Abstract
Aims: Despite technical advancements, long-term outcomes after chronic total occlusion (CTO) recanalisation remain a subject of debate, especially in diabetic patients. The aim of this study, therefore, was to assess the very long-term clinical outcome of diabetic vs. non-diabetic patients in a large cohort from a high-volume CTO PCI centre according to whether or not CTO recanalisation had been successfully achieved.
Methods and results: Between 2004 and 2012, 1,320 consecutive patients underwent PCI for CTO, 27.4% (362/1320) of whom were diabetics. We compared cardiac death, target lesion revascularisation (TLR), myocardial infarction (MI) and combined major adverse cardiac events (MACE) in patients with successful versus failed PCI (median follow-up 4.2 years). The PCI success rate was 75% (990/1,320 patients), with no significant differences between diabetics and non-diabetics (69.8% vs. 75%, respectively, p=0.07). Successful recanalisation was associated with lower cardiac death rates (13.2% vs. 17.2%, respectively, p<0.001) and lower MACE (27.5% vs. 33.7%, respectively, p=0.02). There were no significant differences in TLR (8.9% vs. 14.2% for failed recanalisation, p=0.29) and MI (4.7% vs. 10% for failed recanalisation). Successful recanalisation was a predictor of survival (HR 0.5, 95% CI: 0.32-0.81, p=0.005), whereas diabetes (HR 2.44, 95% CI: 1.52-3.83, p<0,001), left ventricular ejection fraction (HR 0.96, 95% CI: 0.94-0.99, p=0.004) and age (HR 1.06, 95% CI: 1.03-1.08, per year increment, p<0.0001) were predictors of cardiac death at follow-up. Cardiac mortality rates varied markedly after failed PCI between diabetic (20/103, 24.7%) and non-diabetic patients (15/227, 9.3%, p<0.0001 for comparison between groups), suggesting an interaction between the presence of diabetes and procedural outcome.
Conclusions: CTO recanalisation was associated with improved long-term survival, a reduced rate of MACE for up to nine years, and suggests a greater reduction in cardiac death among diabetic patients.
Introduction
Despite substantial improvements in dedicated devices and technical strategies1, the procedural success rate of percutaneous coronary intervention (PCI) in chronic total occlusion (CTO) is still lower than that achieved for non-CTO lesions (ranging from 50%-88% vs. >95%, respectively)2. Several studies3-5, including a meta-analysis6, have shown higher rates of midterm to long-term survival after successful compared to failed PCI of CTOs; however, the optimal benefits of coronary CTO recanalisation remain the subject of debate due to procedural complexity7, increased radiation exposure8 and higher risks of serious complications compared with non-CTO interventions.
The pandemic nature of diabetes mellitus (DM), with the more than 171 million individuals currently affected worldwide projected to increase to 366 million by 20309, is a matter of serious concern, given that diabetes increases the incidence of cardiovascular disease leading to significant morbidity and mortality10,11. While revascularisation has been significantly correlated to a decrease in major adverse cardiac events (MACE) in diabetic patients, there are no available data in the setting of CTO from randomised trials vs. medical therapy. In addition, existing data on late outcomes are restricted to a few studies with limited follow-up, which may appear as relatively obsolete in view of the latest developments in CTO devices and technical strategies12,13.
The aim of this study, therefore, was to assess the very long-term clinical outcome of diabetic vs. non-diabetic patients in a large cohort from a high-volume CTO PCI centre (≥200 CTO procedures per year) according to whether or not CTO recanalisation had been successfully achieved.
Methods
PATIENTS
Consecutive patients from Hôpital Privé Jacques Cartier, Massy, Hôpital Privé Claude Galien, Quincy and GVM La Roseraie, Aubervilliers, France were entered into this prospective registry between 2004 and 2012. Eligibility criteria included the presence of at least one CTO of a principal artery (diameter >2.5 mm, supplying a large myocardial territory), and symptomatic angina and/or a positive functional ischaemia stress test. Diabetes was defined as fasting plasma glucose ≥7.0 mmol/l (126 mg/dl) or 2-hr plasma glucose ≥11.1 mmol/l (200 mg/dl)14.
