Abstract
Aims: The aim of this substudy was to determine the five-year correlates of non-TV-related adverse events (AE) in STEMI patients included in the EXAMINATION trial.
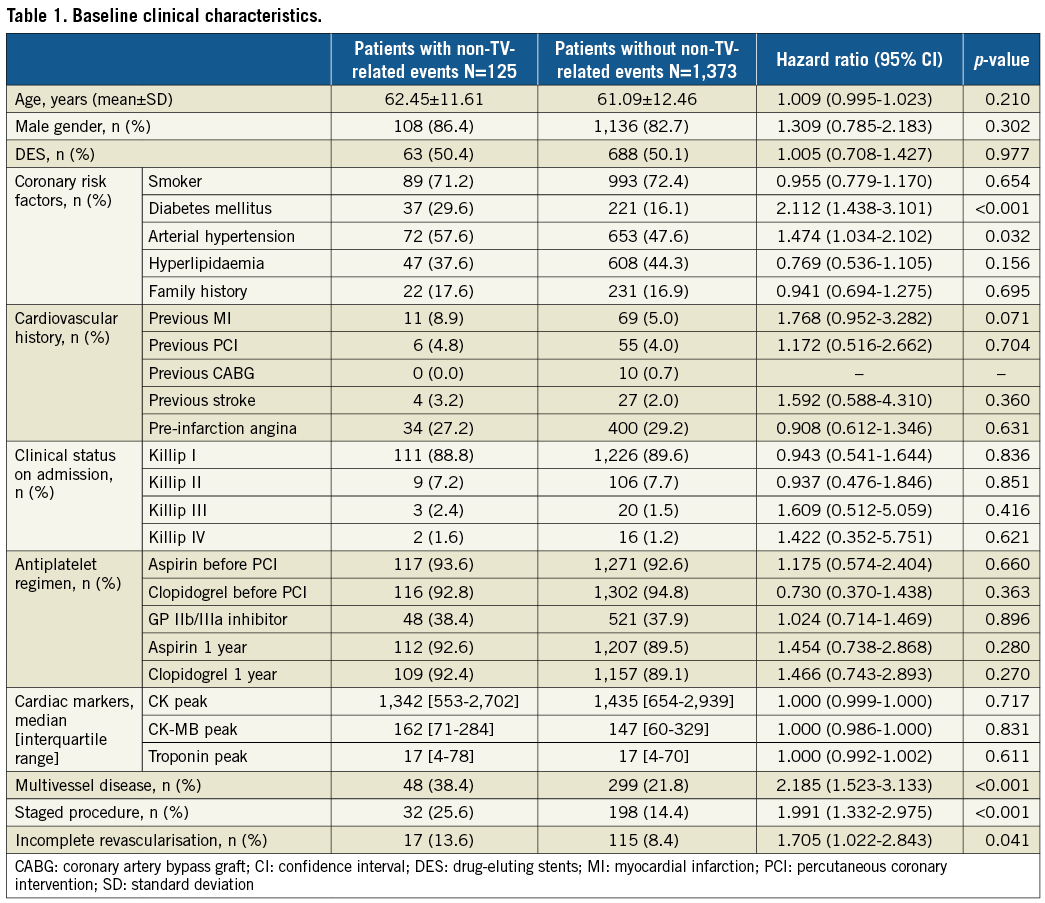
Methods and results: The EXAMINATION trial randomised 1,498 STEMI patients to bare metal or everolimus-eluting stent implantation. In this substudy, patients were analysed according to non-TV-related AE, defined as the composite of either non-TV revascularisation (non-TVR) or non-TV-related myocardial infarction (MI). At five-year follow-up, 125 patients (8.3%) exhibited 136 non-TV-related AE (124 [8.3%] non-TVR, 12 [0.8%] non-TV-related MI), accounting for 47.1% of 289 non-fatal cardiac events overall. These patients had a higher incidence of diabetes mellitus (p<0.001), arterial hypertension (p=0.032), previous MI (p=0.073), multivessel disease (p<0.001), and incomplete revascularisation (p=0.049), and a lower rate of ST-segment resolution >70% (p=0.042) as compared to the rest. At Cox analysis, previous MI (HR 1.872, 95% CI: 1.004-3.489; p=0.048), incomplete revascularisation (HR 1.746, 95% CI: 1.029-2.963; p=0.039) and diabetes (HR 1.942, 95% CI: 1.292-2.919; p=0.001) were independent correlates of non-TV-related AE.
