Abstract
Aims: The relation between socio-economic status (SES) and outcomes after percutaneous coronary intervention (PCI) has not been established. We sought to determine whether or not socio-economic status impacts on prognosis after PCI.
Methods and results: This was an observational cohort study of 13,770 consecutive patients who underwent PCI at a single centre between 2005 and 2011. Patient socio-economic status was defined by the English Index of Multiple Deprivation (IMD) score, according to residential postcode. Patients were analysed by quintile of IMD score (Q1, least deprived; Q5, most deprived). Median follow-up was 3.7 (IQR: 2.0-5.1) years and the primary outcome was all-cause mortality. Patients in Q5 (most deprived) were younger, more commonly South Asian, and had higher rates of smoking, diabetes mellitus, renal impairment, previous MI, and previous PCI than patients in Q1. Rates of long-term mortality increased progressively across the five quintiles of IMD score in a linear fashion (p=0.0004), as did rates of recurrent MI, target vessel revascularisation, and CABG. The difference in mortality rates persisted after adjustment for other potential confounding factors after multivariate analysis (Q5 vs. Q1: HR 1.93, 95% CI: 1.38-2.69).
Conclusions: In this large contemporary cohort of patients receiving PCI, socio-economic status was associated with prognosis in a linear fashion.
Introduction
Social deprivation is associated with an increased incidence of cardiovascular disease1-3. Furthermore, survival is reduced following myocardial infarction (MI)4 in patients from deprived social backgrounds, and studies of patients undergoing coronary artery bypass graft surgery (CABG) have shown higher rates of postoperative mortality and major non-fatal complications in the least affluent patients5,6. Low socio-economic status has been associated with lower rates of percutaneous coronary intervention (PCI)7,8, longer waits for the procedure, and less improvement in quality of life following PCI compared with less deprived patients9,10. However, the impact of socio-economic status on outcomes after PCI is less well defined10.
Understanding the relationship between socio-economic status and clinical outcomes in patients with cardiovascular disease is vital if healthcare inequalities are to be addressed. We sought to determine whether socio-economic status influenced long-term all-cause mortality after PCI in a large cohort of patients treated at a single tertiary cardiac centre in East London, which serves a population with a mixed social background.
Methods
This was an observational cohort study of consecutive patients who underwent PCI at a single, high-volume cardiac centre in East London between January 2005 and July 2011.
During the study period, 14,940 patients underwent PCI. Of these, 13,770 (92.1%) had complete data sets and NHS numbers, which allowed mortality status to be tracked, and were included in the analysis. Excluded patients had similar proportions in each socio-economic group to the study population (data not shown).
Socio-economic status
The socio-economic status of each patient was assessed from their residential postal code using the 2010 version of the English Index of Multiple Deprivation (IMD) score11. Details of this are found in the Appendix.
Data collection
Data were entered prospectively into an electronic database at the time of the PCI procedure. These included patient characteristics, procedural details and procedural complications. A retrospective data quality audit of 200 randomly selected medical records established that 95.8% of data fields, including complications, were entered correctly into the database. The primary outcome was all-cause mortality assessed at a median follow-up of 3.7 (IQR: 2.0-5.1) years. Procedural complications and major adverse cardiac events (MACE) were recorded prospectively. MACE were defined as death, MI and repeat target vessel revascularisation. MACE were adjudicated by three independent physicians who were not involved in the procedure and were unaware of the patient’s SES. All-cause mortality status was recorded as of the 10th August 2011 and obtained from the British Cardiovascular Intervention Society (BCIS) national database, part of the National Institute of Cardiovascular Outcomes Research (NICOR). This national database is periodically linked to the UK Office of National Statistics and provides the life/death status of treated patients.