PROCEDURE
PCI of the CTO and stent implantation were carried out in the standard manner via contemporary techniques such as bilateral injection, using specialised hydrophilic, tapered tip, and stiff wires, parallel wires, microcatheters and the retrograde approach when these became available. Drug-eluting stents (DES) were implanted in more than 90% of patients, using 6 Fr guiding catheters via the radial approach as the default strategy (>60% cases). In patients with ≥2 attempted CTOs, PCI was considered a success in cases where one of the lesions was successfully reopened, even if revascularisation of the other CTO was not achieved.
After PCI, all patients were prescribed dual antiplatelet therapy (DAPT) in compliance with current guidelines. Patients were followed by telephone interview, outpatient visit or physician contact. The adjudication of adverse events was carried out by an internal committee composed of investigators and research assistants blinded to CTO procedural success.
DEFINITIONS
A CTO was defined as a native coronary artery obstruction with TIMI grade 0 flow estimated to be older than three months on the basis of a history of sudden chest pain, previous myocardial infarction (MI) in the same target vessel territory, or according to the time elapsed between coronary angiography diagnosis and PCI1. Procedural success was defined as successful recanalisation and dilation (<50% residual stenosis and TIMI grade 3 flow) of a CTO lesion with or without stent implantation.
Cardiac death, myocardial infarction (MI) and target lesion revascularisation (TLR) were defined according to the Academic Research Consortium definitions15 as follows:
– Cardiac death was defined as any death due to a proximate cardiac cause (e.g., MI, low-output failure, fatal arrhythmia), unwitnessed death and all procedure-related deaths, including those related to concomitant treatment. Death from uncertain causes was also classified as cardiac death.
– Non-cardiac death was defined as a death not due to cardiac causes (as defined above).
– MI was defined as a detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99th percentile of the upper reference limit (URL) together with evidence of myocardial ischaemia (symptoms of ischaemia; ECG changes indicative of new ischaemia; development of pathological Q-waves in the ECG; imaging evidence of new loss of viable myocardium or new regional wall motion abnormality).
– TLR was defined as any repeat PCI of the target lesion or coronary artery bypass graft (CABG) of the target vessel performed for restenosis or any other complication of the target lesion. The target lesion was defined as the treated segment from 5 mm proximal to the stent to 5 mm distal to the stent. In the absence of systematic angiographic follow-up examination, indication for TLR was clinically driven.
The MACE endpoint was defined as a device-oriented composite of cardiac death, MI and TLR.
STATISTICAL ANALYSIS
Data are presented as mean±SD, or as percentages; follow-up is presented as median and IQR. Differences between patients with a failed vs. successful procedure, in terms of baseline clinical, angiographic and PCI characteristics, were compared using the Student’s t-test or Wilcoxon rank-sum test for continuous variables, and the chi-square or Fisher’s exact test for categorical variables, as appropriate. Normal distribution was assessed by the Shapiro-Wilk test. Cumulative incidence rates of individual and composite outcomes were estimated using the Kaplan-Meier method and compared with the log-rank test.
Data on patients who were lost to very long-term follow-up were censored at the time of the last contact. Cox proportional hazards methods were used to identify the predictors of MACE, cardiac death, MI, and TLR at follow-up, among patients with successful vs. failed PCI.
The multivariable model was built by stepwise variable selection with entry and exit criteria set at the p≤0.1 level. The following patient level candidate predictors were evaluated: age (per year increment), gender, hypercholesterolaemia, hypertension, diabetes mellitus, smoking, pre-procedural LVEF, prior MI, prior CABG, multivessel disease, femoral access, coronary dissection, cardiac tamponade, CTO location, total CTO length (mm), CTO reference diameter, and total stent length (mm). Interaction terms between successful recanalisation and the following variables were also calculated by means of Cox proportional hazards models: diabetes, age greater than 65 years, prior MI, prior CABG, hypertension, pre-procedural LVEF lower than 40% and multivessel disease.
Statistical analyses were performed using SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
Between 2004 and 2012, recanalisation of a total of 1,517 CTO lesions was attempted in 1,331 consecutive patients. Figure 1 shows the study flow chart of the patient population. The data of 11 patients were excluded due to the presence of cardiogenic shock at initial presentation. Therefore, the study population comprised 1,320 patients, of whom 1,177 had a single CTO, whereas 143 were treated for >1 CTO; 39 patients were referred to our centre after a first failed attempt in another centre. Overall procedural success, including repeat attempts, was achieved in 990/1,320 patients (75.0%) and was 72.7% in the period 2004-2008 and 77.9% between 2009 and 2012 (p=0.03).