Conclusions: In STEMI patients undergoing primary percutaneous coronary intervention, previous MI, incomplete revascularisation and diabetes resulted in being independent correlates of five-year non-TV-related AE.
Abbreviations
ACS: acute coronary syndrome
ARC: Academic Research Consortium
CABG: coronary artery bypass graft
CAD: coronary artery disease
DES: drug-eluting stent
IR: incomplete revascularisation
MACE: major adverse cardiovascular events
MI: myocardial infarction
MVD: multivessel disease
Non-TV: non-target vessel
Non-TV-related AE: non-target vessel-related adverse events
Non-TVR: non-target vessel revascularisation
PCI: percutaneous coronary intervention
STEMI: ST-elevation myocardial infarction
Introduction
Drug-eluting stent (DES) trials focus mainly on device performance in terms of target lesion events1. Conversely, data on events related to non-target vessels (non-TV) are limited, especially in a specific population such as ST-elevation myocardial infarction (STEMI)2. In patients with acute coronary syndrome (ACS) and multivessel disease (MVD) who underwent culprit only percutaneous coronary intervention (PCI), it has been demonstrated that 50% of total cardiac events are related to non-TV at three-year follow-up3. Although complete revascularisation can reduce the risk of major adverse cardiovascular events (MACE)4 in these patients, non-TV-related adverse events (AE) still account for almost a half of cardiac events5, strengthening the concept of coronary atherosclerosis as a diffuse and progressive disease that goes beyond the treatment of a single coronary lesion.
We therefore sought to analyse the incidence and correlates of non-TV-related AE at five-year follow-up in the STEMI patients included in the EXAMINATION trial6.
Methods
STUDY POPULATION
This is a post hoc analysis from the all-comers, multicentre, controlled, and randomised, EXAMINATION trial (A Clinical Evaluation of Everolimus Eluting Coronary Stents in the Treatment of Patients With ST-segment Elevation Acute Myocardial Infarction: EXAMINATION Study) (NCT00828087). The detailed study design and five-year results of the EXAMINATION trial have been reported previously6,7. The EXAMINATION trial randomised 1:1 a total of 1,498 STEMI patients to an everolimus-eluting stent (n=751) (XIENCE®; Abbott Vascular, Santa Clara, CA, USA) or a MULTI-LINK VISION® BMS (n=747) (Abbott Vascular). All participating centres submitted and received the approval of their medical ethics committee for the protocol and for the informed consent. The study was conducted in compliance with the protocol, the Declaration of Helsinki, and applicable local requirements. All patients provided written informed consent.
ENDPOINTS AND DEFINITIONS
All the patients were analysed according to the incidence of non-TV-related AE, defined as the composite of non-TV revascularisation (non-TVR) or non-TV-related myocardial infarction (MI), as per the Academic Research Consortium (ARC) definitions8. Because death cannot be assigned to any vessel segment, it was not counted as a TV or non-TV-related event. Incomplete revascularisation (IR) was defined as a residual stenosis of ≥50% in the left main coronary artery or ≥70% in another major epicardial coronary artery on the basis of operator visual estimation. Staged procedures were all performed within the first month after discharge and with the same stent as per randomisation. Therefore, incomplete revascularisation was evaluated after staged procedures were performed. Any revascularisation carried out after this time was counted as an unplanned intervention per protocol. Definitions of death (all-cause and cardiac) and stent thrombosis have already been reported7,9. All clinical events were adjudicated by an independent clinical events committee (Cardialysis, Rotterdam, the Netherlands).
