Abstract
Aims: Patients with diabetes mellitus have poorer outcome following acute coronary syndromes and coronary revascularisation. Knowledge of long-term outcome after revascularisation in real-life situations is though limited was analysed.
Methods and results: Patients included in the Swedish Coronary Angiography Angioplasty Registry (SCAAR) in 2002-2007 with no previous revascularisation were followed for mortality after a first PCI until the end of 2007 (mean follow-up time 1,059 days). Differences in background and procedural characteristics were adjusted for in a multivariable Cox regression model. Of 57,708 patients, 18.8% had diabetes. Absolute mortality rate after four years follow-up was after STEMI, non-ST-elevation ACS and stable CAD respectively 23.2%, 17.8% and 12.7% for persons with diabetes and 14.4%, 8.4% and 5.7% for persons without diabetes. Adjusted relative risk for long-term mortality after first PCI was higher in patients with diabetes compared with those without; RR (95% CI); 1.66 (1.33-1.72), and after all three different PCI indications; RR (95% CI) for CAD; 2.01 (1.69-2.40), non-ST-elevation ACS 1.73 (1.58-1.90) and STEMI 1.44(1.30-1.59).
Conclusions: Long-term mortality is higher in diabetic patients compared with those without, after a first PCI and this mortality gap increases with follow-up time. Intensive secondary preventive measures are needed to improve this situation.
Introduction
Patients with diabetes mellitus run an increased risk of coronary heart disease and have an increased mortality and event rate after myocardial infarction1-2. Disturbances in glucose and lipid control, a tendency towards thrombosis and widespread diffuse coronary atherosclerosis are some explanations. Registry analysis indicates that the poorer outcome could be explained in part by lower use of evidence-based treatment in acute situations, including less use of revascularisation within 14 days after admission for acute coronary syndromes1,3. Patients with diabetes also run an increased risk of peri- and post-procedural complications during and after coronary revascularisation.
Coronary revascularisation is considered to be of major importance in diabetic patients with coronary artery disease. For instance, subgroup analysis revealed a substantial decrease in the one-year event rate using an early invasive strategy in diabetic NSTEMI patients2,4, but, despite the impressive event reduction, the event rate is still very high. Long-term follow-up data from the FRISC 2 trial showed an event rate for mortality or re-infarction of 42.5% in patients with diabetes receiving conservative treatment compared with 35.4% for those with an early invasive strategy after five years of follow-up4.
Based primarily on the results of the BARI trial, a strategy of coronary bypass surgery (CABG) aiming for complete revascularisation is recommended for patients with diabetes and three-vessel disease5-6. However, with the introduction of novel techniques and medication such as bare metal stents (BMS), drug-eluting stents (DES) and new antiplatelet therapies, combined with more widespread, easily available angiography laboratories, there has been a change in daily practise in favour of more PCI and less CABG. Despite this change in habits, our actual knowledge of long-term mortality after PCI in a modern setting in diabetic patients is sparse. The Swedish Coronary Angiography and Angioplasty Registry (SCAAR) offers a unique opportunity to analyse outcome and chosen treatment in unselected patients undergoing PCI in an everyday situation in Sweden. We analysed long-term mortality after a first PCI in patients with no previous revascularisation.
Material and methods
Patients
PRESENT MATERIAL
All PCI-treated patients in Sweden in 2002-2007 with no previous revascularisations and with complete information about background, treatment and events were included in the study. All calculations were based on the individual patient’s first PCI during the study period. Survival was followed until the end of 2007.
The SCAAR registry (http://www.ucr.uu.se/scaar/index.htm) collects data on all consecutive patients undergoing coronary angiography and PCI at the 29 centres that perform coronary angiography and PCI in Sweden. Registry data have been monitored and verified at all hospitals since 2001 by comparing 50 entered variables in 20 randomly selected interventions per hospital and year with the patients’ hospital records. The overall correspondence in data during that study period was 95.2%. The registry is sponsored by the Swedish health authorities and is independent of commercial funding.
FOLLOW-UP
The long-term follow-up was obtained by merging the SCAAR database with the Swedish National Population Registry and the Swedish registry of hospital diagnosis on the basis of the unique 10-digit personal identification number of each Swedish citizen.
DEFINITION OF DIABETES
Patients were defined as having diabetes mellitus if they had previously been hospitalised for a diabetes diagnosis or were receiving treatment with diet or antidiabetic oral drugs or insulin.