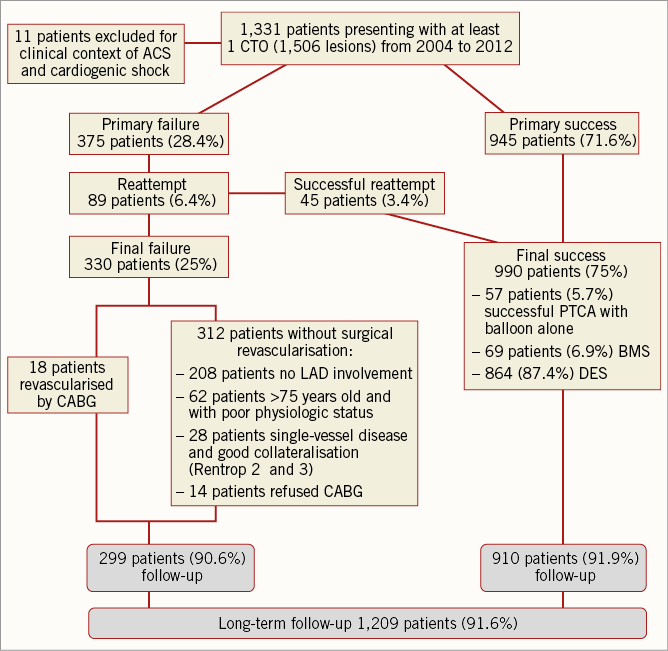
Figure 1. Study design.
RECANALISATION SUCCESS/FAILURE
Cardiovascular risk factors were well balanced between patients who were successfully treated for CTO and those who were not (Table 1). However, compared to patients with unsuccessful recanalisation, patients with a reopened CTO had more favourable baseline clinical characteristics including a less frequent history of previous MI, previous PCI and previous CABG. They also had a higher frequency of left anterior descending (LAD) artery CTO, shorter occlusion lengths, single-vessel disease and a lower J-CTO score (p<0.001). PCI was performed via the radial approach in 62.4% of patients, employing a double coronary injection in 33.5%. With respect to patients with a reopened CTO, stenting was performed in 933/990 (94.2%), using DES in 864/933 (92.6%) and bare metal stents (BMS) in 69/933 (7.4%), reflecting contemporary practice. A total of 24/33 patients with final CTO-PCI failure underwent myocardial revascularisation by CABG.
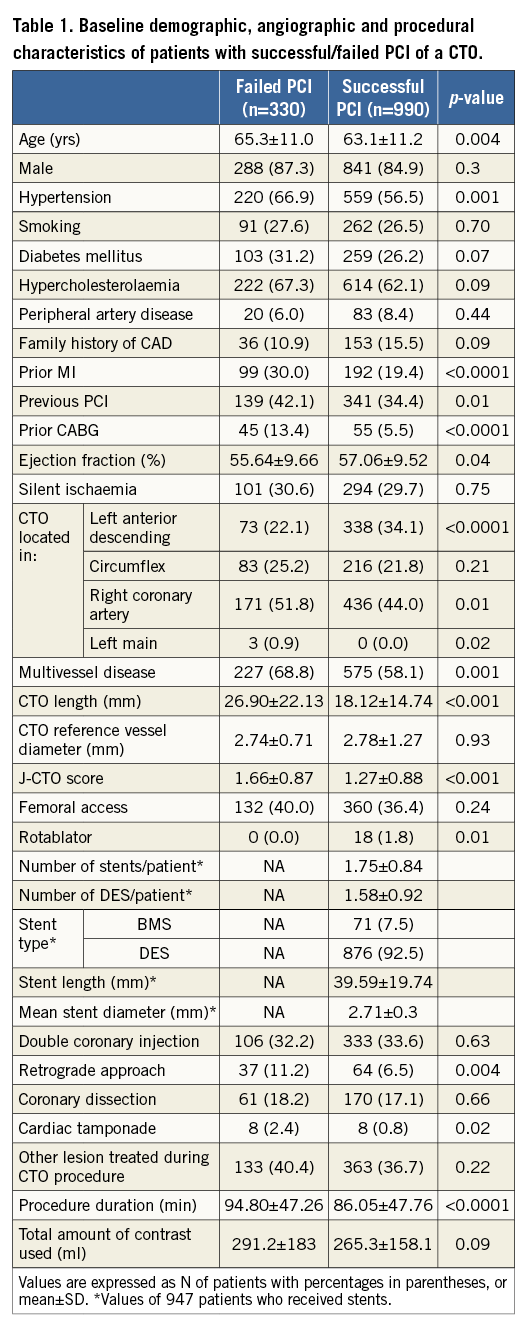
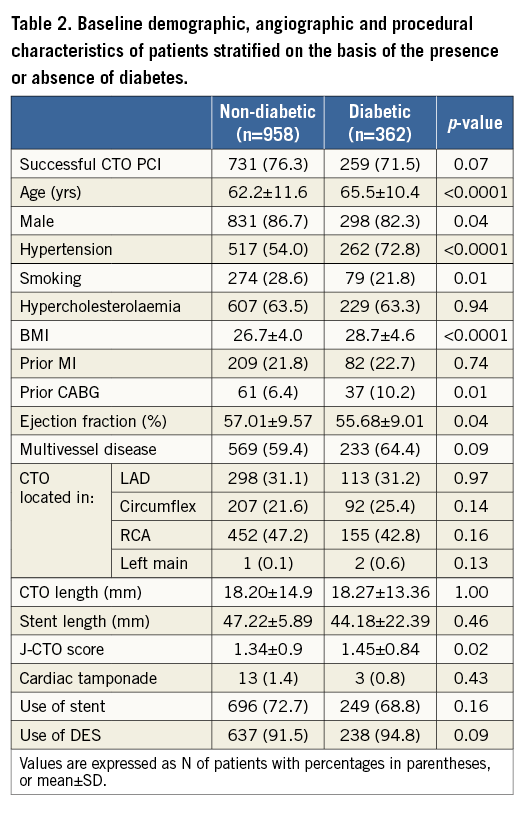