STATISTICAL ANALYSIS
Continuous variables were expressed as mean±standard deviation or median and interquartile range, according to their distribution, and were compared by ANOVA or Wilcoxon rank-sum test. Categorical variables were expressed as numbers and percentages and were compared by chi-square analysis or Fisher’s exact test, as appropriate.
In order to analyse independent correlates of five-year non-TV-related AE, baseline clinical, procedural, and angiographic characteristics were tested in a univariable analysis. Those variables with p<0.10 at the univariable analysis were then entered into a Cox multivariable model with backward elimination. MVD and staged procedure were not entered into the Cox model in order to avoid any multicollinearity with incomplete revascularisation, which conversely was included. Any relation between non-TV-related AE and TV-related AE, all-cause mortality and cardiac death was examined using a Cox regression model with non-TV-related AE as a time-varying covariate. In patients experiencing both a TV and a non-TV-related AE, we considered only those TV events that occurred after a non-TV-related AE.
Results from Cox regression analyses were reported as hazard ratios (HR) with associated 95% confidence intervals and p-values. A two-tailed p-value <0.05 was considered to be statistically significant. Statistical analyses were performed using SPSS, Version 20.0 (IBM Corp., Armonk, NY, USA).
Results
POPULATION
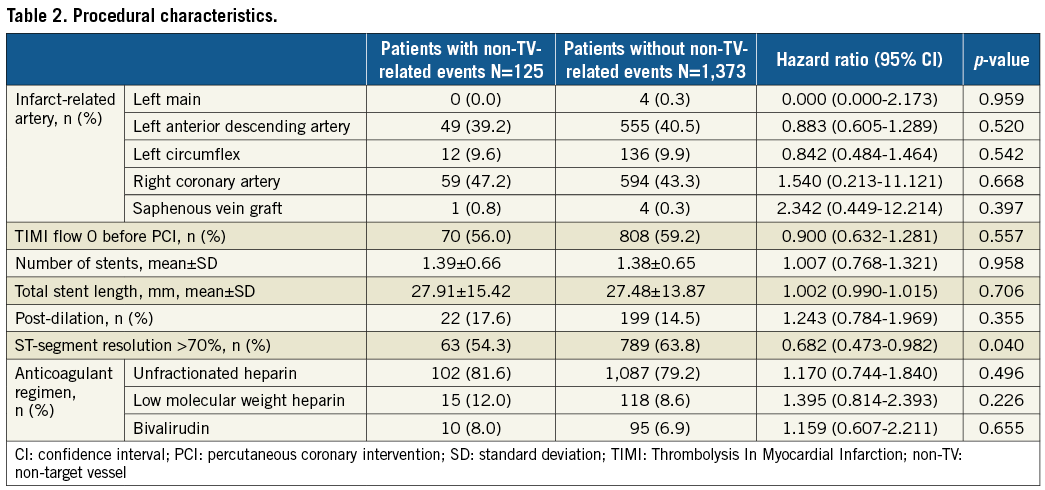
Complete five-year clinical follow-up was available in 97% of patients. At five-year follow-up, 125 patients (8.3%) exhibited 136 non-TV-related AE (124 [8.3%] non-TVR, 12 [0.8%] non-TV-related MI), accounting for 47.1% of 289 non-fatal cardiac events overall (Figure 1). Table 1 shows baseline clinical characteristics. Patients in the non-TV-related AE group had a higher incidence of diabetes mellitus (p<0.001), arterial hypertension (p=0.032), previous myocardial infarction (p=0.073), MVD (p<0.001), staged procedure (p<0.001), and incomplete revascularisation (p=0.049), and a lower rate of ST-segment resolution >70% (p=0.042) as compared to the other group. No other differences were found between the groups (Table 1, Table 2).
