Abstract
Aims: The aim of this study was to compare the long-term clinical outcomes of patients with chronic total occlusion (CTO) treated with percutaneous coronary intervention (PCI) versus medical therapy (MT) according to the presence of diabetes mellitus.
Methods and results: A total of 845 patients without diabetes and 702 patients with diabetes were included from the Samsung Medical Center CTO registry. The inverse probability of treatment weighting (IPTW) method was used to adjust for confounding factors. The primary outcome was cardiac death. Median follow-up duration was 46 (interquartile range: 23-71) months. Among the non-diabetes group, patients in the MT group had a higher rate of cardiac death (adjusted hazard ratio [HR] 2.54, 95% confidence interval [CI]: 1.19-5.42, p=0.02) compared to those in the PCI group. For patients with diabetes, there was no significant difference between the two groups in the rate of cardiac death (adjusted HR 1.09, 95% CI: 0.62-1.90, p=0.77). There was a significant interaction between diabetes and cardiac death (interaction p=0.03). After using IPTW methods, a similar result was observed (interaction p<0.001).
Conclusions: For the treatment of CTO, PCI may reduce the risk of cardiac mortality in non-diabetic patients but not in diabetic patients.
Abbreviations
CABG: coronary artery bypass graft surgery
CAD: coronary artery disease
CTO: chronic total occlusion
CVA: cerebrovascular accident(s)
DES: drug-eluting stent(s)
IPTW: inverse probability of treatment weighting
MACE: major adverse cardiac event(s)
MI: myocardial infarction
MT: medical therapy
PCI: percutaneous coronary intervention
Introduction
Approximately 18 to 25% of non-coronary artery bypass graft surgery (CABG) patients with suspected coronary artery disease (CAD) were observed to have chronic total occlusion (CTO)1,2. Patients with CTO underwent percutaneous coronary intervention (PCI) less frequently than those without CTO because of procedural complexities and a lack of evidence regarding the benefits from CTO revascularisation2,3. Several studies have demonstrated that patients with CTO who underwent successful PCI have a reduced risk of adverse clinical outcomes compared to those with failed PCI4,5. Diabetes mellitus is regarded as a coronary heart disease risk equivalent, and it is an important factor when determining treatment strategies for coronary artery disease3,6. Approximately 34 to 40% of CTO patients in the registry were observed to have diabetes mellitus, which may indicate that diabetes is a risk factor for CTO1,7,8. However, limited data were available regarding the association between long-term clinical outcomes and optimal treatment strategy in CTO patients with or without diabetes mellitus. Therefore, we investigated the long-term clinical outcomes of coronary CTO patients treated with PCI versus medical therapy (MT) according to the presence of diabetes mellitus.
Methods
STUDY POPULATION
This was a single-centre observational study. Between March 2003 and January 2012, 2,024 consecutive CTO patients were recruited from the cardiovascular catheterisation databases of Samsung Medical Center, Seoul, Republic of Korea. A CTO lesion was defined as a complete vessel occlusion with Thrombolysis In Myocardial Infarction (TIMI) 0 flow within the occluded segment and estimated occlusion duration of ≥3 months9. Baseline characteristics, angiographic and procedural data, and outcome data were prospectively obtained by trained study coordinators. Additional information was collected from medical records and telephone interviews if necessary. The Institutional Review Board of Samsung Medical Center waived the requirement for informed consent from individual patients given the retrospective nature of this study. Inclusion criteria for this study were: 1) consecutive patients 18 years of age or older; 2) at least one CTO detected on diagnostic coronary angiography; and 3) symptomatic angina and/or positive functional ischaemia test. Exclusion criteria were: 1) history of previous CABG; 2) history of cardiogenic shock or cardiopulmonary resuscitation; and 3) ST-segment elevation acute myocardial infarction (MI) during the preceding 48 hours. After excluding patients treated with CABG among registered patients, 845 patients without diabetes and 702 patients with diabetes were enrolled in the final analysis.