Table 2 shows demographic, angiographic and procedural characteristics of patients stratified on the basis of the presence or absence of diabetes. Compared to non-diabetic patients, diabetics were older and had higher rates of hypertension and previous CABG, as well as lower left ventricular ejection fraction (LVEF). The majority of angiographic and procedural characteristics did not differ between diabetic and non-diabetic patients, except for a higher J-CTO score amongst diabetic patients (p=0.02) who showed a tendency towards a reduced PCI success rate (p=0.07).
LONG-TERM FOLLOW-UP
Long-term follow-up was achieved in 1,209/1,320 patients (91.6%) at a median (IQR) of 4.2 (2.5-6.6) years.
Clinical outcomes in patients with a reopened CTO and in those with failed PCI are presented in Kaplan-Meier curves depicted in Figure 2. Patients with a reopened CTO had lower cardiac mortality rates (13.2% vs. 17.2%, respectively, p<0.0001). The long-term incidence of MI and TLR was not different after CTO recanalisation. Higher MACE in cases of unsuccessful recanalisation (27.5% vs. 33.7% in those with failed CTO recanalisation, p=0.02) was principally driven by cardiac mortality.
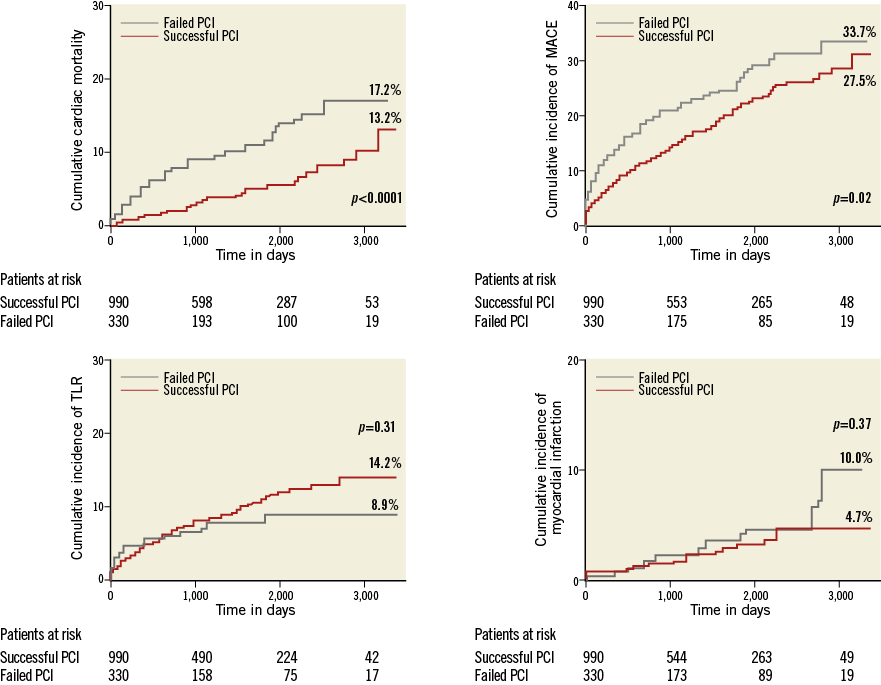
Figure 2. Clinical event rates in patients who underwent successful/failed PCI of a CTO. Unadjusted Kaplan-Maier rates plotted.
