Abstract
Aims: We investigated the impact of preadmission diabetic status on long-term outcome in patients with ST-segment elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI), to improve risk stratification.
Methods and results: Between 1997 and 2007, 4,402 STEMI patients were admitted to our hospital and stratified as having insulin-treated diabetes mellitus (ITDM) (n=176), non-ITDM (NITDM) (n=354) and non-DM (n=3,872). Five-year mortality was significantly higher in patients with DM compared to non-DM (29% vs. 18%, p<0.01). After stratification for preadmission glucose-lowering therapy, five-year mortality was significantly higher in ITDM patients compared to NITDM (36% vs. 25%, p=0.01) and in NITDM patients compared to non-DM patients (25% vs. 18%, p<0.01). After adjustment for age and gender the mortality risk between patients with NITDM versus non-DM was comparable (HR: 1.1, 95% CI: 0.9-1.4, p=0.38), in contrast to patients with ITDM (HR: 1.9, 95% CI: 1.5-2.5, p<0.01) and ITDM versus NITDM (HR: 1.7, 95% CI: 1.2-2.4, p<0.01). After adjustment for all baseline characteristics, the results were comparable to the age and gender adjusted model.
Conclusions: ITDM was a strong predictor for long-term mortality when compared to non-DM and NITDM. The mortality between patients without DM and NITDM was comparable after adjustment for age and gender.
Introduction
Timely primary percutaneous coronary intervention (PCI) is currently the preferred treatment for ST-segment elevation myocardial infarction (STEMI)1. Even though primary PCI significantly reduces mortality and morbidity after STEMI compared with thrombolysis2, STEMI patients with diabetes still have a worse prognosis compared to patients without diabetes3-7. Patients with diabetes can be subdivided into those with insulin-treated diabetes mellitus (ITDM) and non-insulin-treated diabetes mellitus (NITDM). Patients with ITDM have either type 1 diabetes or type 2 diabetes with inadequate glycaemic control on oral medication and are well known to be at increased cardiovascular risk compared with patients with NITDM when suffering from coronary atherosclerosis8-11.
Currently, information is limited about clinical outcomes in STEMI patients with ITDM compared to patients with NITDM, treated with primary PCI. Therefore, we investigated long-term five-year mortality in patients with ITDM and NITDM in a large cohort of STEMI patients treated with primary PCI.
Methods
Between 1997 and 2007, a total of 4,931 consecutive and unselected patients were admitted to our hospital with STEMI. Acute STEMI was diagnosed when patients had symptoms of an acute myocardial infarction lasting 30 minutes to 12 hours, accompanied by an electrocardiogram with ST-segment elevation >1 mm (0.1 mV) in ≥2 contiguous leads. Patients were immediately transported to the cardiac catheterisation laboratory and underwent immediate coronary angiography with a view to performing primary PCI. PCI was performed by standard techniques, if the coronary anatomy was suitable. All procedural decisions, including device selection and adjunctive pharmacotherapy, such as glycoprotein IIb/IIIa inhibitors, were made at the discretion of the operator. All patients were treated with heparin (5000 IU) and aspirin (500 mg) prior to PCI. If a coronary stent was implanted, ticlopidine or clopidogrel was prescribed according to the guidelines1.
STUDY COHORT
Data for the 4,931 patients were checked for consistency and completeness. For patients who underwent >1 primary PCI during the study period (n=156), only the first intervention was included in this analysis. Patients with a second primary PCI were followed for mortality in relation to the first primary PCI. Patients treated with rescue PCI for failed intravenous thrombolysis (n=145), patients without confirmed diagnosis of STEMI (n=76) and patients lost to follow-up (n=58) were excluded. The remaining 4,496 patients constitute the present study cohort.
DEFINITION
Upon arrival at the catheterisation laboratory, the diabetic status of the patient was determined by the operator through careful assessment of the past medical history and drug use. After the procedure, the information obtained was entered into our electronic database by qualified cardiac catheterisation laboratory personnel and interventional cardiologists. The patients were categorised into: no diabetes, non-insulin-treated diabetes, insulin-treated diabetes or diabetes with treatment unknown. For patients with unknown treatment or missing information (n=1,037), we reviewed the patient files or contacted the general practitioner. In 94 cases, the information could not be retrieved and these patients were therefore excluded from analysis.
