Abstract
Aims: The aim of the study was to evaluate the incidence and causes of rehospitalisation within one year after percutaneous coronary intervention (PCI) in a country where the National Health Service provides universal tax-supported healthcare, guaranteeing residents free hospital access.
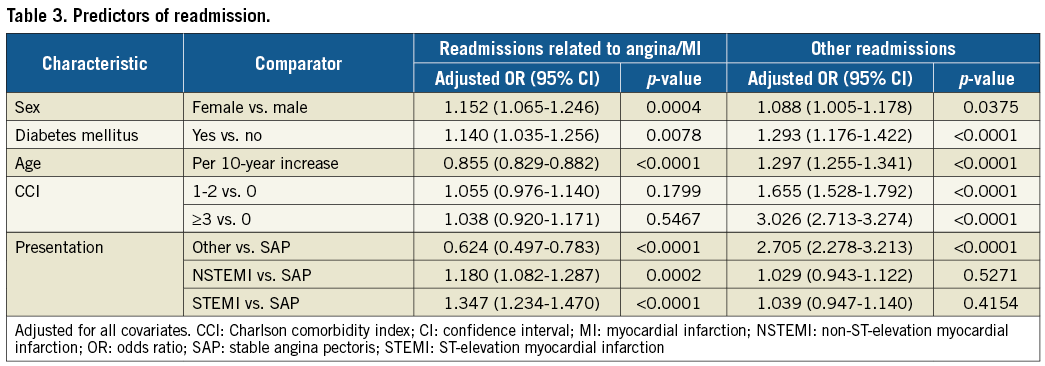
Methods and results: Between January 2010 and September 2014, 17,111 patients were treated with PCI in two University Hospitals in Western Denmark. Patients who were readmitted within one year after PCI were identified. The overall one-year readmission rate was 50.4%. The cause was angina/myocardial infarction (MI) in 4,282 patients (49.7%), and other reasons in 4,334 (50.3%). Predictors of angina/MI-related readmissions were female gender (odds ratio [OR] 1.15, 95% confidence interval [CI]: 1.07-1.25), diabetes (OR 1.14, 95% CI: 1.04-1.26), age (per 10-year increase) (OR 0.86, 95% CI: 0.83-0.88), and indication for index PCI (stable angina pectoris as reference): ST-segment elevation myocardial infarction (OR 1.34, 95% CI: 1.23-1.47) and non-ST-segment elevation myocardial infarction (OR 1.18, 95% CI: 1.08-1.29). Predictors for other readmissions were female gender (OR 1.09, 95% CI: 1.01-1.18), diabetes (OR 1.29, 95% CI: 1.18-1.42), age (OR 1.30, 95% CI: 1.26-1.34) and Charlson comorbidity index ≥3 (OR 3.03, 95% CI: 2.71-3.27).
Conclusions: In an unselected patient cohort treated with PCI, half of the patients were rehospitalised within one year, highlighting the impact of comorbidity in patients with ischaemic heart disease.
Abbreviations
ACS: acute coronary syndrome
CABG: coronary artery bypass graft
CCI: Charlson comorbidity index
CHF: chronic heart failure
CI: confidence interval
IHD: ischaemic heart disease
MI: myocardial infarction
NSTEMI: non-ST-segment elevation myocardial infarction
OR: odds ratio
PCI: percutaneous coronary intervention
SAP: stable angina pectoris
STEMI: ST-segment elevation myocardial infarction
WDHR: Western Denmark Heart Registry
Introduction
Ischaemic heart disease (IHD) is a progressive condition which can lead to an increased risk of mortality and morbidity1. It is a common and burdening condition for both the patients and the healthcare system2,3. Initially, patients with coronary artery disease have a relatively low mortality rate (1.2-2.4%), but the individual prognosis is highly influenced by various factors, such as baseline characteristics, previous myocardial infarction (MI), and comorbid diseases such as diabetes and chronic kidney disease4.
Half of the patients presenting with IHD and acute coronary syndrome (ACS) suffer from chronic comorbidities, which may have a major influence on a patient’s outcome both during and after hospitalisation1,5. It is important to bear in mind various factors such as age, comorbidities and physical condition, when reperfusion with thrombolysis or revascularisation with percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) is considered4,5. PCI is a common and low-risk procedure with a poorly described readmission pattern6.