Statistical analysis
Diabetic and non-diabetic patients were compared regarding background characteristics, treatment and outcome. Long-term mortality was adjusted for differences in background and procedural characteristics in a multivariable Cox regression model (age, indication, gender, hospital, previous myocardial infarction, previous heart failure, previous renal insufficiency, previous stroke, previous peripheral artery disease, hypertension, smoking, complete revascularisation, angiography findings, stent/balloon or DES, numbers of stents, admission year, aspirin and clopidogrel before PCI, glyco-protein 2B/3A (GP2B/3A) blocker during PCI). All known variables with possible clinical importance recorded in SCAAR were forced into the statistical model. Independent predictors of mortality in the diabetic cohort were adjusted for the same factors as above in a Cox regression model. In the diabetic cohort, statistical interaction between indications for the procedure and GP2B/3A blocker treatment was also tested by introducing the interaction term indication GP2B/3A blocker treatment in the same statistical model.
All analyses were conducted using the SPSS statistical program (version 15.0; SPSS Inc., Chicago, IL, USA).
Ethical consideration
All patients were informed of their participation in the SCAAR registry. The merging of the registries was performed by the Epidemiologic Center of the Swedish National Board of Health and Welfare and was approved by the local ethics committee at Uppsala University.
Results
Between 2002-2007, 62,247 patients with no previous revascularisation were PCI treated in Sweden; 4,539 (7.3%) were excluded from the present study due to incomplete data. In the remaining 57,708 (92.7%) patients, the mean follow-up time (± Standard deviation) was 1,059 (± 569) days with a minimum time of 133 days and at a maximum time of 2,323 days and a median follow up of 1,012 days. Diabetes mellitus was present in 18.8% of the patients. Survival among patients included in the study did not differ compared with those excluded due to incomplete data (RR [95%CI]; 1.05 [0.97-1.15]).
Patients with diabetes were older and more frequently female (Table 1).
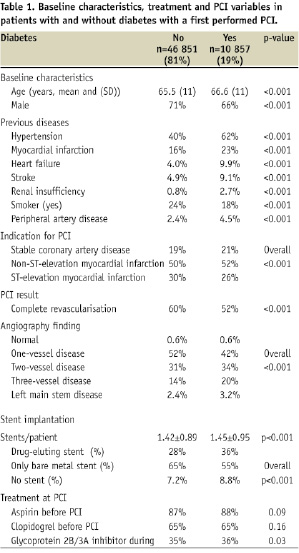
They had a more frequent history of hypertension, myocardial infarction, heart failure, stroke, renal insufficiency and peripheral artery disease but smoked less. There was no difference in treatment with aspirin or clopidogrel before the PCI. The indication for PCI in patients with diabetes was somewhat less frequently ST-elevation myocardial infarction (STEMI) and more frequently non-ST-elevation acute coronary syndrome (ACS) and stable coronary artery disease (CAD) compared with those without diabetes. Patients with diabetes had more advanced coronary artery disease with more frequent two- and three-vessel disease and more frequent involvement of the left main stem. Stents, including use of drug-eluting stents (DES), were more frequently used in diabetic patients. The rate of any procedure-related complications was similar in patients with and without diabetes respectively (6.8% vs. 7.2% p<0.01).
Mortality
Long-term survival curves for the whole cohort are shown in Figure 1 A-B (A: crude, B: adjusted). Both crude and adjusted relative risks for mortality were higher in patients with diabetes than in patients without diabetes, RR (95% CI); 1.99 (1.88-2.11) and 1.66 (1.33-1.72) respectively.
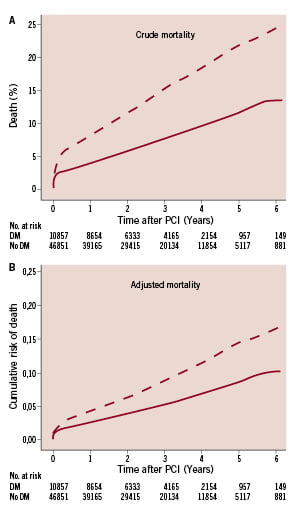
Figure 1. Long-term mortality after first PCI in patients with (broken line) and without (solid line) diabetes in the whole cohort A; unadjusted, B; adjusted cumulative mortality.
Even after considering different indications for PCI, outcome was poorer in diabetic patients with higher adjusted relative risk for mortality after stable CAD; RR (95% CI); 2.01 (1.69-2.40), non-ST-elevation ACS 1.73 (1.58-1.90), and STEMI 1.44 (1.30-1.59). The increased risk for patients with diabetes was even more pronounced at younger ages, with an adjusted relative risk for ages below < 65 years of (RR; CI 95%) 2.12 (1.84-2.43), between 65-74 years 1.61(1.44-1.81) and above > 74 years 1.51(1.38-1.65).