TREATMENT STRATEGY
MT included antiplatelet medication, β-blocker, renin-angiotensin system blockade, nitrates, calcium channel blocker, and aggressive lipid-lowering therapy. The medication regimens of all patients were considered optimal, with doses as allowed by heart rate, blood pressure, and symptoms in the absence of justifiable relative contraindications. CTO revascularisation was performed by CABG or PCI with a drug-eluting stent (DES). Each revascularisation strategy was decided as a treatment option based on patient and physician preference. PCI was performed using contemporary techniques such as bilateral injections, a specialised stiff hydrophilic wire with a tapered tip, microcatheters, and a retrograde approach when possible. The treatment strategy, techniques for approach, type of wire, duration of clopidogrel use, and use of glycoprotein IIb/IIIa receptor inhibitors or intravascular ultrasound were all carried out according to the operator’s discretion.
DEFINITIONS AND OUTCOMES
Diabetes mellitus was defined as a fasting glucose level >126 mg/dl or glycated haemoglobin A1c concentration greater than 6.5% assessed at least once, or the current use of oral hypoglycaemic agents or insulin. All-cause death was defined as any post-procedure death during follow-up, and the cause was considered cardiac unless a definite non-cardiac cause was established10. MI was defined as recurrent symptoms with new electrocardiographic changes compatible with MI or cardiac marker level at least twice the upper limit of normal11. Any revascularisation was defined as revascularisation of either the target or non-target vessels with PCI or CABG. Successful PCI was defined as final residual stenosis less than 20% of the vessel diameter, with TIMI grade ≥2 after stent implantation, as assessed by visual estimation on angiography. The primary outcome was cardiac death during follow-up. Secondary outcomes included myocardial infarction, any revascularisation, and major adverse cardiac events (MACE) consisting of cardiac death, MI, or any revascularisation.
STATISTICAL ANALYSIS
Continuous variables were compared using the t-test. Categorical data were tested using the chi-squared test or Fisher’s exact test, as appropriate. Survival curves were constructed using the Kaplan-Meier method. In multivariable models, covariates that were either statistically significant on univariate analysis or clinically relevant were considered candidate variables. Adjusted hazard ratios were compared by Cox regression based on age, history of PCI, history of MI, multivessel disease, left ventricular ejection fraction, SYNTAX score, left anterior descending artery involvement, and presence of acute coronary syndrome. The inverse probability of treatment weighting (IPTW) method was performed using generalised boosted models for the multiple treatment, and weights were based on the presence of diabetes and treatment strategy (PCI vs. MT) to evaluate interactions between diabetes and treatment strategy that affect clinical outcomes. Statistical analyses were performed using R Statistical Software, version 3.1.3 (R Foundation for Statistical Computing, Vienna, Austria) with p<0.05 considered statistically significant.
Results
BASELINE AND ANGIOGRAPHIC CHARACTERISTICS
OVERALL POPULATION
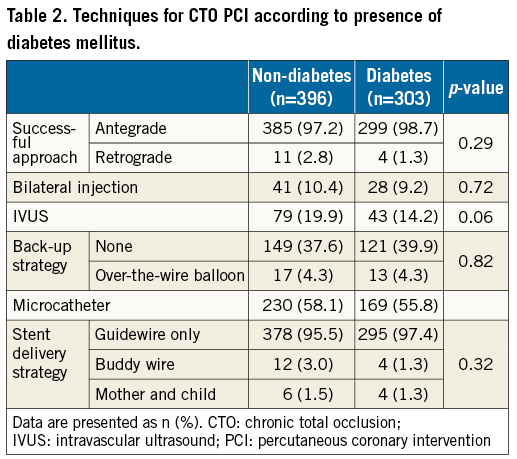
A total of 1,547 CTO patients treated with MT or PCI were enrolled from the registry, including 845 patients without diabetes and 702 patients with diabetes (Table 1). Of these patients, 883 (57.1%) underwent PCI, including 499 (59.1%) in the non-diabetes group and 384 (54.7%) in the diabetes group. There was no significant difference between diabetes and non-diabetes in the procedure time (48.7±37.0 vs. 47.9±34.5 mins, p=0.77) or attempted techniques such as approach of the CTO lesion, bilateral injection, use of support catheter, IVUS, and stent delivery method for CTO PCI (Table 2). In addition, PCI was more frequently attempted in the proximal to mid locations of CTO lesions in both the non-diabetes and diabetes groups (Table 1). Compared with the non-diabetes group, the diabetes group was significantly older and had a higher frequency of chronic kidney disease, hypertension, previous cerebrovascular accident (CVA), multivessel disease, right coronary artery involvement, and high SYNTAX score. Those in the diabetes group also had a low left ventricular ejection fraction and a lower frequency of bridge collaterals.