We subsequently identified patients with an established diagnosis of DM (n=530) at the time of admission from our electronic database for the current analysis. Patients with DM were categorised according to preadmission treatment: either with oral medication or diet controlled (NITDM, n=354) or with insulin (ITDM, n=176).
BASELINE DATA
All patients undergoing PCI at our institution were prospectively followed. Baseline clinical, angiographic, and procedural information was entered by qualified cardiac catheterisation laboratory personnel and interventional cardiologists in a dedicated electronic database.
FOLLOW-UP
Information on the vital status was obtained from the Dutch national population registry (Statistics Netherlands, Voorburg, The Netherlands).
PRIMARY OBJECTIVE
The primary objective of the present analysis was to evaluate all-cause five-year mortality of patients with different diabetic status, reflected by their preadmission glucose-lowering treatment.
STATISTICAL ANALYSIS
Discrete variables were summarised as frequencies and percentages. Differences in baseline characteristics between the groups were tested for significance using the χ2 test. Statistical significance was defined as a p-value <0.05. Cumulative event rates of all-cause death were estimated using the Kaplan-Meier method. The log-rank statistic was used to test for significant differences in mortality between the groups. Follow-up for mortality was censored at the date of last follow-up by checking vital status in the Dutch population registry, or at five years, whichever came first. Cox proportional hazards regression analysis was performed to correct for other baseline characteristics after verification of the proportional hazards assumption.
For the primary analysis, we only corrected for age (continuous variable, per year increment) and gender differences, as an assessment of prognosis is only relevant when the effect of age and gender is neutralised. To obtain the age and gender adjusted survival curves from the Cox proportional hazards model, we used the mean of covariates method, which is based on the regression estimates and the average covariate values in the study groups.
A secondary analysis with all other baseline characteristics was performed for illustrative purposes only, namely: preadmission glucose-lowering therapy as a categorical value with non-DM as reference, hypertension, smoking, hypercholesterolaemia, family history of cardiovascular disease, body mass index (BMI), previous myocardial infarction (MI), shock, left anterior descending coronary artery related MI, multivessel disease and preprocedural Thrombolysis In Myocardial Infarction (TIMI) flow grade 3. The multivariable model was built by stepwise backward variable elimination with entry and exit criteria set at the p=0.1 level.