Long-term survival curves separate over time to the disadvantage of patients with diabetes, regardless of indication but especially among those with stable CAD. Crude and adjusted long-term mortality among diabetic patients with stable CAD was almost of the same magnitude as among non-diabetic patients with STEMI and worse than for non-diabetic patients with non-ST-elevation ACS (Figure 2 A-C, Figure 3).
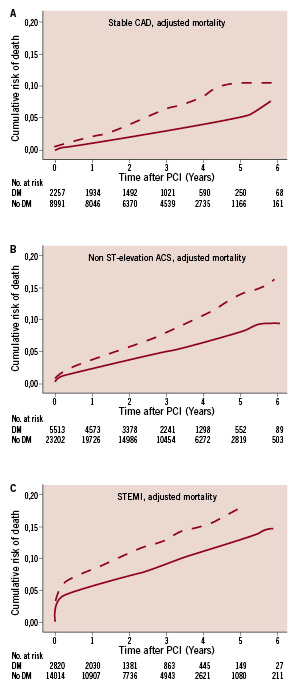
Figure 2. Adjusted long-term mortality in patients with (broken line) and without (solid line) diabetes after A; stable coronary artery disease, B; non-ST-elevation acute coronary syndrome, C; ST-elevation myocardial infarction.
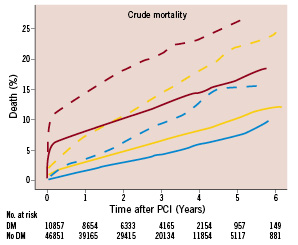
Figure 3. Crude cumulative long-term mortality after first PCI in patients with (broken lines) and without diabetes (solid line) after STEMI (red line), non-ST-elevation ACS (yellow line) and CAD (blue line).
The absolute mortality rate (Figure 3) after STEMI, non-ST-elevation ACS and CAD respectively was 14.6%, 8.2% and 3.3% for persons with diabetes after one year and 23.2%, 17.8% and 12.7% after 4 years’ follow-up. The corresponding figures for persons without diabetes were 7.2%, 2.8% and 1.3% after one year and 14.4%, 8.4% and 5.7% after 4 years’ follow-up.
Information on diabetes treatment was available from 2005. In this subgroup of 33,951 patients, 2,471 were classified as insulin-treated diabetes and 2,388 as non-insulin-treated diabetes. The relative risk increase for long-term mortality in comparison to non-diabetic patients was RR (95%CI); 2.70 (1.78-2.90) and 1.73 (1.50-2.01) respectively for insulin-treated and non-insulin-treated diabetes patients and 2.03(1.81-2.28) and 1.45(1.28-1.64) respectively after multiple adjustments.
Predictors for mortality among persons with diabetes
In a multivariate Cox regression analysis within the diabetic cohort (Table 2), independent predictors of mortality were high age, smoking, history of previous myocardial infarction, renal insufficiency, heart failure and peripheral artery disease. Male gender was associated with lower mortality in the crude model, but, after adjustments, the mortality in both genders was almost identical. The severity of the angiography findings and the acuteness (acute vs. stable situation) of the coronary disease were also related to mortality. In the model, diabetic patients with complete revascularisation had lower adjusted mortality than those with incomplete revascularisation (Table 2). In the unadjusted models, pre-treatment with aspirin and clopidogrel was associated with lower mortality, but, after adjustments, the effects decreased for aspirin but remained for clopidogrel.
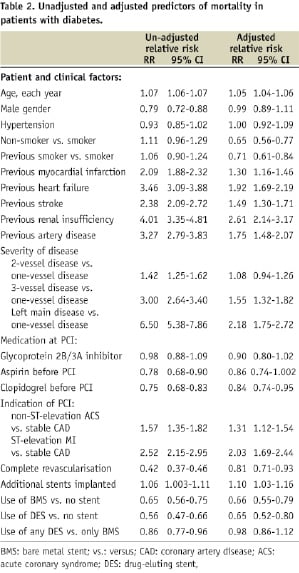
Stent use was associated with lower mortality, for both BMS and DES, compared with patients without stents. The crude mortality was lower in patients with at least one DES compared with patients with only BMS, but this difference disappeared when adjustments were made.