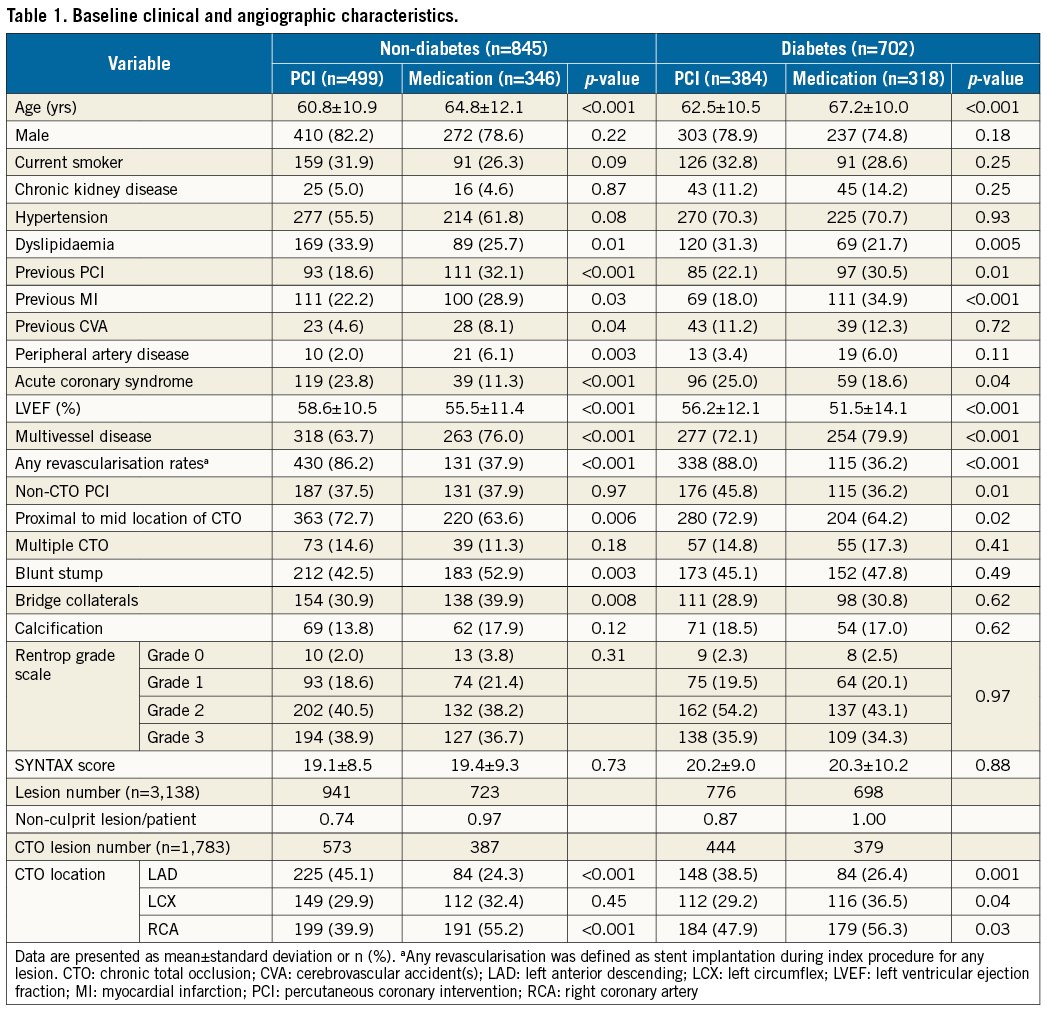
In the non-diabetes group, patients treated by MT alone were more likely to be older. They also had a higher prevalence of previous PCI, previous MI, previous CVA, peripheral artery disease, right coronary artery involvement, multivessel disease, blunt stump, bridge collaterals, and low left ventricular ejection fraction with lower prevalence of dyslipidaemia, acute coronary syndrome, and left anterior descending artery involvement compared with those undergoing PCI. Rentrop grade scale and SYNTAX score were similar for the two groups. In the diabetes group, patients treated by MT alone had a higher prevalence of old age, previous PCI, previous MI, right coronary artery and left circumflex artery involvement, multivessel disease, and low left ventricular ejection fraction. They also had a lower prevalence of dyslipidaemia, acute coronary syndrome, and left anterior descending artery involvement compared with those undergoing PCI. There was a similar prevalence of bridge collaterals, blunt stump, Rentrop grade scale, and SYNTAX score in the two groups.