Statistical analysis
Patients were analysed by quintile of English IMD score11. Clinical characteristics of patients were compared using Pearson’s chi-square test for categorical variables and ANOVA for continuous variables. Normality of distribution was assessed using the Shapiro-Wilk test. Kaplan-Meier product limits were used to estimate the cumulative probability of reaching an endpoint and the log-rank test was used to assess survival differences between quintiles. Cox regression analysis was used to estimate hazard ratios (HRs) with 95% confidence intervals (CIs) for the effect of socio-economic status on clinical outcomes in age-adjusted and multiply-adjusted models, which incorporated covariates which showed significant (p<0.05) univariate association with the outcome. The proportional hazards assumption was evaluated by examining log (-log) survival curves and tested with Schoenfeld’s residuals. The proportional hazards assumption was satisfied for all outcomes evaluated. A propensity score analysis was performed using a non-parsimonious logistic regression model comparing patients ranked by IMD score. Multiple variables were incorporated in the model, including all variables with significant interactions. To avoid overadjustment, the multivariable Cox regression analysis was performed using only the two variables “propensity score” and “SES”. SPSS for Mac version 19.0 (IBM Corp., Armonk, NY, USA) was used for all analyses.
Results
BASELINE PATIENT CHARACTERISTICS
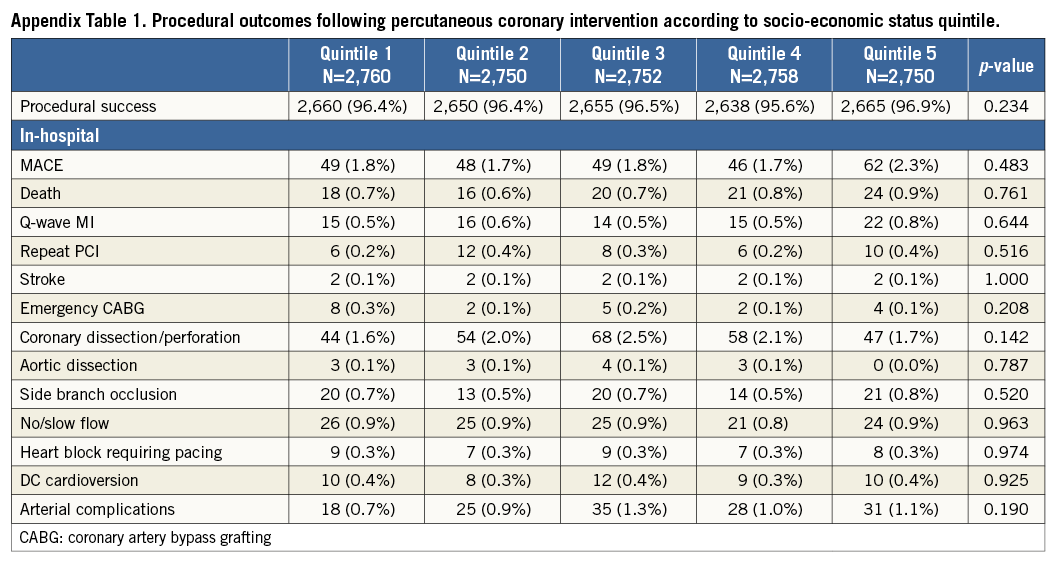
Of the 13,770 patients, the majority were male (74.0%) and Caucasian (71.7%) with a mean age of 63.8±12.0 years. The median IMD score was 24.4 (range 13.4 to 38.4). Patients in Q5 (most deprived) were significantly younger than the least deprived patients and were more commonly of Asian descent. Q5 patients also had higher rates of diabetes mellitus, chronic renal failure (CRF), previous MI, previous PCI, impaired systolic left ventricular function, and multivessel coronary artery disease (Table 1).