Thirty-day readmission rates after PCI range from 8.0% to 17.9% with a majority of cardiac-related reasons for rehospitalisation, but long-term readmission rates and non-cardiac reasons are poorly described6-10. It is difficult to predict long-term readmission, as knowledge of this health issue is limited, but individual health condition has a great influence on the risk of readmission, and needs to be considered when discussing this issue7,11,12. It is important to understand the reasons for readmission to improve patient outcome and prevent readmissions. To shed light on the impact of comorbidity in a progressive condition such as IHD, a long-term investigation of risk factors is necessary.
The purpose of this study was to investigate the one-year readmission rate after PCI and to evaluate predictors for angina/MI-related and other rehospitalisations in a country with free access to healthcare.
Methods
STUDY POPULATION
The study was conducted using Western Denmark’s healthcare databases, which cover the region’s entire population of approximately 3.0 million inhabitants (55% of the Danish population). A detailed description of the databases has been reported previously13. The Danish National Health Service provides universal tax-supported healthcare, guaranteeing residents free access to general practitioners and hospitals. We used the Western Denmark Heart Registry (WDHR) to identify all PCI procedures performed from 1 January 2010 up to 30 September 2014, at Odense University Hospital and Aarhus University Hospital. The study protocol was approved by The Danish Data Protection Agency (2012-41-0164).
All Danish citizens can be tracked in the healthcare system and national registries. The Danish Civil Registration System has kept electronic records on gender, birth date, residence, and emigration date since 1968, and characteristics of all non-psychiatric in-patient admissions since 1977 with daily updates14. The 10-digit civil registration number assigned at birth and used in all registries allows accurate record linkage15. The Danish Civil Registration System provided vital status data for our study participants and minimised loss to follow-up.
DATA ANALYSIS
PCI procedures were linked to the Danish Civil Registration System using the 10-digit civil registration number, which made it possible to list the readmissions within one year, and to track the diagnoses given during the readmission, specified using ICD-10 coding. Several diagnoses were given during the hospitalisation, but only one action diagnosis was given at discharge. The action diagnosis was used as the reason for readmission. Admissions within two days of the index procedure were interpreted as transfer between departments and were not included as readmissions in the data set. Patients who were readmitted several times within one year were only included once in the data set with the first given diagnosis. Only hospital readmissions were included.
For each patient, data on all diagnoses from the Danish National Registry of Patients were obtained. Comorbidity scores were computed using the Charlson comorbidity index (CCI)16, which covers 19 major disease categories, including diabetes mellitus, heart failure, cerebrovascular diseases, and cancer. The CCI is used to estimate risk of death in patients with comorbid diseases. The CCI value is a weighted summary of the diagnoses and weights the number and seriousness of comorbid diseases calculated on the basis of one-year mortality associated with each disease in the original Charlson data set16. A modified CCI was used, as diabetes mellitus was considered a separate confounder and removed from the CCI. Reasons for readmission were recorded and categorised.
STATISTICAL ANALYSIS
Contingency tables were created for the main study variables characterising patients readmitted to hospital and not readmitted after PCI. The group of readmitted patients was further divided into patients with and without diagnoses of IHD. The follow-up period was 365 days after PCI. Statistical comparisons were undertaken for the two readmitted patient groups versus the non-readmitted group, using t-tests for continuous variables and the χ² test for categorical variables. For readmitted patients, the most frequently occurring diagnosis was identified during readmission and up to one year after PCI. Kaplan-Meier curves were constructed to estimate the probability of readmission within 365 days from the PCI and compared across indications for PCI (stable angina pectoris [SAP], STEMI, NSTEMI and other), comorbidities (using CCI ten years prior to PCI), diabetes mellitus and gender with log-rank tests. Eventually, potential risk factors for readmission after PCI were analysed using logistic regression: the indication for PCI, comorbidities, diabetes mellitus together with age and gender. All data analyses were carried out using SAS software, version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
STUDY POPULATION
A total of 18,025 patients were treated with PCI at one of the two participating PCI centres between January 2010 and September 2014. Of these, 158 patients were foreign citizens, 14 patients emigrated, 566 patients died before hospital discharge and 176 had missing admission dates in the database; these were all excluded from the analysis (Figure 1). Thus, the final study cohort consisted of 17,111 patients. The readmissions included both acute readmissions and staged revascularisation. Of the included patients, 8,616 patients (50.4%) were readmitted to the hospital within 365 days after the index PCI procedure. The all-cause 30-day readmission rate was 14.9%. The majority of patients were readmitted within the first month (Figure 2).