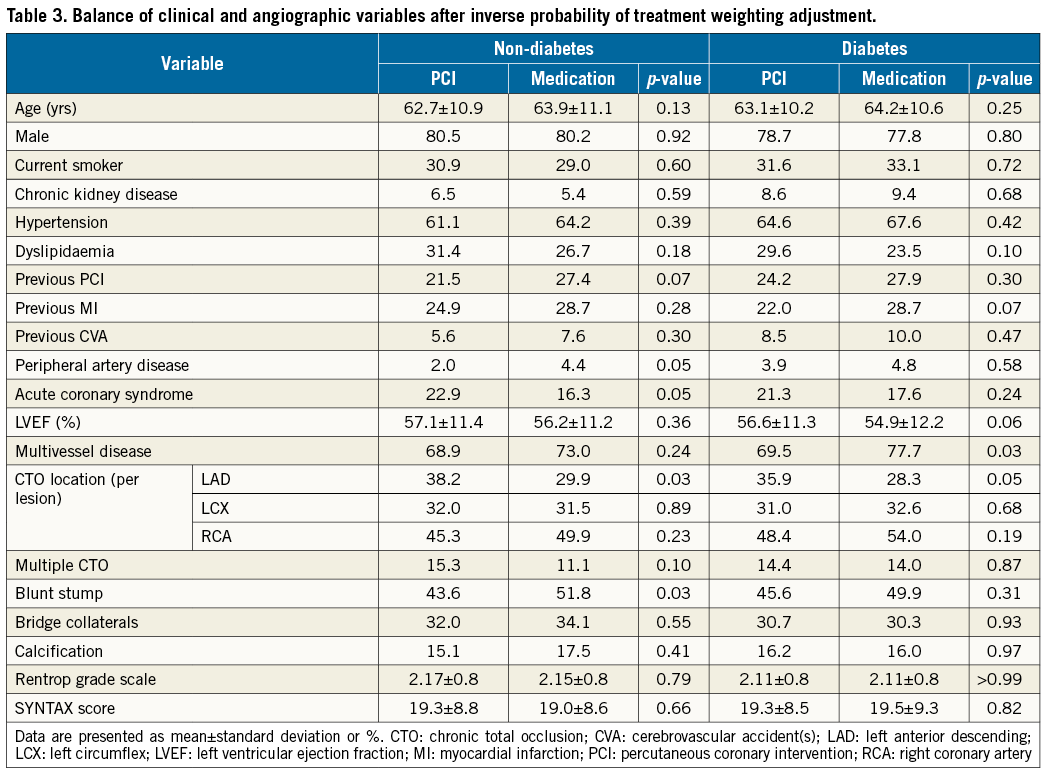
IPTW ADJUSTMENT
The IPTW method was performed to evaluate interactions between diabetes and treatment strategy that affect clinical outcomes. The balances of clinical and angiographic variables after IPTW adjustment are listed in Table 3. After performing IPTW, almost no variables had significant inter-group differences except left anterior descending artery involvement and blunt stump in the non-diabetes group and multivessel disease in the diabetes group.