Results
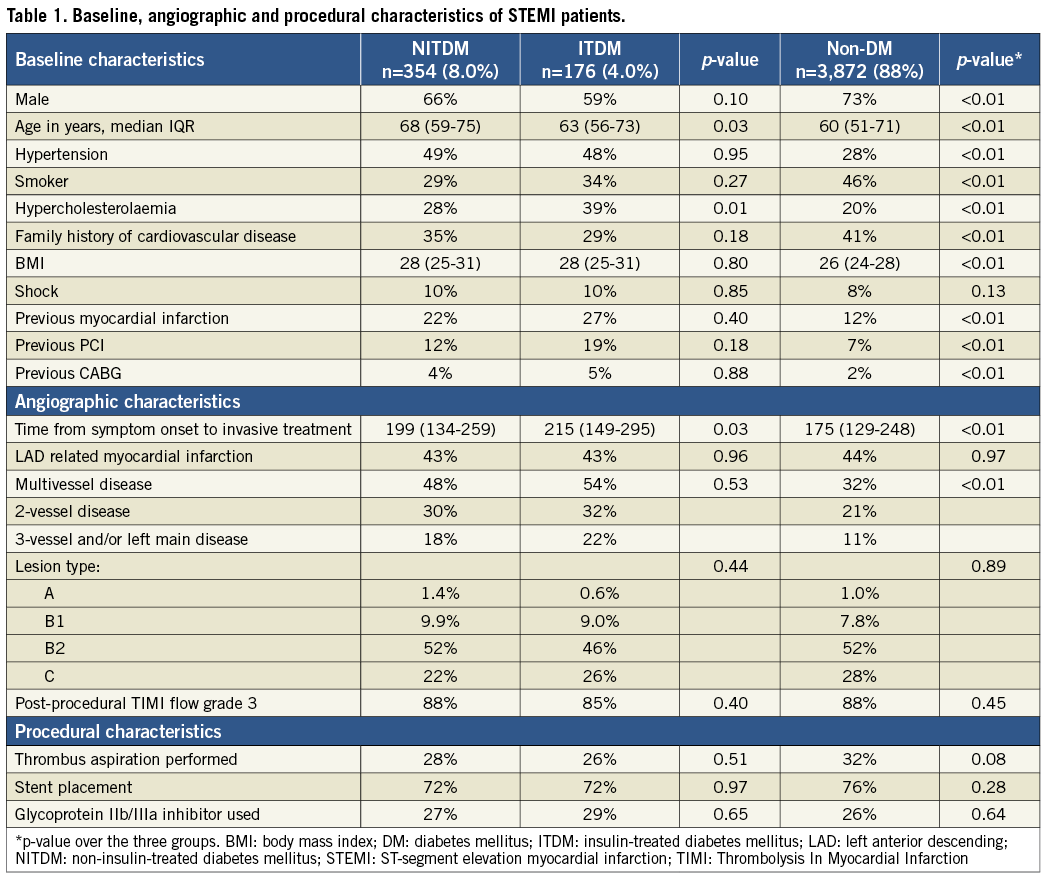
The final study cohort consisted of 4,402 STEMI patients treated with primary PCI. Of these patients, 530 (12%) had a confirmed diagnosis of DM at admission, of whom 176 (33%) had ITDM and 354 (67%) NITDM. Median follow-up duration was 3.9 years (IQR: 2.3-5 years). Table 1 shows baseline, angiographic and procedural characteristics for 530 STEMI patients for whom preadmission glucose-lowering therapy was known and 3,872 patients without DM. Patients with DM in comparison to patients without DM were older, more often female, had a higher BMI and a higher prevalence of hypertension, hypercholesterolaemia, previous MI, previous PCI, previous coronary artery bypass graft surgery (CABG) and multivessel disease. However, they had a lower prevalence of current smoking and positive family history of cardiovascular disease. Patients with NITDM in comparison to ITDM were older and more often male. Patients with ITDM had a higher prevalence of hypercholesterolaemia.
PRIMARY ANALYSIS
Unadjusted Kaplan-Meier survival curves up to five years after primary PCI are shown in Figure 1. At five years, the estimated mortality rate was significantly higher in patients with DM compared to those without DM (29% vs. 18%, p<0.01) (Figure 1A). After stratification for preadmission glucose-lowering therapy, cumulative five-year mortality was significantly higher in ITDM patients compared to NITDM (36% vs. 25%, p=0.01) and NITDM patients compared to non-DM patients (25% vs. 18%, p<0.01) (Figure 1B). The majority of these patients died during the first 30 days after the index event with the highest mortality in the ITDM group (18%), intermediate in the NITDM group (10%), and the lowest mortality rate in the non-DM group (8%).
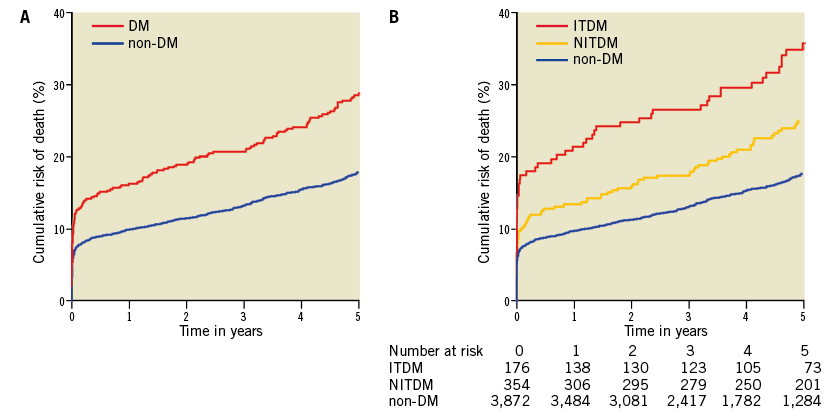
Figure 1. Long-term mortality in STEMI patients. A) Stratified by diabetic status. B) Stratified by preadmission glucose-lowering therapy. DM: diabetes mellitus; ITDM: insulin-treated diabetes mellitus; NITDM: non-insulin-treated diabetes mellitus; STEMI: ST-segment elevation myocardial infarction
Figure 2 shows the age and gender adjusted survival rates. After adjustment, there appeared to be a comparable mortality risk between patients with NITDM and patients without DM (HR: 1.1, 95% CI: 0.9-1.4, p=0.38), in contrast to patients with ITDM (HR: 1.9, 95% CI: 1.5-2.5, p<0.01) and ITDM versus NITDM (HR: 1.7, 95% CI: 1.2-2.4, p<0.01).