PROCEDURAL CHARACTERISTICS
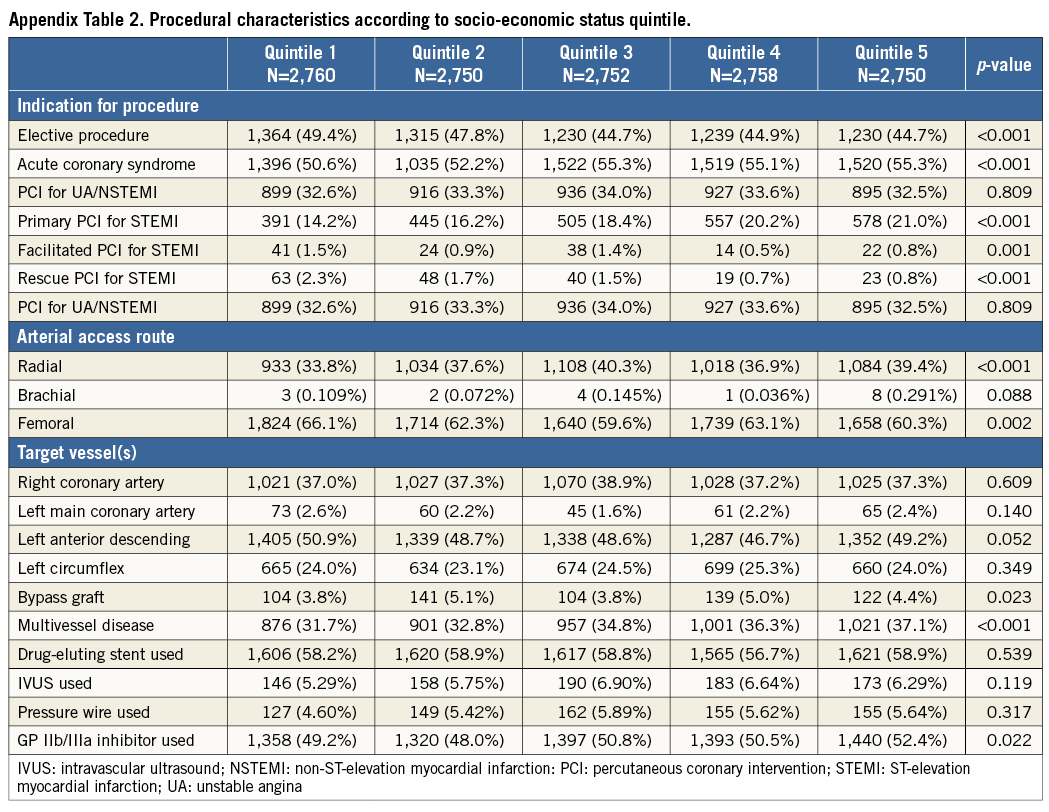
The indication for PCI was more frequently an acute coronary syndrome, particularly STEMI, in patients in Q5 compared with Q1. Patients in Q5 also more commonly underwent radial access for PCI, underwent multivessel PCI, and received a GP IIb/IIIa inhibitor. There were no significant differences in target vessel, or drug-eluting stent use between groups (Appendix Table 1).
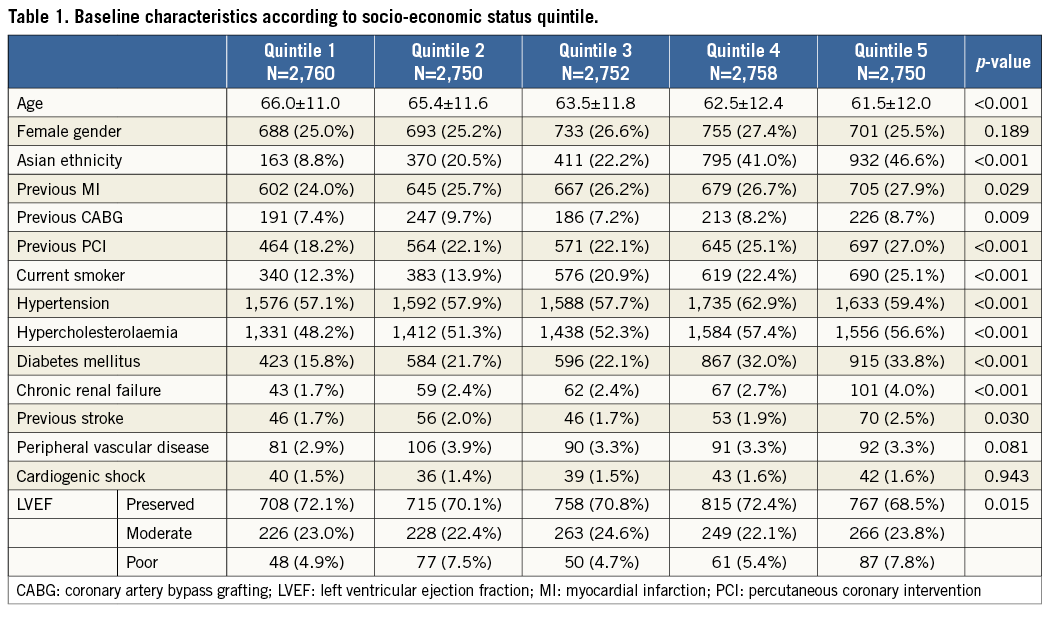
PROCEDURAL OUTCOMES
There were no significant differences in procedural success or complication rates between patients in the different socio-economic groups. Composite in-hospital MACE rates and the rates of its individual components were also similar for patients in each quintile of socio-economic status (Appendix Table 2).
ALL-CAUSE MORTALITY
Kaplan-Meier estimates showed that rates of long-term all-cause mortality increased progressively across quintiles of IMD score, patients in Q5 demonstrating significantly higher long-term mortality