CLINICAL OUTCOME
OVERALL POPULATION
Follow-up data were available for 1,517 patients (98.6%) with median follow-up duration being 46 (interquartile range: 23-71) months. In the non-diabetes group, patients with MT had a higher rate of cardiac death (MT group versus PCI group, 8.1% vs. 2.2%, adjusted HR 2.54, 95% CI: 1.19-5.42, p=0.007) and MACE (22.0% vs. 12.8%, adjusted HR 1.52, 95% CI: 1.05-2.19, p=0.03) (Table 4). In the diabetes group, there was no significant difference between the rate of cardiac death in the two groups (MT group versus PCI group, 11.9% vs. 6.8%, adjusted HR 1.09, 95% CI: 0.62-1.90, p=0.77). Among diabetic patients, MACE displayed the only significant difference between the two groups (29.6% vs. 20.1%, adjusted HR 1.43, 95% CI: 1.03-1.99, p=0.03) (Table 4). There was a significant interaction between diabetes and cardiac death (interaction p=0.03), but not with MACE (interaction p=0.70).
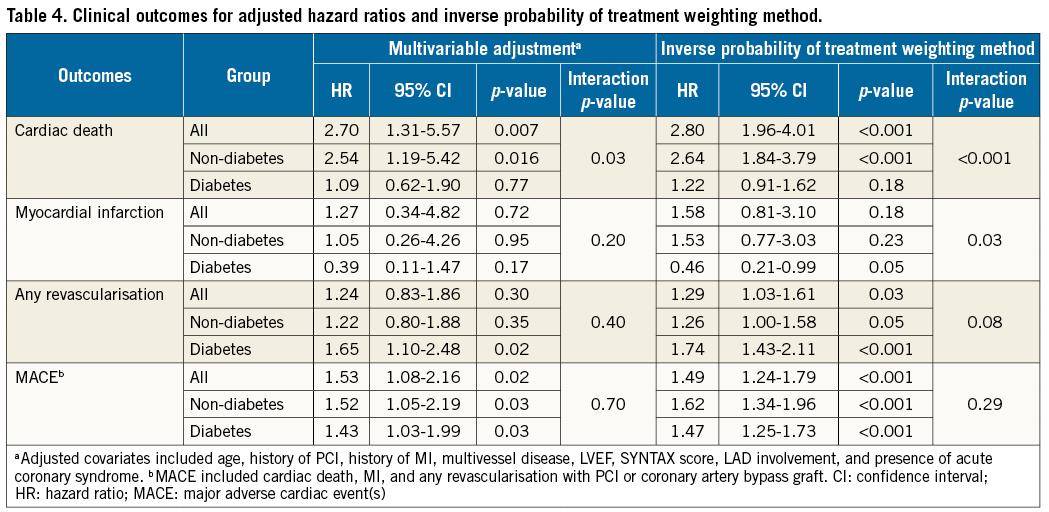
IPTW ADJUSTMENT
After performing the IPTW method within the non-diabetes group, cardiac death was still higher in the MT group compared with the PCI group (HR 2.64, 95% CI: 1.84-3.79, p<0.001) (Table 4, Figure 1A). Within the diabetes group, the incidence of cardiac death was similar between the two groups (HR 1.22, 95% CI: 0.91-1.62, p=0.18) (Table 4, Figure 1B). The interaction p-value for cardiac death and diabetes was significant (p<0.001). In the diabetes group, myocardial infarction was significantly higher in the PCI group compared to the MT group.