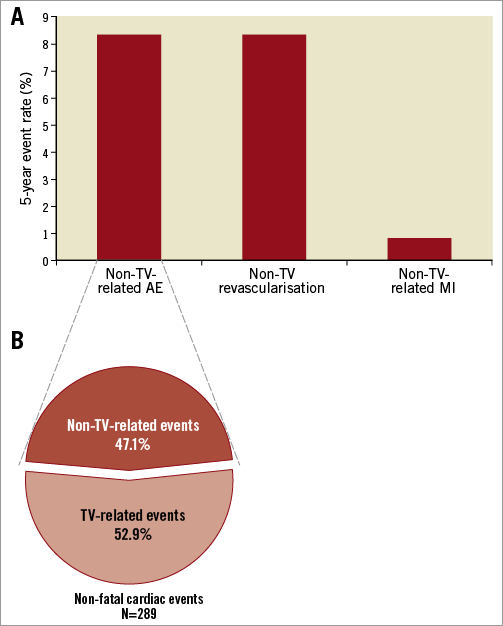
Figure 1. Non-TV-related adverse events. A) Incidence of non-TV-related adverse events, non-TV revascularisation and non-TV-related myocardial infarction. B) Proportion of non-TV-related adverse events of total non-fatal cardiac events. MI: myocardial infarction; Non-TV-related AE: non-target vessel-related adverse events; TV: target vessel
CORRELATES OF NON-TARGET VESSEL-RELATED ADVERSE EVENTS
At Cox analysis, previous MI (HR 1.872, 95% CI: 1.004-3.489, p=0.048), incomplete revascularisation (HR 1.746, 95% CI: 1.029-2.963, p=0.039) and diabetes (HR 1.942, 95% CI: 1.292-2.919, p=0.001) were independent correlates of non-TV-related AE (Figure 2).
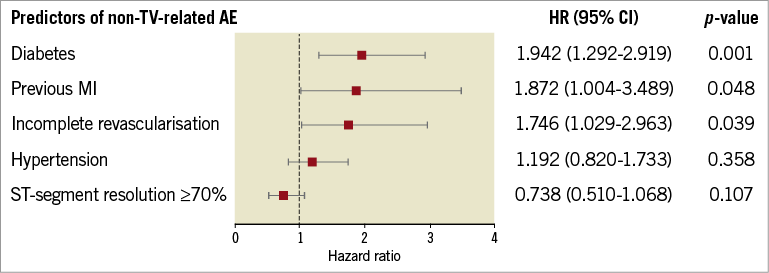
Figure 2. Correlates of non-TV-related AE at five-year follow-up. AE: adverse events; CI: confidence interval; HR: hazard ratio; MI: myocardial infarction; non-TV: non-target vessel
Patients who experienced a non-TV-related AE had a higher risk of target vessel-related AE (HR 2.919, 95% CI: 1.556-5.478, p<0.001) (Table 3), even after adjustment (adjusted HR 2.818, 95% CI: 1.470-5.404, p=0.002), with no significant effect modification by type of stent implanted (HR for BMS: 2.011, 95% CI: 0.765-5.285; HR for DES: 3.095, 95% CI: 1.625-9.676; p for interaction: 0.222). Non-TV events did not have a significant impact on cardiac death (HR 0.752, 95% CI: 0.274-2.059, p=0.579) or all-cause mortality (HR 0.891, 95% CI: 0.435-1.825, p=0.753). Similarly, TV-related AE did not increase the risk of cardiac death (HR 0.891, 95% CI: 0.435-1.825, p=0.753) or all-cause mortality (HR 1.357, 95% CI: 0.624-2.950, p=0.442).