rates compared with patients in Q1 (p=0.0004) (Figure 1). Age-adjusted HRs for all-cause mortality were significantly higher in patients in Q5, Q4, and Q3 compared with patients in Q1. The age-adjusted HR for death for Q5 compared with Q1 was 1.65 (95% CI: 1.40-1.94) (Figure 2). After these multiple adjustments for confounding variables, the HR for death increased (compared to the age-adjusted hazard) for Q5 compared to Q1 and was 1.93 (95% CI: 1.38-2.69) (Figure 3). The HRs for death also increased in a stepwise linear fashion for each decreasing quintile of SES. Additionally, SES was associated with long-term mortality after a propensity score was included in the proportional hazard model as a covariate (HR for Q5 compared to Q1: 1.96 [95% CI: 1.40-2.80]).
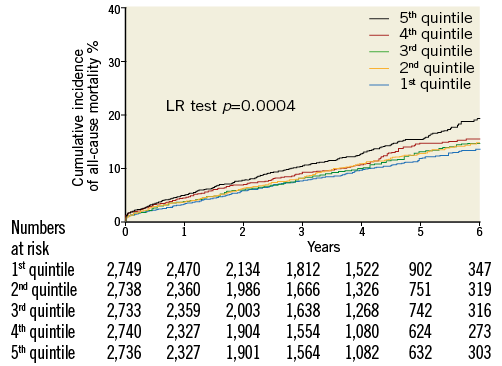
Figure 1. Kaplan-Meier curves showing cumulative probability of all-cause mortality. Kaplan-Meier curves showing cumulative probability of all-cause mortality after PCI according to socio-economic status quintile.