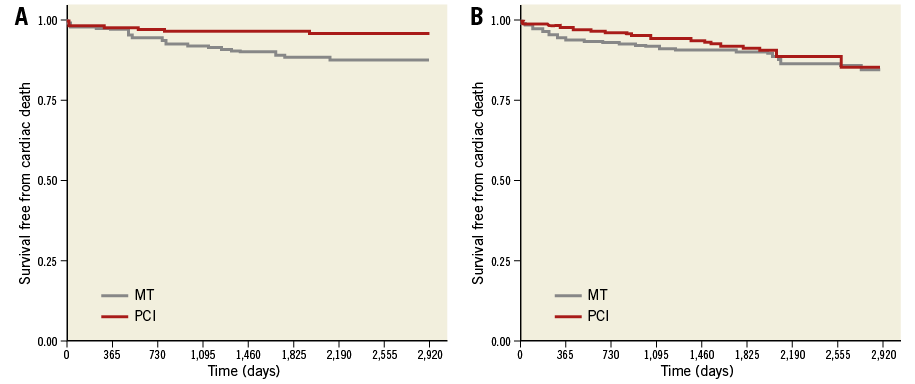
Figure 1. Kaplan-Meier curves, IPTW adjusted to clinical variables for cardiac death among the CTO patients without diabetes (A) and those with diabetes (B) in the PCI group versus the MT group. CTO: chronic total occlusion; IPTW: inverse probability of treatment weighting; MT: medical therapy; PCI: percutaneous coronary intervention
SUCCESSFUL VS. FAILED PCI
Additional analysis was performed to evaluate the clinical outcomes between successful PCI and failed PCI. There was no significant difference between the non-diabetes and diabetes groups in the success rates of PCI (non-diabetes vs. diabetes, 79.4% vs. 78.9%, p=0.87). The successful PCI group had a significantly lower cardiac mortality than the failed PCI group (Figure 2).
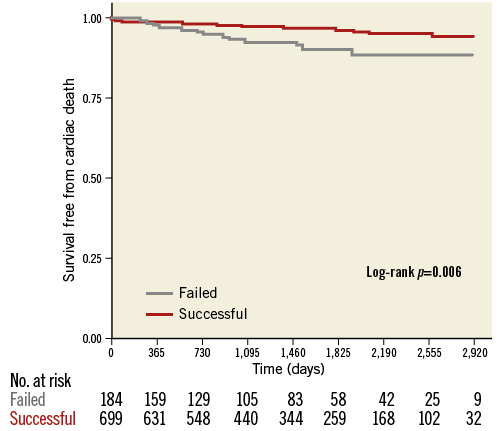
Figure 2. Kaplan-Meier curves for cardiac death among the CTO patients undergoing PCI according to successful or failed PCI. CTO: chronic total occlusion; PCI: percutaneous coronary intervention
CLINICAL OUTCOMES OF CTO LESIONS ACCORDING TO LESION LOCATION
We performed an additional per-lesion-based analysis for evaluation of clinical outcomes according to CTO target lesion location. There were no significant differences in interaction between different CTO target vessels in both diabetes and non-diabetes lesions (Figure 3).
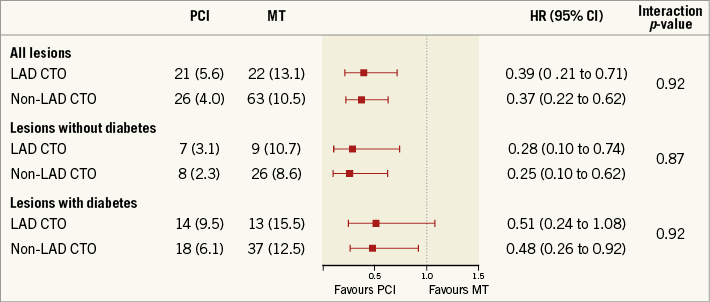
Figure 3. Subgroup analysis according to lesion location. CI: confidence interval; CTO: chronic total occlusion; HR: hazard ratio; LAD: left anterior descending; MT: medical therapy; PCI: percutaneous coronary intervention
Discussion
In this study, the association between long-term clinical outcomes and PCI vs. MT was investigated in CTO patients according to the presence of diabetes mellitus using a single-centre registry. There are several main findings of our study. 1) Among CTO patients, treatment with PCI was associated with lower rates of cardiac death compared to MT alone among non-diabetes patients, but not in patients with diabetes. There was significant interaction between diabetes and cardiac death. In particular, the association of PCI treatment with a lower incidence of cardiac death in non-diabetic CTO patients was maintained after IPTW adjustment. 2) Regardless of the presence of diabetes mellitus among CTO patients, MACE was significantly higher in the MT group compared with the PCI group.