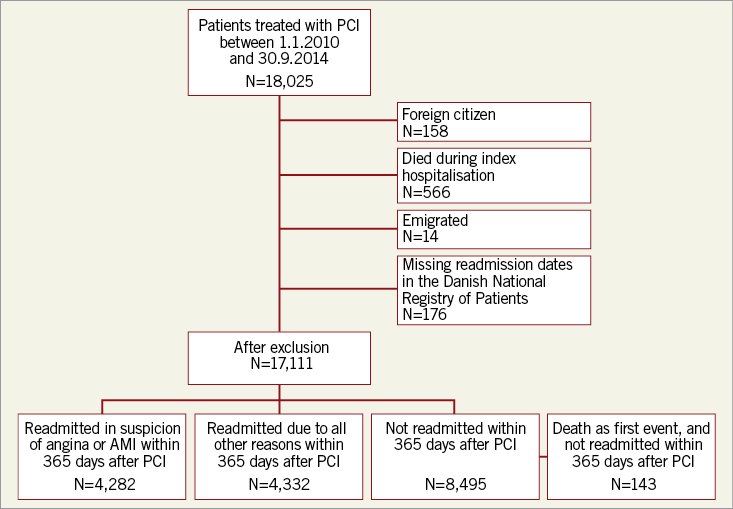
Figure 1. Flow chart of enrolled patients.
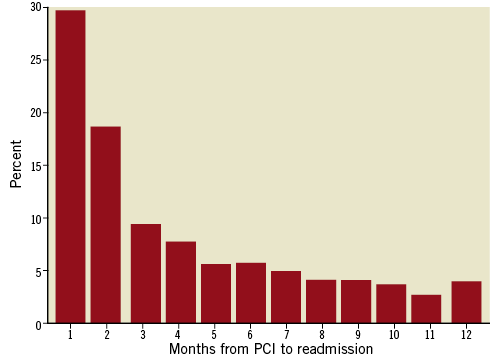
Figure 2. Timing of all-cause rehospitalisation: non-cumulative frequency within one year.
CHARACTERISTICS OF READMITTED PATIENTS
The clinical characteristics at baseline are shown in Table 1. Compared with patients who were not readmitted, females, smokers and diabetics were more likely to be readmitted for angina/MI. However, patients readmitted due to other reasons were more likely to be elderly, female, have a family history of IHD, hypertension, hypercholesterolaemia, diabetes mellitus, and have higher levels of creatinine, compared to patients who were not readmitted. Patients with previous PCI, or CABG, or MI patients with comorbidities, with a longer stay at index hospitalisation, and patients with multivessel disease were more likely to be readmitted within 365 days, no matter the reason. The frequency of each component of the modified CCI is illustrated in Figure 3. The most common comorbidities were MI, peripheral vascular disease and cerebrovascular disease.