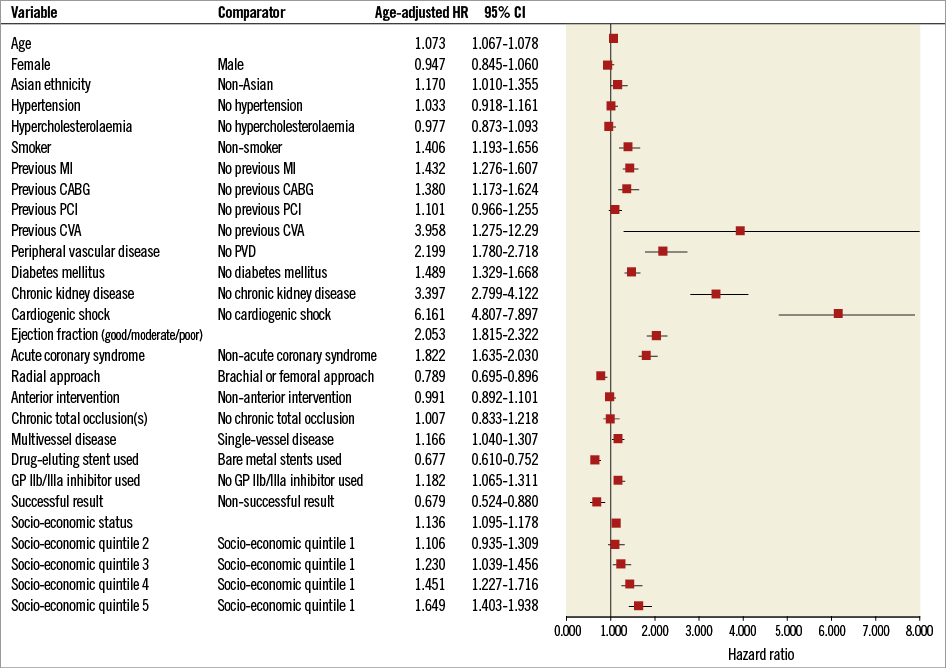
Figure 2. Age-adjusted hazard ratios for all-cause mortality after PCI. Age-adjusted hazard ratios of the Cox analysis for all-cause mortality after PCI with 95% confidence intervals. CABG: coronary artery bypass grafting; CVA: cerebrovascular accident; MI: myocardial infarction; PCI: percutaneous coronary intervention; PVD: peripheral vascular disease
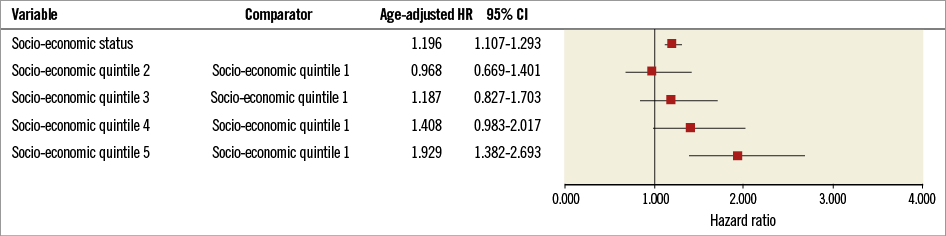
Figure 3. Multivariate hazard ratios for all-cause mortality after PCI. Multivariate hazard ratios of the Cox analysis for all-cause mortality after PCI with 95% confidence intervals.
REPEAT MYOCARDIAL REVASCULARISATION AND MYOCARDIAL INFARCTION
Kaplan-Meier estimates showed that the rates of repeat target vessel revascularisation and MI increased progressively from least to most deprived patients, with a significant difference in rates between Q5 and Q1 (p<0.0001) (Appendix Figure 1). A similar pattern was observed for the rates of CABG during follow-up, with higher rates in patients in Q5 compared to patients in Q1 (6.4% [95% CI: 3.4-11.1] versus 4.5% [95% CI: 2.1-8.9], p=0.02).
Discussion
This is the first study to observe a powerful pernicious association of socio-economic status on outcome after PCI. In this large, contemporary cohort study of 13,770 consecutive patients, all-cause mortality rates 3.7 years after PCI were significantly higher in patients in the lowest quintile for socio-economic status compared with patients in the highest quintile. Our rich data source allowed adjustment for multiple confounding factors known to be associated with outcome after PCI. We also included patients presenting with both acute coronary syndromes and stable angina. As expected, there were significant differences in the baseline characteristics of the patients in the different socio-economic groups. However, the association between all-cause mortality and socio-economic status not only persisted, but the hazard ratios increased after accounting for these differences. The 20% most deprived patients had a dramatically increased adjusted hazard of death which was >90% higher than the 20% least deprived patients. Furthermore, there was a progressive increase in mortality from the lowest to the highest quintile of deprivation, suggesting a possible dose response relationship of increasing hazard of death with deteriorating SES.