There was only a trend towards lower adjusted mortality in diabetic patients on GP 2B/3A blocker treatment compared with those who did not receive this treatment, but there was a statistically significant interaction between indications for PCI and GP2B/3A blocker treatment, p=0.034. When predictors of mortality were tested using the same statistical model in patients with diabetes and STEMI (n=2820), the adjusted mortality was lower in patients treated with GP2B/3A blockers than in those without (RR [95% CI]; 0.81 [0.67-0.98]). In diabetic patients without STEMI (n=8037), there was no adjusted association between GP2B/3A blocker treatment and mortality, RR (95% CI); 0.99 (0.84-1.15).
Discussion
In the present register-based analysis, the main finding is the higher long-term mortality after a first PCI in patients with diabetes compared with those without diabetes, regardless of indication and even after extensive adjustments for other risk factors. Furthermore, this risk increases with time, successively increasing the mortality gap between patients with and without diabetes. After four years of follow-up, 18% of the patients with diabetes had died compared with 9% of non-diabetic patients. Our results therefore strongly support the need for more intensive secondary handling and treatment after PCI in patients with diabetes, at least to decrease the successively increasing mortality gap. Results from registry-based analyses after myocardial infarction in patients with diabetes indicate that mortality can improve but not disappear with increased adherence to treatment guidelines1. Thus, increased adherence to guidelines will probably not be enough to eliminate the mortality difference and new strategies and research are needed.
We did in fact select a fairly healthy diabetic cohort without any previously performed revascularisation (PCI and/or CABG), but the prognosis is still much more dismal in the diabetic cohort. Interestingly, and contrary to what many would have predicted, diabetes emerged as an even stronger risk factor among those treated with PCI for the indication stable CAD than for STEMI and unstable CAD. Accordingly, long-term mortality among diabetic patients with stable angina was of almost the same magnitude as for non-diabetic patients with STEMI and poorer than for non-diabetic, unstable CAD patients. Moreover, and in accordance with results from MI populations, diabetes as a risk factor was even stronger in the younger age group below the age of 65 years1. Our results therefore indicate that a relatively young person with diabetes and stable CAD in need of PCI runs a much higher risk at long-term than might be expected.
Unfortunately, no information on type 1 or type 2 diabetes was available, but, in the subgroup of patients registered from 2005, which included information on insulin- or non-insulin-treated diabetes, we found that long-term mortality was highest among those treated with insulin but also higher in diabetic subjects without insulin treatment in comparison to non-diabetic subjects. Since there is no information on diabetes duration, HbA1c or type 1 or type 2 diabetes, it is not possible to draw any conclusions about whether this increased mortality among insulin-treated patients is related to a more severe diabetes state or to the type of diabetes treatment. This could be better clarified by a more careful characterisation of diabetes variables in future trials and registries.
It has been debated whether GP2B/3A blockers improve long-term prognosis in patients with diabetes mellitus treated with PCI. Both the ISAR-SWEET and ISAR-REACT 2 trials showed no significant impact by abciximab on the one-year combined outcome in patients with diabetes presenting with stable CAD or NSTEM undergoing PCI7-9. This could of course be related to low power among the diabetic subgroup (25% had diabetes in ISAR-REACT 2), but increased levels of inflammatory markers in the diabetic subgroup have been another speculative explanation. In the present analysis, in the entire diabetic cohort, treatment with GP2B/3A blockers was only associated with better long-term survival in those with ongoing STEMI, while no benefit from GP2B/3A blockers could be identified in the remainder.
Recent meta-analyses of randomised studies comparing drug-eluting stents with BMS showed no significant effect of DESs versus BMSs on total survival10. Our results show that the use of stents rather than the type of stent is the important factor and stent implantation was associated with better long-term survival irrespective of the type of stent. However it is important to keep in mind that the non-stented group also includes patients with an unsuccessful PCI result where no stent could be placed in the vessel, this group have probably a different prognosis.
Data concerning the influence of complete revascularisation on the long-term outcome in diabetic patients undergoing PCI are limited. In the present analysis, diabetic persons had better survival if they were judged to have complete revascularisation after the PCI procedure. This is in accordance with the results of a study by Nikolsky and colleagues which showed that complete percutaneous coronary revascularisation is associated with improved long-term outcome in diabetic patients with multivessel CAD11 and might be of special importance in patients with diabetes who often have more than one diseased vessel and complete revascularisation might therefore increase the chance of surviving a next coronary event. However, as “complete revascularisation” in our registry data probably reflects the extent and seriousness of the coronary artery disease and the result of the PCI rather than the intent of the operator to achieve complete revascularisation, the possibility that the improved prognosis related to complete revascularisation is mainly due to less severe coronary artery disease in this group cannot be ruled out. Diabetic patients with three-vessel disease had a poorer outcome than those with 1- or 2-vessel disease. Interestingly, after adjusting for other risk factors, outcome did not differ between those with 1- or 2-vessel disease, which indicates that, especially in those with 3-vessel disease, the best way to achieve complete revascularisation needs to be clarified.