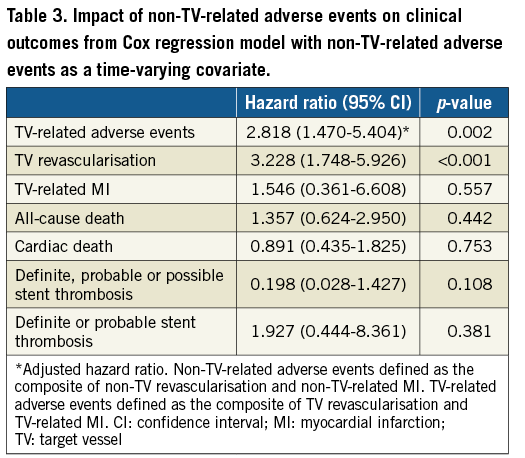
In addition, median time from index procedure to non-TV events (median: 113 days; interquartile range: 44-604 days) and to TV events (median: 196 days; interquartile range: 27.5-678 days) was not statistically different (p=0.96).
Discussion
Our analysis showed that: 1) the cumulative incidence of non-TV-related adverse events in STEMI patients treated with primary PCI was 8.3% at five years, accounting for 47.1% of total adverse events; 2) previous MI, incomplete revascularisation, and diabetes appeared to be independent correlates of non-TV-related AE in our study population; 3) non-TV-related adverse events are associated with a higher incidence of TV-related adverse events.
Coronary artery disease (CAD) progression involves the entire coronary tree and could be responsible for events in areas remote from the culprit vessel. Previous studies have already reported the rate of this phenomenon in various populations. Cutlip et al found that, in a low-risk population, the non-TVR cumulative rate was 21.7% at five-year follow up10. In the SIRIUS trial11, events attributed to non-TV were estimated at 26% after five years from the index procedure. Similarly, a single-centre all-comers Japanese study showed that the rate of non-TV repeat PCI was 17.6% at five-year follow-up12. Compared to these studies, we report a lower rate of events in the non-culprit vessels, which accounted for almost 50% of cardiac events overall. This lower rate of events could be explained in several ways. Firstly, the aforementioned findings might have been influenced by protocol-driven repeat coronary angiographies, whereas the events in our analysis were clinically driven. In addition, patients included in the previous studies had a higher CAD burden. In fact, MVD was present in up to 70% of those patients while in our population the prevalence of MVD was 30.1%. This could also be related to the fact that we included only STEMI patients, who usually have a lower prevalence of MVD compared with other ACS patients13. In our population, the incidence of non-TV-related revascularisation was not statistically different between patients receiving bare metal stents and those receiving DES (8.3% vs. 8.3%, p=0.975), even when considering patients who underwent a staged procedure in non-TV (15.8% vs. 11.6%, p=0.353).
With regard to prognostic factors, in the present report we found that previous MI, incomplete revascularisation, and diabetes appeared to be independent factors of non-TV-related AE. It is already known that STEMI patients who have had a previous MI have worse long-term clinical outcomes14. Our findings are consistent with previous studies as we showed that previous MI is associated with an increased risk of non-TV-related AE. This could be explained by considering that STEMI patients who have experienced a previous MI could have a more extensive and complex CAD. Regarding the completeness of coronary revascularisation, it has been demonstrated that MVD, which is found in approximately 40-60% of STEMI patients, is associated with bad short- and long-term prognosis15. Several studies have analysed the effects of complete revascularisation on outcomes, but contrasting results have been reported. A recently published meta-analysis of eight studies showed that, in STEMI patients, complete revascularisation reduced the risk of MACE and repeat revascularisation, compared to incomplete revascularisation16. Two recent randomised controlled trials have shown that the fractional flow reserve-guided treatment of non-culprit vessels in STEMI patients reduced MACE at 12- to 24-month follow-up4,17. However, these studies examined MACE without giving information on non-TV-related adverse events. Our study, which has a longer follow-up (60 months), focused on these events and showed that incomplete revascularisation is an independent risk factor for non-TV-related AE. In addition, we found that, out of 17 non-TV-related AE occurring in patients with incomplete revascularisation, 13 were clinically driven non-TV revascularisations and that they occurred in the first three months after PCI. Therefore, we might hypothesise that these events could be related to lesions that were not treated immediately and that had an early impact on patients’ symptoms, confirming the protective role of the complete revascularisation even in the first months after PCI.