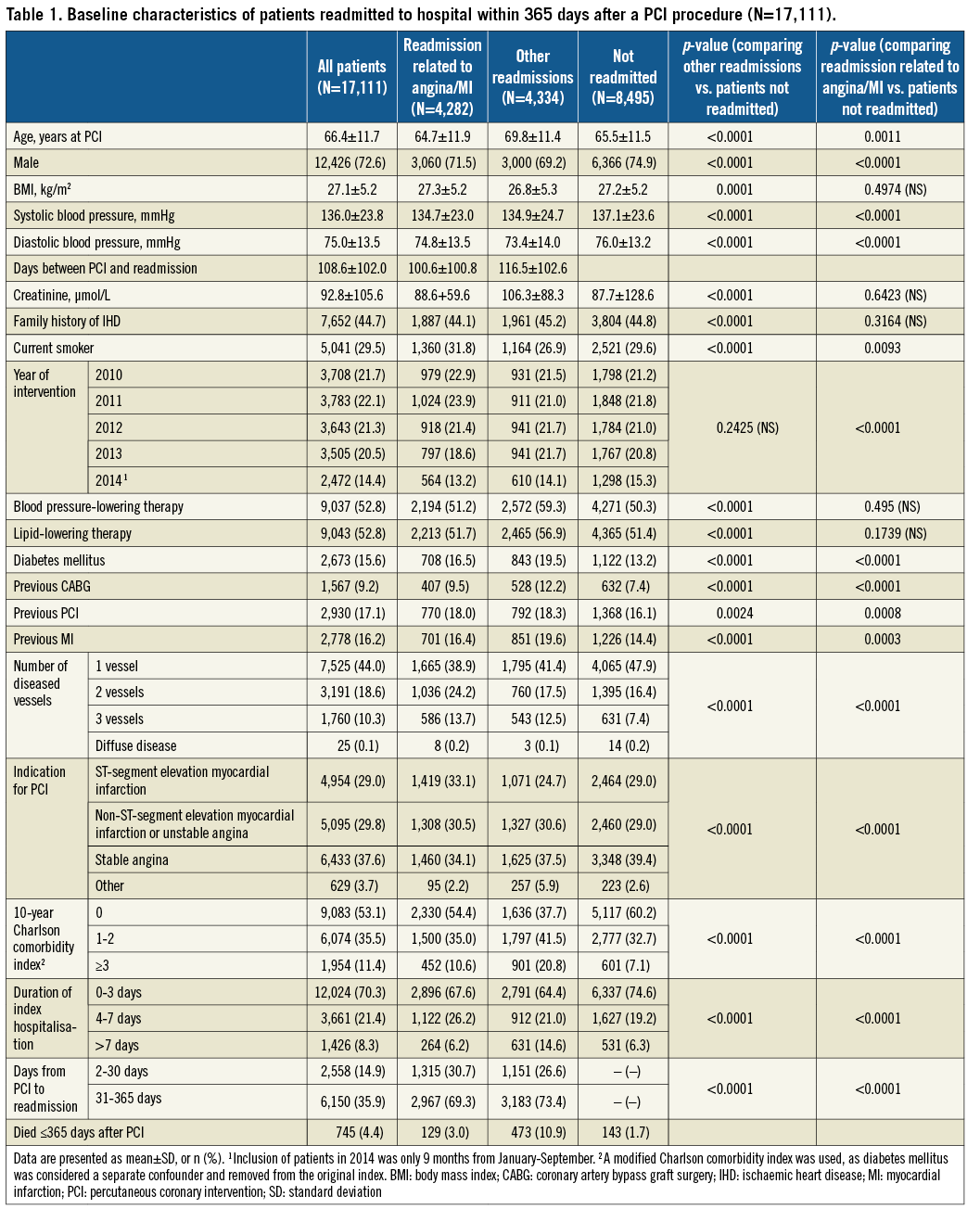
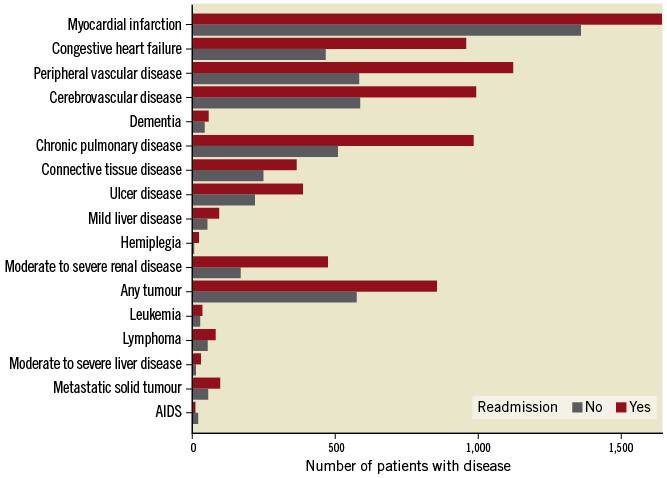
Figure 3. Frequency of each component of the modified Charlson comorbidity index. Note that diabetes is considered a separate confounder and is excluded from the index.