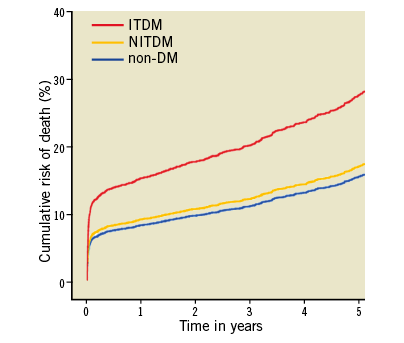
Figure 2. Age and gender adjusted survival rates in STEMI patients stratified by preadmission glucose-lowering therapy. DM: diabetes mellitus; ITDM: insulin-treated diabetes mellitus; NITDM: non-insulin-treated diabetes mellitus; STEMI: ST-segment elevation myocardial infarction
SECONDARY ANALYSIS
After multivariate adjustment for all other baseline characteristics, the results were comparable to the age and gender adjusted model (NITDM vs. non-DM, HR: 1.0, 95% CI: 0.8-1.3, p=0.95, ITDM vs. non-DM, HR: 1.8, 95% CI: 1.4-2.3, p<0.01, and ITDM versus NITDM, HR: 1.8, 95% CI: 1.3-2.5, p<0.01).
Discussion
The present analyses confirmed that in STEMI patients DM is associated with increased mortality. However, when stratified for preadmission diabetic status reflected by glucose-lowering therapy, ITDM was a strong predictor for long-term mortality when compared to non-DM as well as to NITDM alone. After correction for age and gender, the risk of mortality was comparable between NITDM and non-DM patients.
The impact of DM on adverse outcome after percutaneous treatment for STEMI is already known and has been extensively described previously4-7. However, information regarding preadmission diabetic status on clinical outcome is scarce, especially in the percutaneous reperfusion era4,12. To the best of our knowledge, this is the first study evaluating the impact of preadmission diabetic status on long-term five-year mortality in STEMI patients treated with primary PCI. A previous report from our centre evaluated one-year cumulative mortality only4. In the current study, we increased the study period and as a result significantly increased the cohort size.
Type 1 diabetes is characterised by destruction of the pancreatic beta cells, leading to absolute insulin deficiency. This is usually due to autoimmune disease developing at a young age. However, the fact that our diabetes patients were older than our non-DM patients argues against a large proportion of type 1 diabetes patients in our cohort. Type 2 diabetes is characterised by a variable degree of insulin resistance treated with oral glucose-lowering medication. However, over time patients with type 2 diabetes often lose beta cell function leading to relative insulin deficiency necessitating insulin treatment. The progression of the disease was also reflected in the baseline characteristics of our cohort. Patients with ITDM had a higher prevalence of hypercholesterolaemia, previous MI and multivessel disease which is an indicator of the extent of the coronary artery disease. This observation emphasises the fact that ITDM seems to be associated with a more severe cardiovascular risk profile. Besides the increased baseline risk profile of ITDM patients, another explanation for the augmented mortality could be the presence and extent of neuropathy leading to silent ischaemia, impaired sensation of myocardial ischaemic pain, delayed diagnosis, delayed referral and as a result postponed treatment13,14. In our cohort, the time from symptom onset to invasive treatment was known in 65% of all patients and increased significantly from non-DM (median: 175 minutes, IQR: 129-248) to NITDM (median: 199 minutes, IQR: 134-259) and ITDM (median: 215 minutes, IQR: 149-295, p-value <0.01). Another explanation was proposed by Antoniucci et al who evaluated the impact of preadmission glucose-lowering therapy on six-month outcome in a smaller STEMI cohort (n=1,061)12. They observed that ITDM was associated with worse early ST-segment resolution, suggesting less effective reperfusion and myocardial salvage in this subset of patients despite successful procedural outcome15-17. Several causative factors were suggested, for example an already damaged microcirculation18, increased procedural risk for atherothrombotic embolism, decreased cell viability due to the metabolic disorder of the diabetic status, and decreased myocardial resistance to ischaemia due to poor collateral flow17,19.