Endothelial cell dysfunction, structural changes in microcirculation, development of collateral arteries, prothrombotic states, proinflammatory states, and poor clinical prognosis are well-established features of patients with diabetes mellitus12-14. Diabetic status is an important consideration when deciding upon the optimal treatment strategy for patients with complex lesions such as CTO because diabetes is associated with an increased risk of adverse clinical outcomes in populations treated with DES15. In the randomised Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial, rates of survival and freedom from MACE did not differ significantly between the PCI group and the MT group among patients with type 2 diabetes and stable ischaemic heart disease16. In accordance with previous studies, among CTO patients with diabetes, the rate of cardiac death did not differ significantly between the PCI group and the MT group. Conversely, our study showed that the incidence of MACE was significantly higher in the MT group compared to the PCI group. In the BARI 2D trial, 34.7% of patients received a DES and 56.0% received a bare metal stent. The other 9.3% did not receive a stent. However, 100% of the PCI group in our study population received a DES. After the introduction of DES, restenosis rates decreased dramatically17. In diabetic patients, DES are associated with reduced mortality, myocardial infarction, and revascularisation rates compared with bare metal stents18. Therefore, the authors speculate that the declining repeat revascularisation rate resulting from popular usage of DES may reduce the incidence of MACE in the PCI group compared with the BARI 2D trial.
A previous study from our registry showed that a PCI success rate of approximately 80% in real-world practice did not reduce cardiac death compared to MT alone19. However, this study demonstrated the cardiovascular mortality benefit in non-diabetic CTO patients with PCI compared to those with MT. In the randomised COURAGE trial comparing medical therapy with PCI for stable ischaemic heart disease, no overall outcome benefit has been demonstrated in non-diabetic patients from subgroup analysis20. However, it is difficult to compare the COURAGE trial and our study because DES were only used in 3% of randomly assigned patients in the COURAGE trial. It is also difficult to explain the reason for the discrepancy between our study and other previous studies. Our study group previously showed the long-term survival benefit of revascularisation compared with medical therapy in patients with CTO and well-developed collateral circulation. In fact, the non-diabetic group of that study had a slightly higher incidence of well-developed collateral vessels21. Our data also show that non-diabetic patients have a significantly lower incidence of multivessel disease and SYNTAX score compared with diabetic patients. The authors speculate that the efficacy of PCI is greater in non-diabetic patients than in diabetic patients because of comparatively fewer non-culprit vessel lesions. Also, one of the potential explanations for the mortality difference with CTO PCI is unmeasured confounders. Higher-risk patients were less likely to undergo CTO PCI. This is very similar to DES studies showing mortality benefit in observational studies but not in RCTs20,22. Accordingly, our results support the idea that diabetes might be an important factor to consider when determining treatment strategies for CTO patients. Randomised controlled trials are needed to confirm the findings of the present study: two trials are ongoing (ClinicalTrials.gov numbers NCT01760083 and NCT01078051).
Limitations
This study has several limitations. First, this study is limited by its observational nature, which may have affected results through confounding factors. In addition, the selection of treatment strategies was based on physician preference. Although IPTW adjustments were performed for potential confounding factors, we were not able to correct for unmeasured variables. Second, this study is also limited by including patients from only a single centre. Third, due to the limitations of our database, we did not have functional ischaemia testing to identify the amount of viable myocardium of study patients. Despite these limitations, this study included long-term follow-up data collection and strict control to adjust for confounding factors using IPTW methods.
Conclusions
For treatment of CTO, PCI may reduce the risk of cardiac mortality in non-diabetic patients but not in diabetic patients. PCI might be actively considered as the treatment option for the treatment of CTO in low-risk patients such as those without diabetes.
| Impact on daily practice We demonstrated that patients with MT had a higher rate of cardiac death compared to those with PCI among non-diabetic patients with CTO. Conversely, among diabetic patients with CTO, there was no significant difference in the rate of cardiac death between PCI and MT. PCI might be actively considered as the treatment option for the treatment of CTO in low-risk patients such as those without diabetes. |
Conflict of interest statement
The authors have no conflicts of interest to declare.