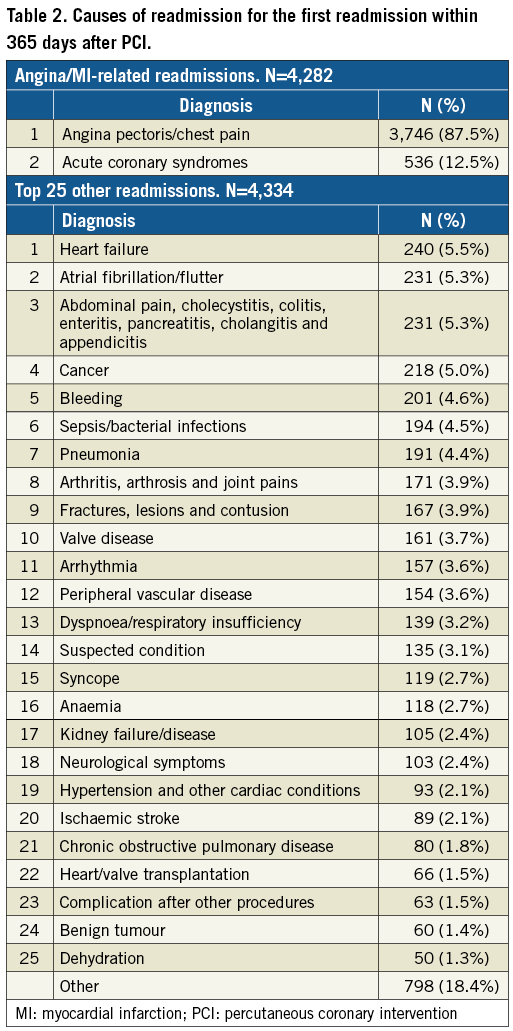
REASONS FOR READMISSION
Reasons for readmission were various and are shown in Table 2. Of all the 8,616 patients readmitted, 4,282 patients (49.7%) were readmitted on suspicion of angina/MI within 365 days after the index PCI procedure. The diagnoses defining angina/MI are shown in Table 2. The remaining 4,334 patients (50.3%) were readmitted due to other indications. The most common angina/MI-related reasons for readmission were angina pectoris/chest pain (87.5%) and ACS (12.5%). ACS is defined by the action diagnosis: MI, unspecified, unstable angina, STEMI and NSTEMI. For patients readmitted for other reasons, heart failure was the most common cause (5.5%), followed by atrial fibrillation/flutter (5.3%), and abdominal pain (5.3%) (Table 2).
RISK OF READMISSION
The probability of readmission is illustrated in the Kaplan-Meier curves (Figure 4). The probability of being readmitted within 365 days increased with higher modified 10-year CCI, if the patients were diabetic or female, or if the PCI was performed due to an indication other than NSTEMI, STEMI or SAP.
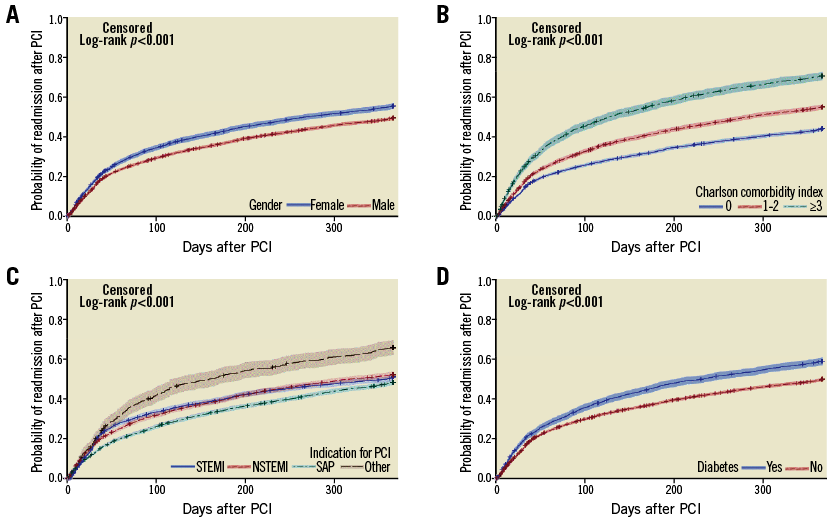
Figure 4. Kaplan-Meier cumulative event curves with 95% confidence limits for probability of readmission after PCI within a year as per various factors. A) Gender. B) Modified Charlson comorbidity index. C) Indication for percutaneous coronary intervention. D) Diabetes status.