Analysis of the Kaplan-Meier curves revealed a clear difference in PCI outcomes according to the presence or absence of diabetes in the study population (Figure 3).
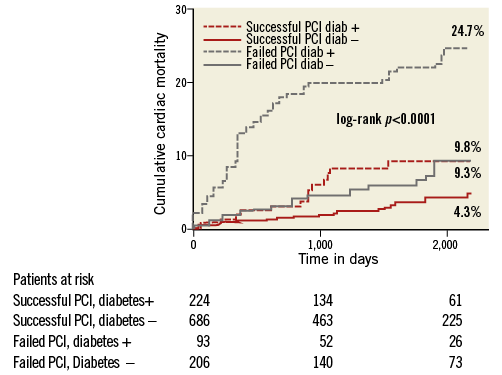
Figure 3. Interaction between diabetes and revascularisation of a CTO. Unadjusted Kaplan-Meier rates plotted.
In instances of PCI failure, diabetics had a higher rate of cardiac death at follow-up (31.1% vs. 13.1% in patients successfully treated, p<0.0001), compared to non-diabetics (Table 3), in whom, interestingly, cardiac mortality was not significantly different between successful and failed angioplasty (23.1% vs. 22.2%, p=0.08).
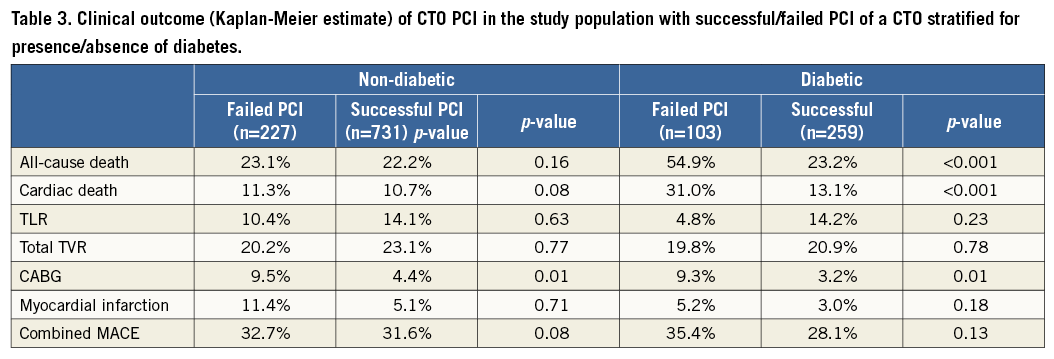
Figure 4 describes the interaction between successful recanalisation and all other relevant covariates. The interaction term HR was 0.48 (95% CI: 0.19-1.21; p=0.12) for diabetes, which estimates the difference in hazard ratios between diabetics and non-diabetics (HR 0.30, 95% CI: 0.15-0.60 for diabetics vs. HR 0.82, 95% CI: 0.41-1.62 for non-diabetics).