One important limitation of the present analysis is the lack of comparison of long-term outcome after CABG. A randomised trial of CABG vs. PCI in diabetic patients in a modern setting is needed to increase our knowledge of who to send for PCI and who for CABG. The FREEDOM trial is an ongoing trial that will compare CABG and PCI with DES in persons with diabetes and multivessel disease12. In subgroup analyses of patients with diabetes and multivessel disease (n = 208), the 5-year follow-up data from the ARTS trial showed a non-significantly higher morality rate among those randomised to PCI vs. CABG (13.5% vs. 8.3%, p 0.27 RR 1.61(0.71-3.63)13. In the Syntax trial, in which 25% had diabetes and 45% met the criteria for the metabolic syndrome, the results for the whole cohort showed fewer combined cardiovascular events within one year in patients with three-vessel disease but at the expense of an increased risk of stroke in the CABG group14. In the Syntax trial, a higher percentage of patients had complete revascularisation after CABG than after PCI (63.2% vs. 56.7%, p=0.005) and a high SYNTAX score was related to increased events, including major cardiovascular events, in the PCI group but not in the CABG group. Although no specific subgroup analysis of the diabetes patients has yet been reported from the SYNTAX trial this indicates that CABG might still be preferable for patients with diabetes and three-vessel disease and complex lesions. The follow-up time in the SYNTAX trial was only one year, as in many other trials, and our long-term data add further important information, especially as, in the real-life situation, PCI might sometimes be the only choice for patients with diabetes due to co-morbidities.
There could be several explanations for the adverse outcome among diabetic patients. Despite stent implantation, there is an increased risk of re-stenoses and repeat revascularisation among patients with diabetes. Even in non-revascularised areas, there is faster progress in atherosclerosis among these patients. The exact mechanism behind this is not completely understood, but new approaches other than the treatment of traditional risk factors such as lipid disturbances, hypertension and platelet aggregation need to be explored to reduce the accelerated atherosclerosis process among diabetic patients. For instance, elevated glucose levels15 and inflammatory markers7,16 are associated with increased re-stenoses rates and one-year mortality and might be involved in this process. Increased levels of inflammatory markers have been related to increased plaque instability and atherothrombosis17-18 and increased levels of inflammatory markers are seen in patients with diabetes with NSTEMI7. Increased glucose levels are related to increased platelet reactivity in patients with diabetes and there are indications that improved glycaemic control reduces platelet reactivity in type 2 diabetes patients with coronary artery disease undergoing PCI19-21. However, as yet, no trial has tested the effect of glucose control on long-term mortality after PCI. Furthermore, there is an increased problem with non-responders to clopidogrel among patients with diabetes22, especially among those on insulin23, with a corresponding increased risk of adverse outcome24. Another explanation could be the risk of a higher prevalence of silent ischaemia and atypical symptoms among diabetic patients with coronary ischaemia25. A complication with re-stenosis or occlusion after PCI might therefore be undetected and left untreated more frequently among patients with diabetes.
There are several limitations to the present report. As this is a registry analysis, we cannot adjust for concealed confounders, which is especially important to bear in mind when analysing effects of treatment, and the results for GP 2B/3A and stents should therefore be interpreted cautiously. Several important risk factors related to the diabetes disease are missing, as well as other types of evidence-based secondary medical treatment. On the other hand, we believe that the strength of the present analysis is the representation of patients from the ordinary daily situation. The SCAAR registry records all patients in Sweden in whom a PCI is performed, thereby limiting the problem of inclusion bias to the registry. PCI is becoming a more widespread and available treatment for both acute and stable coronary syndromes and to date the long-term results in a modern setting among diabetic patients have been sparse and many randomised trials exclude diabetic patients with other co-morbidities.
In conclusion, long-term mortality is higher in patients with diabetes compared with those without after a first PCI and this risk increases with follow-up time. This risk increase related to diabetes is seen regardless of PCI indication and is even more marked among diabetic patients with stable angina and among those of lower ages. Our findings highlight the importance of increased awareness and aggressive secondary treatment when PCI is chosen in patients with diabetes, regardless of indication.
Acknowledgements
The Swedish Heart- Lung Foundation, the Swedish Federation of County Councils, the Swedish National Board of Health and Welfare and the Swedish Society of Cardiology supported this study.

