Abstract
Aims: Our aim was to investigate whether there is social inequality in access to invasive examination and treatment, and whether access explains social inequality in case fatality in a nationwide sample of patients admitted for the first time with unstable angina or non-ST-elevation myocardial infarction (NSTEMI) in Denmark.
Methods and results: All patients admitted for the first time with NSTEMI (n=16,625) or unstable angina (n=8,800) from 2001 to 2009 in Denmark were included. We measured time from admission to coronary angiography (CAG), percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG). The outcomes were 30-day and one-year case fatality. We found social inequality in access to CAG and one-year case fatality for both NSTEMI and unstable angina patients, but the time waited for CAG did not explain the social inequality in case fatality.
Conclusions: Despite nominal equal access to health care, social inequality in case fatality after NSTEMI and unstable angina exists in Denmark. The patients with the shortest education waited longer for angiography; however, this did not seem to explain inequality in case fatality. This register-based study was approved by the Danish Data Protection Agency (Approval number 2010-41-5263). Register-based studies do not need approval by a medical ethics committee in Denmark.
Abbreviations
ACS: acute coronary syndrome
AMI: acute myocardial infarction
CABG: coronary artery bypass graft
CAG: coronary angiography
NSTEMI: non-ST-elevation myocardial infarction
PCI: percutaneous coronary intervention
STEMI: ST-elevation myocardial infarction
Introduction
Social inequality in case fatality after diagnosis of ischaemic heart disease (IHD) is a consistent finding 1-3. This inequality has been explained by differences in severity at the time of diagnosis, delay in seeking help4, lifestyle1,5, and differences in treatment1,6. Routine invasive examination within 72 hours is currently recommended for all patients with non-ST-elevation myocardial infarction (NSTEMI) and unstable angina7-10. Studies have shown that patients with a low socioeconomic position (SEP) are less likely to receive the most advanced treatment and the optimal timing of treatment7,11-14. Whether inequality in treatment and timing of treatment actually influence social inequalities in IHD case fatality has scarcely been explored. The few studies available have found that waiting time plays a minor role compared to demographic and clinical factors in explaining social inequality in case fatality11,15,16. However, many of these studies were small, used area-based measures of social position, and none of them included a nationwide cohort of patients. In Denmark, information on SEP can be linked with information on treatment and survival at the individual level for all patients who come into contact with the national healthcare system. The aim of this paper was, therefore, to investigate whether access to invasive examination and treatment explain social inequality in 30-day and one-year case fatality in a nationwide cohort of patients admitted for the first time to a hospital with a diagnosis of NSTEMI or unstable angina from 2001 to 2009 in Denmark.
Methods
This study was based in Denmark, which has a healthcare system financed by public tax. Danish legislation calls for easy and equal access to healthcare17. Invasive examination and treatment of patients with acute coronary syndromes was, from 2001 to 2009, provided by five hospitals designated as invasive centres and eight satellite centres providing only coronary angiography (CAG)18,19.
CASE DEFINITION AND DATA LINKAGE
All patients admitted to hospital with acute coronary syndrome (ACS) from 2001 to 2009 were identified in the Danish National Patient Registry (DNPR) (n=99,473) using the following ICD10 codes: I20.0 unstable angina pectoris, I21.0-I21.3 ST-elevation myocardial infarction (STEMI), I21.4 non-ST-elevation myocardial infarction (NSTEMI) and I21.9 acute myocardial infarction (AMI) - unspecified.
The DNPR contains information on patients admitted to hospital from 1977, and on out-patient and emergency care from 1995 onwards20. Patients with prior ischaemic heart disease (ICD10: I20-I25) registered in the DNPR were excluded using information from six years prior to the index admission for all patients (n=14,094). As recommended by Joensen et al21 we restricted the analysis to patients discharged from hospital wards. We therefore excluded out-patients (n=2,564) and patients with a NSTEMI or unstable angina diagnosis from an emergency room which was not verified on the subsequent admission (n=11,560). We further excluded patients who were born before 1920 (n=8,301) because the information regarding their education is considered invalid. A further 2,870 patients had no information on education. Of the remaining 57,797 patients there were 8,800 unstable angina patients, 14,851 STEMI patients, 16,625 NSTEMI patients and 17,521 patients with unspecified AMI. Patients with STEMI and unspecified AMI were not included in the analysis. Information from the DNPR was linked with data from the Danish Heart Registry, which registers clinical information regarding patients undergoing invasive cardiac procedures, the Medical Cause of Death Registry and central registers containing information on SEP.