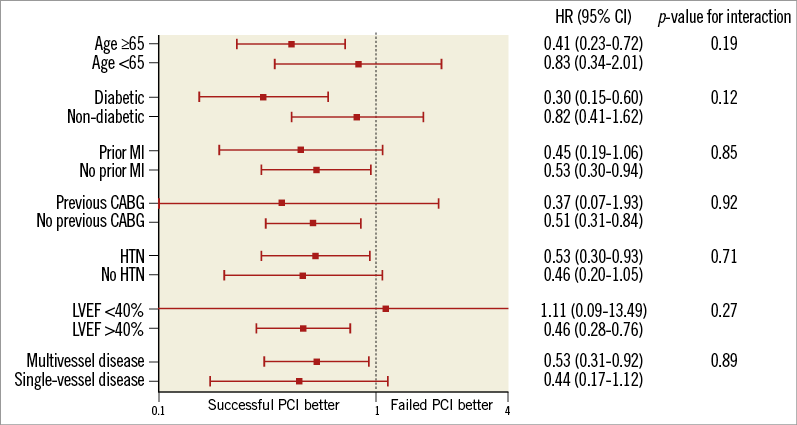
Figure 4. Interaction between successful recanalisation and other relevant covariates.
PREDICTORS OF LONG-TERM SURVIVAL
By multivariate analysis (Figure 5), successful PCI of a CTO (HR 0.51, 95% CI: 0.32-0.81, p=0.005) was a predictor of decreased cardiac mortality. Conversely, presence of diabetes (HR 2.44, 95% CI: 1.52-3.83), increased age (per year increment, HR 1.06, 95% CI: 1.03-1.08) and decreased left ventricular ejection fraction (per percent decrease, HR 1.03, 95% CI: 1.01-1.06) predicted higher cardiac mortality rates.
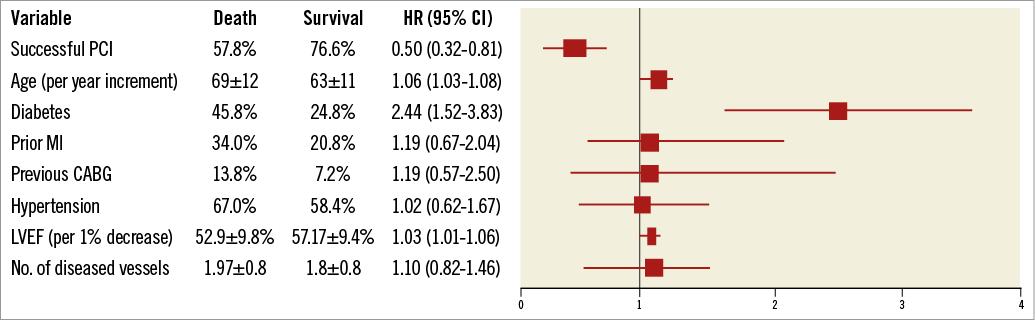
Figure 5. Multivariate analysis. Independent predictors of cardiac death.
Discussion
The main findings of this observational CTO cohort analysis are the following: 1) successful PCI of a CTO is associated with reduced long-term cardiac mortality, 2) independent predictors of cardiac mortality are presence of diabetes, older age and decreased LVEF, 3) the benefits of successful CTO recanalisation are particularly manifest in diabetic patients.
Prior small-cohort studies have shown no differences in long-term survival after recanalisation of a CTO16,17. Valenti et al reported a two-year survival benefit in patients with successful recanalisation of a CTO in a series of 486 patients5. They speculated that improved clinical outcome resulted from complete revascularisation of high-risk patients with documented myocardial viability subtended by the CTO. More recently, the Multinational Chronic Total Occlusion Registry3 and a single-centre registry4 showed improved survival benefit after successful CTO PCI at longer follow-up. As suggested by Jones et al4 and consistent with our study, all-cause mortality was significantly higher after failed reopening in trials with up to four-year follow-up. The present cohort is the largest CTO series derived from a high-volume centre reported to date, with the longest follow-up in a contemporary setting. It is important to underline that available data3,12 were relatively old (1998 to 2007) and could not, therefore, reflect the benefit of recent technical improvements, new-generation DES, microcatheters, and newly developed tapered or stiff wires that have considerably modified the strategy and success rate of CTO reopening. Indeed, our data confirm and further emphasise the fact that opening a CTO is associated with better long-term outcomes in terms of survival.
The mechanism of improved survival associated with opening a CTO has not yet been elucidated. The quantity of viable myocardium subtended by a CTO artery may be an underlying factor and can have an impact on LVEF. Depressed LVEF is in fact known to be associated with increased risk of cardiac death18-20, while CTO revascularisation has been shown to improve left ventricular function21-23. As demonstrated in these previous studies, in this registry decreased LVEF proved to be an independent predictor of cardiac death, whereas prior MI did not. This could be a consequence of the myocardial revascularisation of a CTO corresponding to an infarcted area with preserved viability.
