 12% of the younger patients with stress complaints were referred to this type of qualified support.
Discussion
This study in a large and representative national sample reveals a number of shortcomings in the present practice of cardiac rehabilitation in a country which previously had a good track record as compared to other European countries13. There appears to be a remarkable lack of knowledge as to the role of modifiable risk factors in this post-PCI population, even more pronounced than the previous findings in a smaller study from Australia14. Smoking, lack of physical activity and food habits were regarded as important causes of the disease by 20-30% of the patients, in contrast to the fact that 39% were tobacco users at the time of the PCI and, even after the procedure and educational efforts, 45-50% of patients were still not attaining targets for healthy food habits and physical activity. However, the exact pre-PCI risk profiles of the patients were not known, but in the Swedish general PCI population smoking rates vary between 20 and 27% and the prevalence of those who are overweight (BMI >27) reaches up to 48%9.
Furthermore, a minority of the patients seem to have perceived that CAD is a chronic disease that cannot be cured by a coronary intervention alone. Clearly there is a significant overconfidence in the curative role of PCI, as was also reported recently by Lee et al15, but it should be noticed that our study reflects the understanding of the individual patient and not necessarily the precise content of the given information from doctors and nurses. In a review by Young et al containing 10 smaller studies, a misalignment was found between the patients’ and health professionals’ perception of the information16. This is even more pronounced when the views from patients and cardiologists are compared17. Patient information does not extend to the nearest relatives, who could have been of significant support to the patient in changing towards a more heart-healthy lifestyle. However, this study did not show that this actually affected the misconceptions.
Globally, concerning post-PCI cardiac prevention and rehabilitation, the majority of the population was invited to physical training and attended dietary counselling. However, the outcome of these efforts was less satisfactory, since only half reached the target levels for physical activity and food habits. This is in line with the findings of the OASIS 5 study10. Obviously there is considerable room for improvement.
The findings for smoking and stress management are problematic. Since one in five were still using tobacco (mainly smoking), it is hardly acceptable that according to the patients only a minority received smoking cessation support. These patients had a doubled risk for new cardiac events as compared to those who stopped smoking18. A similar argument is valid for stress management, especially in the younger age groups. Here guidelines give a clear recommendation as to the need for professional support, something which appears to be lacking in many centres.
One explanation for the waning interest in participation in prevention and rehabilitation programmes and for changing behaviour might be the fact that patients attribute their disease to factors they cannot influence, such as age and family history of CAD. Apparently, modifiable risk factors are not seen as the patients’ own road to prevention. This may be reinforced by the next misconception, the conviction that PCI cures the underlying disease and that behavioural change is not really needed or even strongly recommended by healthcare workers. Furthermore, the timing of patient information after a short stay in hospital might not be the most effective as patients may still be in a state of mental shock and confusion after the acute event.
Our study showed that patient information does not extend to the majority of the closest relatives, who could have been of significant support to the patient in changing towards a more heart-healthy lifestyle. The importance of including spouses and significant others has been demonstrated in the review by Gentz et al19. Here, examples as in the EUROACTION study based upon nurse-coordinated prevention services or from the GOSPEL study could lead the way to a more effective programme20.
The Health Belief Model, developed in the context of behavioural science and aimed at explaining individuals’ preparedness to change health behaviour, could shed light on the results and provide some clinical implications. Key concepts of the model are Perceived (by the patient) susceptibility, Perceived severity, Perceived benefits, Perceived barriers, Cues to action, and Self-efficacy. For behavioural change to occur, it is necessary that the patient understands and accepts that CAD is a severe disease to which he or she is particularly vulnerable, perceives that personal health benefits are possible through behavioural change, that the barriers can be overcome by his or her own efforts, that there is a “trigger” to start acting, and that the patient feels assured of his or her own competence. Effective health education could help the patient to increase the urgency of personal lifestyle change. Obviously, the mode of information/advice most commonly used by professionals does not achieve that, and thus new ways need to be explored.
Study limitations
It should be pointed out that the results of the study are entirely based upon confidentially submitted replies from the patients and thus only reflect their views, which might not necessarily be the view of healthcare workers.
However, what is of importance for the occurrence of a change of behaviour is the patients’ perception and understanding.
With a reply rate of almost 70%, which is a common level for this type of study, it is not thought that the outcome among the 30% of non-respondents would be more positive, especially regarding the modifiable risk factors.
Conclusions
| Impact on daily practice Adopting a heart-healthy lifestyle is an important priority for patients after an acute coronary syndrome and PCI. To achieve this, clear patient education and support from the medical staff are of major importance. This study has shown that there is ample room for improvement in providing patient information, where even participation of family members should be strongly encouraged. Only then can the unsatisfactory compliance to lifestyle modification be reversed, thus improving the outcome for the post-PCI patient. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