A modified 10-year CCI ≥3 was the strongest risk factor for other readmission (OR 3.0, 95% CI: 2.7-3.3, p<0.0001) (Table 3) but did not increase the risk for angina/MI patients. Patients presenting with NSTEMI and STEMI were at no greater risk of being readmitted for other reasons compared to patients with SAP, whereas patients with other indications for PCI had a 2.7-fold increased risk for other readmissions than those with stable angina. However, both NSTEMI and STEMI patients had a higher risk of angina/MI-related readmission compared to SAP, while other indications for PCI were associated with a lower likelihood of angina/MI-related readmission. Older age was linked to a 1.3 times higher risk of other readmission but was associated with a lower likelihood of angina/MI-related readmission. Females and diabetic patients had a slightly higher risk of readmission in both groups.
ANGIOGRAM AND REVASCULARISATION
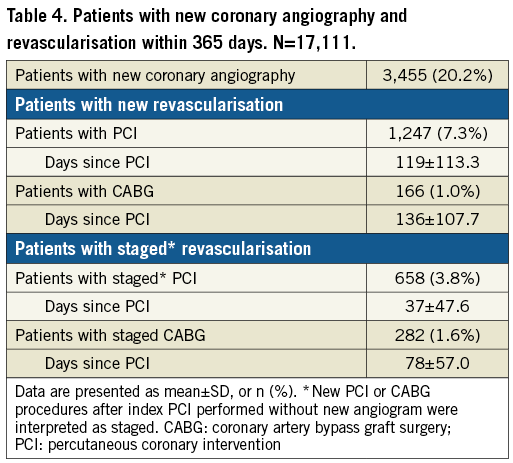
Of the 17,111 patients included in the study, 3,455 (20.2%) had new coronary angiography within 365 days after index PCI (Table 4). The coronary angiography was followed by PCI in 1,247 patients (7.3%), and CABG in 166 patients (1.0%). Planned revascularisation was seen in 5.5% of the patients – 658 (3.8%) received staged PCI, and 282 (1.6%) underwent staged CABG.
Discussion
The present study found that half of the patients undergoing PCI were readmitted within one year after the procedure. Half of the readmitted patients were rehospitalised on suspicion of angina/MI, and half were readmitted due to other causes. One in eight of the angina/MI patients was hospitalised due to ACS, and the rest were readmitted due to angina or angina-suspected events. The all-cause 30-day readmission rate was found to be 14.9%.
A recent published study8 found a lower 30-day readmission rate compared to ours (9.8% vs. 14.9%). Multiple aspects can influence the differing results. Firstly, data collection using WDHR combined with the Danish Civil Registration System made it possible to register all readmissions to every Danish hospital and not just the index hospital, thereby minimising loss to follow-up. Secondly, we included PCI centres with patient uptake from Western Denmark, which comprises both metropolitan and rural areas. Additionally, our study included patients from two of five PCI centres, thereby representing half of the Danish population. Furthermore, the patient’s possibility of readmission did not depend on health insurance or income due to the free Danish healthcare system, thus resulting in a diverse population.
Our results confirmed that chest pain was the major reason for readmission within the first year after index PCI. Among patients presenting with IHD symptoms, the suspicion of ACS often results in diagnostic procedures such as coronary angiography. Occasionally, angiography was performed for diagnostic or research purposes during readmission, and repeat revascularisations were also performed as elective procedures at times. One fifth of the readmitted patients had a new angiogram, but only a minority required revascularisation treatment with repeat PCI (7.3%) or CABG (1.0%). In prior studies, approximately half of all readmitted patients underwent a repeat PCI within 30 days of readmission, but only a small percentage (10.5%) was due to acute MI6,17-19. Also, in these studies, both staged and acute PCI were encountered. It should be borne in mind that patients are at great risk of repeat revascularisation within the first month after index PCI – often a staged procedure – but this plays a small role in readmission treatment within 365 days20.