The present study shows different outcomes after successful recanalisation of a CTO in diabetic and non-diabetic patients. Safley et al24 reported a non-significant improvement in survival rates among diabetics with CTO in whom PCI success was achieved compared to those with failed PCI. Although Liu et al25 reported increased MACE rates among diabetic patients compared to non-diabetics after PCI of a CTO, Sohrabi et al26 showed higher in-hospital adverse events in diabetics without any difference in the long-term outcome. In the present study, consistent with the higher all-cause mortality incidence observed in the Multinational CTO Registry12, CTO reopening was associated with decreased cardiac mortality rates among diabetic patients, compared to patients in whom PCI was unsuccessful (31.0% vs. 13.1%, respectively).
Furthermore, these results are consistent with a recent study27 which showed that, in diabetic patients with CTO, an incomplete revascularisation and high residual platelet reactivity after a clopidogrel loading dose are independently related to increased cardiac mortality, suggesting one potential physiopathological explanation supporting our clinical results.
The difference observed in the survival curve between diabetics and non-diabetics was maximal at five years’ follow-up (Figure 3) and decreased up to nine years’ follow-up given the increasing age of the population.
Despite the known limitations of interpreting interaction terms, e.g., low power even with moderately sized samples, and although the interaction term p-value is not significant, our results could be indicative of a very poor outcome in diabetic patients after failed CTO reopening, especially if reproduced in a larger study sample.
Because diabetes is becoming the leading cause of cardiovascular mortality worldwide, the findings of this and future studies in this high-risk subset of patients may be particularly meaningful and furthermore may support the clinical need for appropriately attempting CTO revascularisation, either with PCI, or with CABG in cases of failure.
Finally, the increased need for CABG observed in the failed CTO group (HR 4.06, 95% CI: 1.95-8.43, p<0.001) is consistent with the findings reported in previous publications3,4. This was perhaps to be expected because patients with failed percutaneous revascularisation are more likely to be referred for surgical revascularisation than to be treated medically, especially if CTO involves the LAD.
It is important to point out that in our series patients undergoing CABG after PCI failure, even when revascularised, were included in the failed revascularisation group. Though a potential study limitation, this is, however, negligible in view of the low incidence of cardiac death observed in this subgroup (only two patients revascularised by CABG, and only one patient non-revascularised by CABG experienced cardiac death).
Limitations
Study limitations are inherent in the non-randomised design of this real-life single-centre registry, as it does not provide a comparison of results with those of a medically treated arm. Data were prospectively collected over a long enrolment period in parallel with significant changes in technique and dedicated materials; moreover, no data safety monitoring board or clinical events committee was set up. Additionally, whether diabetic patients required insulin (or not) is not reported, and detailed information on post-procedural medical therapy was not available in all patients. Although we used multivariate Cox regression analysis including a large number of covariates to adjust for differences in baseline characteristics, it is possible that we did not include potentially unknown confounding variables in the multivariate model.
Conclusions
In this large cohort of patients treated for CTO, successful recanalisation was a predictor of improved long-term survival at very long-term follow-up (up to nine years). Presence of diabetes and decreased left ventricular ejection fraction were predictors of higher cardiac mortality rates. Successful recanalisation seems to play a particularly meaningful role in the outcomes of diabetic patients, suggesting that strong efforts to reopen CTO could be beneficial in these patients. Further studies are warranted to confirm the importance of the findings reported here.
| Impact on daily practice Percutaneous coronary intervention for CTO is currently one of the most debated topics in cardiology. Diabetes mellitus is pandemic with more than 171 million affected individuals worldwide, with numbers projected to increase over the next few years. Pending the results of randomised trials, we would like to share with our colleagues the results of this large prospective CTO cohort, which shed some light on the impact of CTO revascularisation focusing, in particular, on diabetic patients. We believe that repeated attempts at achieving CTO revascularisation are likely to improve survival outcomes. We would, therefore, encourage our colleagues to take these findings into consideration when planning procedure strategies, and when discussing treatment options with the patient and the Heart Team. |
Acknowledgements
The authors would like to thank Catherine Dupic and Andrew Roy, MD, for their help in proofreading the manuscript.
Conflict of interest statement
The authors have no conflicts of interest to declare.