Antoniucci et al reported a similar observation of a comparable mortality rate between non-DM and NITDM with an increased mortality rate in the ITDM group. One may argue that the comparable risk of mortality is facilitated by a higher incidence of CABG in the NITDM group versus the non-DM group, as the Bypass Angioplasty Revascularization Investigation (BARI) trial20 demonstrated that, for patients with treated diabetes mellitus and multivessel coronary artery disease who were candidates for either CABG or PCI, initial CABG was associated with a markedly lower five-year mortality rate relative to initial PCI (19.4% vs. 34.5%, respectively, p<0.01). However, these results were not consistent in subsequent randomised controlled trials or registries21-24. To address this issue, we investigated the proportion of patients who received CABG in our centre during the follow-up period. The proportions were equally divided among the three groups: non-DM: 3.2%, NITDM: 4.2% and ITDM: 3.4%, p=0.54.
Besides the mechanisms described above, there is an ongoing debate about the possible adverse effects of insulin itself. On the one hand, intensive glucose control with insulin reduces the long-term risk of cardiovascular disease and all-cause death, whereas on the other hand insulin treatment might be associated with pro-atherogenic effects25,26. In this perspective, a comparable mortality rate between patients without diabetes and patients with non-insulin-treated diabetes seems logical although a very simple explanation could account for this finding. The prevalence of type 2 diabetes increases with age and therefore it is particularly observed in the elderly27,28. This will probably explain the observed finding of a non-significant mortality difference between non-DM and NITDM after multivariate adjustment and adjustment for age in particular (Figure 2). The mechanisms behind this phenomenon have not been fully clarified; however, it has been suggested that with increasing age the insulin sensitivity decreases, in which an inactive lifestyle, unhealthy diet and weight gain play a significant role29. Furthermore, it is hypothesised that pancreatic beta-cell function decreases over time28.
Study limitations
Several limitations should be mentioned. In this study, the diagnosis of diabetes mellitus was based on a known history of DM at admission and preadmission glucose-lowering treatment. We did not routinely measure haemoglobin A1c or test for DM during admission. In addition, detailed information on subsequent treatments (e.g., medication, PCI, surgery) was not available. However, upon acute presentation to the catheterisation laboratory, this information is also unknown and therefore it cannot be taken into account for an estimation of the prognosis, which is made during the primary PCI procedure. As the BARI trial suggested that CABG versus PCI can improve survival in patients with diabetes, we investigated the proportion of CABG during the follow-up period performed in the Academic Medical Center. However, the primary PCI region is much larger than the CABG region. Therefore, not all patients receiving CABG will be treated in our centre. Nevertheless, there was no significant difference between the incidence of CABG and the presence of DM.
Conclusion
Our study confirms previous reports on the unfavourable prognostic impact of DM after STEMI and extends this knowledge by providing long-term outcome stratified by preadmission diabetic status, reflected by glucose-lowering therapy. ITDM was a strong predictor when compared to non-DM as well as to NITDM alone. After correction for age and gender, the risk for mortality was comparable between patients without diabetes and patients with non-insulin-treated diabetes.
| Impact on daily practice Even in the era of primary PCI, STEMI patients with diabetes still have a worse prognosis when compared with patients without diabetes. In our analyses, we found that long-term survival is severely reduced in patients with ITDM whereas there was a comparable survival rate in patients with NITDM and patients without DM after correcting for age and gender. These analyses identify ITDM patients as a subgroup with an increased mortality risk in whom post-STEMI care needs to be carefully regulated. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