In order to reduce the readmission rates after PCI, it should be taken into account that the patient’s individual condition and health status appear to influence the outcome, more than the PCI procedure itself. IHD is a progressive disease that leads to an increased risk of both mortality and morbidity. Several variables influencing mortality - such as female sex, medical insurance, education and age - are not modifiable7,17,19, but comorbidity may have a greater impact on one-year outcome than was previously expected. Our findings show that half of the patients were readmitted due to other reasons, e.g., infection, cancer, chronic obstructive pulmonary disease, diseased peripheral vessels, chronic heart failure (CHF) and kidney failure. Patients with a CCI ≥3 had a threefold increased risk of readmission for other reasons, whereas CCI played no significant role for patients readmitted with angina/MI. Furthermore, diabetes and old age increased the readmission risk significantly. Patients with an index indication for PCI other than SAP, STEMI or NSTEMI were at a 2.7-fold increased risk of readmission. This indication covers, for example, revascularisation in patients with arrhythmia, valve disease, cardiomyopathy and CHF with severely reduced ejection fraction. This group of patients is known to suffer from more comorbidities21. Comorbidity in IHD patients is associated with long-term mortality and renal disease, diabetes, peripheral vascular disease and chronic obstructive pulmonary disease in particular lead to higher mortality rates. These findings indicate that chronic medical conditions should be considered when investigating management of individual therapy, counselling and quality comparison to avoid readmission.
Long length of hospital stay was related to higher readmission rates for all readmissions, demonstrating that patients in need of no or limited healthcare after the procedure were less likely to be readmitted. Similar results have been presented in prior studies8,18. These findings indicate that patients with comorbidities are at high risk for readmission and are particularly vulnerable after PCI procedures. This information can be used to advise the health system to be careful with treatment and discharge of patients with comorbid diseases, and to consider the benefits from close outpatient follow-up after the index PCI.
Limitations
Our study should be interpreted in the context of several potential limitations. Firstly, as previously discussed, we did not distinguish between patients who were readmitted more than once within a year; these patients were only included in the data set with their first readmission diagnosis. In addition, readmission within two days of the index procedure was interpreted as transfer between departments or hospitals during the index admission and was not included as a readmission in the data set, thereby risking losing very early, acute readmissions. Secondly, it was not possible to differentiate between patients who underwent coronary angiography for research purposes, or patients undergoing coronary angiography or PCI due to acute chest pain. Thirdly, principal diagnoses such as “chest pain”, “chronic heart failure” and “ACS” are defined from several different diagnostic codes, which results in difficulties determining the actual reason for readmission. Finally, in our study, we present data from a population with free healthcare which are thereby not limited by economic aspects. It is unclear therefore to what extent our results can be generalised to other healthcare systems and hospitals.
Conclusions
In an unselected patient cohort treated with PCI, a substantial proportion of patients is readmitted within one year. The reasons for readmission fall into several broad categories with “chest pain” as the most common diagnosis. Even though one in five patients had new angiography, only a minority of the patients needed repeat revascularisation. Other reasons for rehospitalisations accounted for half of the readmissions with a large number of both cardiac and non-cardiac causes. Comorbidities were the strongest predictor of readmission and were associated with an increased risk of readmission, which highlights the impact of comorbidity in patients with IHD.
| Impact on daily practice In a country with free hospital access, half of the patients undergoing PCI were readmitted within one year after the procedure. Half of the readmitted patients were rehospitalised on suspicion of IHD, and half were readmitted due to non-IHD causes. This information can be used to advise the health system to be careful with treatment and discharge of patients with comorbid diseases, and to consider the benefits of close outpatient follow-up after index PCI. |
Conflict of interest statement
L.O. Jensen has received research grants from Terumo, Biotronik, St. Jude Medical, and Biosensors to her institution. The other authors have no conflicts of interest to declare.