SOCIOECONOMIC POSITION (SEP)
SEP was measured as the highest attained education registered in the year prior to diagnosis. The variable was grouped into three categories: higher education (university, medium length education including bachelor’s degrees), medium education (trade/craft education and short education) and low education (obligatory schooling or high school).
TIME TO EXAMINATION OR TREATMENT
Time measured in hours was estimated from admission to initiation of coronary angiography (CAG), and from CAG to percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG). Only treatment and examination within the first 30 days after the initial admission were included in the analysis.
30-DAY AND ONE-YEAR CASE FATALITY
The main outcome 30-day and one-year case fatality was calculated after the initial diagnosis and after examination (CAG) or treatment (PCI or CABG).
COMORBIDITY
To adjust for pre-existing comorbidity we used the Ontario acute myocardial infarction prediction rules22,23. These rules have been found to predict mortality after AMI better than the modified Charlson comorbidity index (i.e., excluding myocardial infarction)24. We used both primary and secondary diagnosis from the DNPR dating from five years prior to the index admission.
SEVERITY OF DISEASE
Left main coronary artery (LMCA) involvement and the number of occluded vessels, which indicate the severity of the disease, were extracted from the Danish Heart Register (DHR). When identifying this information we allowed for ±2 days between the DHR CAG date and the DNPR CAG date. Information on LMCA involvement and the number of occluded vessels was available for 72% of the NSTEMI patients and 76.2% of the unstable angina patients receiving CAG.
STATISTICAL ANALYSIS
In analysis 1 we analysed whether there was social inequality in survival after diagnosis of ACS and analysed the effect of CAG within 30 days on this inequality. This was done by using a Cox proportional hazards model with time since diagnosis as the underlying time and adjustment for age, sex, year of diagnosis and comorbidity. When analysing the effect of CAG within 30 days this was included as a time-varying covariate.
In analysis 2 we analysed social inequality in being invasively examined (CAG) within 30 days, for having a PCI or CABG within 30 days of CAG, and for social inequality in time waited. For the first part we used a Cox model where we censored for death and PCI/CABG respectively. For the second part we plotted cumulative incidence curves for the three educational groups where we censored when patients died or, in the case of CABG or PCI, when the other treatment was chosen, i.e., a competing risk. For PCI and CABG we also plotted the combined incidence curve to see if there was a substitution effect between PCI and CABG which accounted for a potential inequality.
In analysis 3 the focus was on whether time waited could explain differences in social inequality in survival after CAG, PCI or CABG. We used a Cox proportional hazards model and used time since CAG, PCI and CABG as the underlying time. When analysing whether social inequality in survival could be explained by time waited for CAG we estimated case fatality from the time of CAG, thus time waited for CAG was not included. This was done in order to avoid immortal time bias. We included time waited as an explanatory variable along with the number of occluded vessels and LMCA involvement. Results from analysis 2 showed no or only minor inequality in time waited for PCI or CABG treatment. Therefore, we ultimately did not perform analysis 3 on case fatalities subsequent to PCI and CABG.
Analysis 4 focused on whether the total inequality shown in analysis 1 could, alternatively, be explained by differences in survival among the patients who did not have a CAG performed. We used a Cox model where we censored for CAG as a competing risk.
In all analyses we included age as a cubic spline if necessary. Due to potential problems with the validity of an ACS sub-diagnosis (i.e., cases we believe to be NSTEMI or unstable angina cases could in fact be more acute STEMI cases), we validated our results by excluding patients receiving a CAG within 24 hours (more acute cases) and repeated analysis 3.