Diabetes is an established risk factor for CAD and future cardiac events in patients who undergo PCI, mainly because of an increased risk of stent restenosis and MI during follow-up18. However, diabetes also plays a central role in the progression of atherosclerotic disease and it has been recognised as a negative prognostic factor for non-TV events. An intravascular coronary ultrasound analysis which included 237 coronary segments from 45 patients enrolled in the DIABETES I, II and III trials19-21 showed that insulin-dependent diabetes was associated with vessel shrinkage and disease progression, both in treated and in not previously treated lesions22. In the PROSPECT trial, patients with insulin-requiring diabetes had a threefold increased risk of non-culprit lesion-related MACE at three-year follow-up3. In addition, a recent propensity-matched sub-analysis of the PROSPECT trial showed that the three-year total MACE rate was significantly higher in patients with diabetes versus those without, mainly driven by a higher rate of non-culprit lesion-related MACE23. Accordingly, in our study population diabetes was the strongest predictor with almost a twofold risk of non-TV-related AE at five-year follow-up. This slightly lower risk of adverse events, as compared to the PROSPECT trial, could be related to the fact that we included all diabetic patients, regardless of insulin or oral glucose-lowering medication use.
Interestingly, our analysis also showed that non-TV-related AE, despite the lack of a significant impact on all-cause mortality and cardiac death, are associated with a higher incidence of TV-related AE, in particular TVR. In addition, no statistically significant difference was found in the occurrence of any stent thrombosis between the two groups. The strong relation between non-TV and TV-related AE is a novel finding, which confirms the concept of CAD as an extensive disease. Therefore, our findings underline the fact that both complete revascularisation and an aggressive control of all cardiovascular risk factors (in particular diabetes) could be effective in the prevention of non-TV-related AE at long-term follow-up.
Limitations
This study has several limitations. Firstly, it is a post hoc analysis and therefore our results should be considered hypothesis-generating. Secondly, there were baseline differences between both groups in terms of patient, clinical, lesion, and procedural characteristics; despite these differences, an adequate statistical treatment was performed in order to minimise their impact on the results. Neither prasugrel nor ticagrelor had been approved for use in clinical practice at the time this study was conducted, thus all patients were treated with clopidogrel. Moreover, we took into account only anatomical incomplete revascularisation rather than the functional residual CAD.
Although non-TV-related AE did not increase the risk of more prognostically relevant events such as death or myocardial infarction, 95% confidence intervals were wide, suggesting imprecision and uncertainty on the assessed relationship.
Lastly, patients with previous revascularisation (with either PCI or coronary artery bypass graft [CABG]) were not excluded from the analysis; therefore, a non-TV AE could relate to a stent or graft failure rather than to a disease progression. However, only six patients, out of the 125 patients who experienced a non-TV adverse event, had undergone a previous PCI and none of them had undergone a previous CABG. This small number of patients should not have affected the results.
Conclusions
In STEMI patients undergoing primary PCI, incomplete revascularisation, previous MI and diabetes resulted in being independent correlates of five-year non-TV-related AE.
| Impact on daily practice Our findings might help in the identification, at the time of primary PCI, of those patients at risk of future events related to areas remote from the target vessel. Complete revascularisation at the index procedure and more aggressive risk factor control, in particular diabetes, could reduce the occurrence of non-target vessel-related adverse events at long-term follow-up. |
Guest Editor
This paper was guest edited by Lorenz Räber, MD, PhD; University Hospital Bern, Bern, Switzerland, and Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat, Paris, and University Paris VII, Paris, France.
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor Lorenz Räber has no conflicts of interest to declare. The Guest Editor Alec Vahanian is a consultant for Edwards Lifesciences.