This is the largest study which has investigated the effect of socio-economic status on outcomes after PCI and the first displaying a relationship with a significant clinical endpoint of mortality. Previous studies demonstrated that patients who were from a low socio-economic background had more frequent chest pain-related readmissions and a lower quality of life after PCI10. However, they did not detect an effect on mortality10 or report rates of cardiovascular events12. A smaller study with 1,397 patients, who were analysed in groups of low, medium, and high socio-economic status, showed a significantly higher MACE rate in patients in the low socio-economic group compared with the medium and high socio-economic groups during a median follow-up of 650 days13. The higher MACE event rate in this study was mainly driven by higher rates of MI and repeat revascularisation but mortality rates were not significantly different between the groups. Not only did our study find that low socio-economic status was an independent predictor of all-cause mortality following PCI, but we also showed that lower SES was associated with higher rates of repeat PCI, MI, and CABG.
Our catchment area in East London has a population which is diverse in ethnicity and socio-economic status. Three of its local authorities (Hackney, Newham, and Tower Hamlets) are amongst the 10 most deprived in England11,14. However, even within these local authorities there are affluent areas, while different local authorities within the catchment area are far less deprived. Furthermore, >95% of PCI procedures undertaken in patients in East London during the study period were performed at our centre. These factors made our population ideal for the study of the relation between socio-economic status and prognosis after PCI.
In this study, we demonstrated progressively higher rates of comorbidities such as diabetes mellitus, CRF, previous MI and multivessel disease from least deprived to most deprived patient groups. However, correction for these variables did not account for the mortality differences. As the difference in outcome cannot be explained exclusively by the difference in conventional risk factors, it is possible that conventional secondary prevention may not resolve these social inequalities in healthcare.
There are likely to be several possible reasons why socio-economic status might influence PCI outcomes. Although specific diagnostic categories are accounted for in the regression analysis, other unassessed comorbidities may also be more prevalent. Obesity, for example, is associated with low socio-economic status15 and premature death16 but was not included in this analysis. Other risk factors for chronic disease such as sedentary lifestyle, poor diet and heavy alcohol consumption are all more prevalent in patients from low socio-economic groups17. Furthermore, relevant comorbidities may not be limited to physical disease states, but might also include psychological morbidity. Social isolation is seen increasingly in those of low socio-economic status18 and has been associated with poorer outcomes following MI19. Asian ethnic origin was also progressively more common across quintiles of social deprivation. Intuitively, it might be thought that this would contribute to the prognostic disadvantage among patients with low socio-economic status. However, ethnicity has previously been shown not to be associated with all-cause mortality after PCI20.
Two of the domains which contribute to the English IMD score are income and education and training. These variables have a potentially important influence on behaviour, related to outcome in patients with vascular disease. Change leading to risk factor modification, uptake of cardiac rehabilitation, and compliance with medications are likely to be affected by these variables which may affect cardiovascular and non-cardiovascular mortality21-23. Indeed, attendance at cardiac rehabilitation is reduced in patients of a lower socio-economic class24, which may contribute to the elevated mortality of these patients, although data exist to show that, despite correction for cardiac rehabilitation attendance, SES still correlates with functional recovery post MI25. Additionally, some studies have identified reduced rates of prescription of secondary prevention medications in patients with low socio-economic status26, which may also contribute to the elevated mortality.
The explanation for the excess mortality observed in patients from low socio-economic groups in this study is therefore likely to be multifactorial. Irrespective of the cause, the independent association between social deprivation and higher rates of all-cause mortality implies that the solution must be to try to shift the characteristics of subjects in the lowest socio-economic groups towards those in the higher socio-economic groups.
Limitations of this study
Our study is an observational analysis of consecutive patients from a single centre. Our data set included most clinical variables known to affect outcome but, like all observational studies, our results might be confounded by variables that we did not measure, such as adherence to secondary preventative therapies and cardiac rehabilitation. Furthermore, we excluded 8% of patients due to incomplete data sets, which could have introduced a selection bias. Socio-economic status is a variable that is difficult to measure. The English IMD score has several limitations, which are discussed in the Appendix.
Conclusions
This study in a large, contemporary cohort is the first to demonstrate that low socio-economic status is associated with adverse prognosis after PCI using hard endpoints such as mortality. This association persisted after accounting for conventional variables known to influence long-term mortality rates. We have confirmed the pernicious effect of socio-economic status on mortality after PCI, which cannot be explained by conventional risk factors alone. Indeed, we feel that conventional secondary prevention is unlikely to resolve the social inequalities we have described. Other factors are likely to be driving the poor outcome that patients in the low socio-economic groups appear to suffer.
| Impact on daily practice |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Methods
IMD SCORE
This robust index of deprivation divides England into 32,482 small geographical areas, each of which contains about 1,500 residents, and awards them a score for seven domains (income, employment, health and disability, education and training, housing and services, living environment, and crime) according to information obtained from the 2010 national census. The domains were weighted and then combined to provide a single measure of deprivation for each geographical area. IMD scores have been widely used to study relationships between socio-economic factors and health outcomes, such as equity of access to care27, disease presentation28, life expectancy29, and post-surgical mortality30.
The English IMD score has several limitations, which arise from the methodology involved in its derivation. The score incorporates seven domains into an overall quantification of deprivation, which is assigned based on defined geographical area rather than on an individual subject’s characteristics. Individuals who live in one particular area will obviously experience different levels of deprivation31. IMD scores are not a linear measure of deprivation and do not incorporate information on duration of residence. Therefore, we could not assess the contribution of deprivation exposure time to mortality. Nevertheless, the IMD score is the best available means for quantifying deprivation in England32.
DATA COLLECTION
Baseline clinical data collected included age, gender, racial origin, diabetes mellitus, smoking status, hypertension, hypercholesterolaemia, prior MI, PCI, CABG, peripheral vascular disease (PVD), New York Heart Association (NYHA) class, chronic renal failure (CRF; serum creatinine concentration >200 umol/L or requirement for renal replacement therapy), systolic left ventricular (LV) function, cardiogenic shock, and number of diseased coronary vessels. Procedural data recorded included indication for PCI, target vessel(s), use of intravascular ultrasound (IVUS) or pressure wire, stent type (drug-eluting or bare metal), and use of glycoprotein (GP) IIb/IIIa inhibitors. Procedural complications included arterial access-site complications, side branch occlusion, aortic or coronary dissection, MI, emergency CABG, and arrhythmia. MI was defined as new pathologic Q-waves in the distribution of the treated coronary artery with an increase of creatinine kinase-MB to >2 times the reference value or significant elevation in troponin T values. The requirement for repeat target vessel revascularisation during follow-up was identified from the PCI database, and the requirement for subsequent CABG was identified from analysis of the separate surgical database.
ETHICS
The data were collected as part of a national cardiac audit and all patient identifiable fields were removed prior to analysis. The local ethics committee advised us that formal ethical approval was not required.
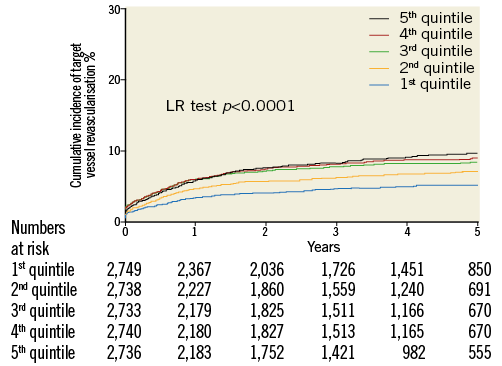
Appendix Figure 1. Kaplan-Meier curves showing cumulative probability of repeat target vessel revascularisation or myocardial infarction. Kaplan-Meier curves showing cumulative probability of repeat target vessel revascularisation or myocardial infarction after PCI according to socio-economic status quintile.