Results
Table 1 shows that, of the 8,800 unstable angina and 16,625 NSTEMI patients, 30% were not invasively examined, 30.1% received a CAG and no other invasive treatment, 31.6% received a CAG and PCI and 8.9% CAG and CABG. Men accounted for 63.6% of patients, 70.7% were ≥60 years or older, 50.3% of the patients had a low education, 38.7% a medium education and 10.9% a high education. Cardiac dysrhythmias, cerebrovascular disease, cancer and diabetes were the most common pre-existing comorbidities. Crude analysis showed a higher 30-day and one-year case fatality rate for patients not invasively examined or treated, NSTEMI patients, women, older patients and patients with pre-existing comorbidities (except congestive heart failure).
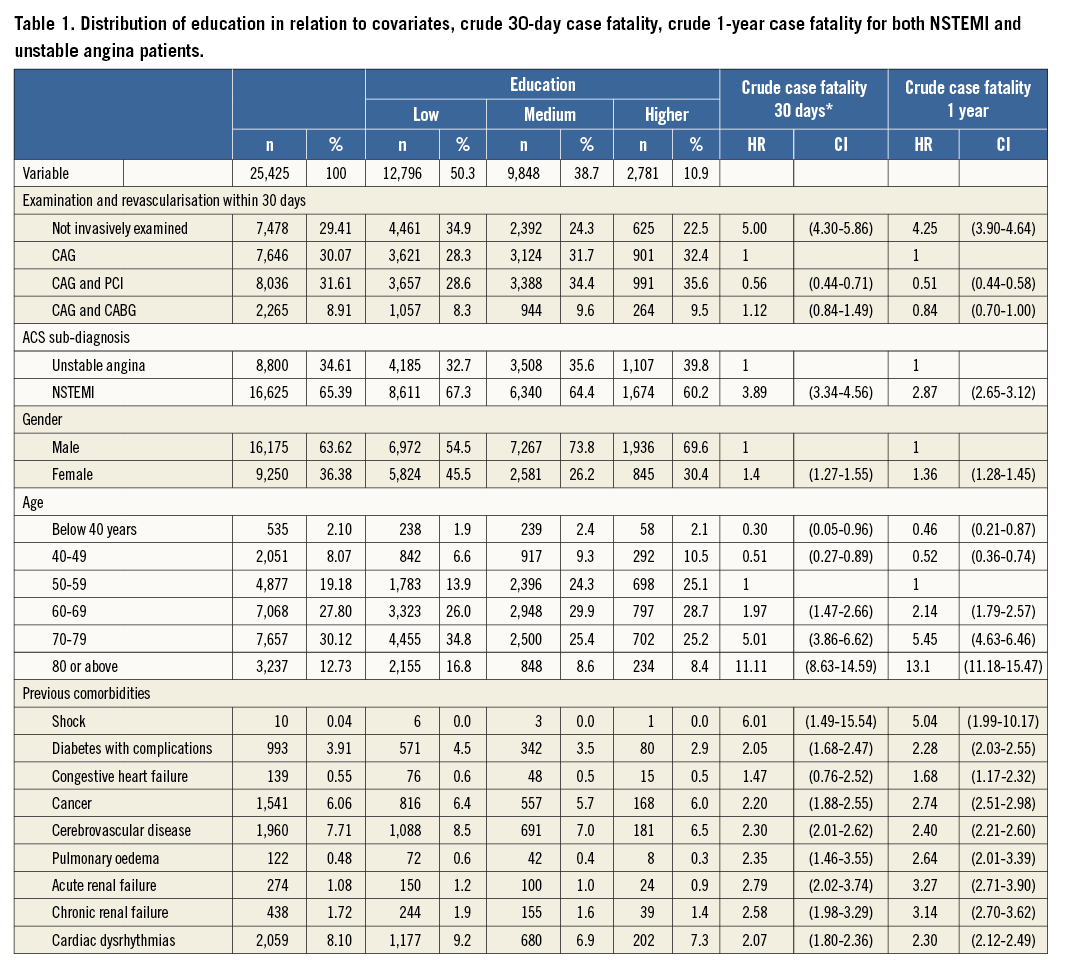
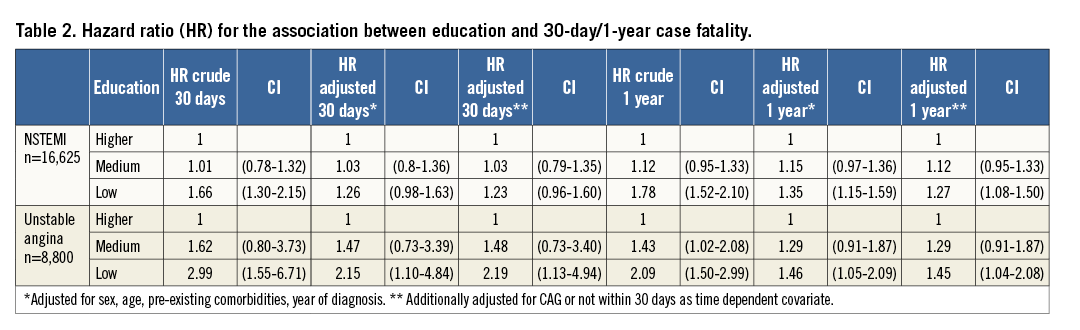
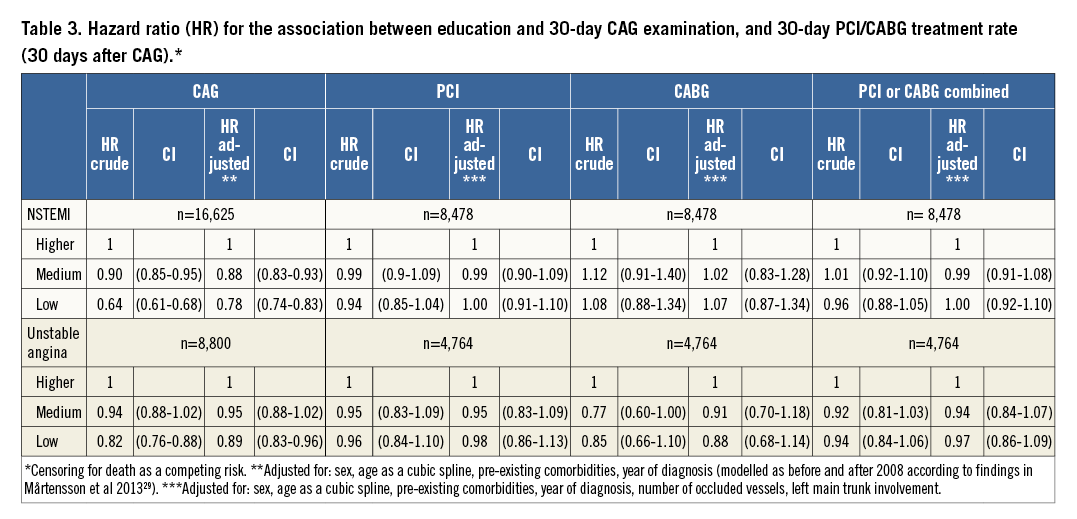
Table 2 presents the results from analysis 1 and shows a clear relationship between education and both 30-day and one-year case fatality, except for NSTEMI and 30-day case fatality where the effect became insignificant after adjustment. When including CAG within 30 days as a time-dependent covariate the effect of education on both 30-day and one-year case fatality was generally only slightly attenuated. Analysis 2 (Table 3) revealed that patients with a lower education were less likely to receive a CAG within 30 days. However, for the patients who did receive a CAG there were no differences in the likelihood of receiving a PCI or CABG within 30 days of the CAG. The cumulative incidence curves (Online Figure 1, Online Figure 2) showed the same result.
In the analyses of case fatality after CAG (analysis 3) (Table 4, Table 5), we found a significantly higher one-year case fatality rate among the lower educated patients compared to the highest educated patients. This inequality was not attenuated when time waited for CAG was included in the models. In general, patients who waited longer for CAG had a lower case fatality. Because of potential validity problems with the ACS sub-diagnosis we excluded patients receiving a CAG within the first day. This did not change the relationship between education and case fatality, except for unstable angina and one-year case fatality where the effect of education became insignificant.
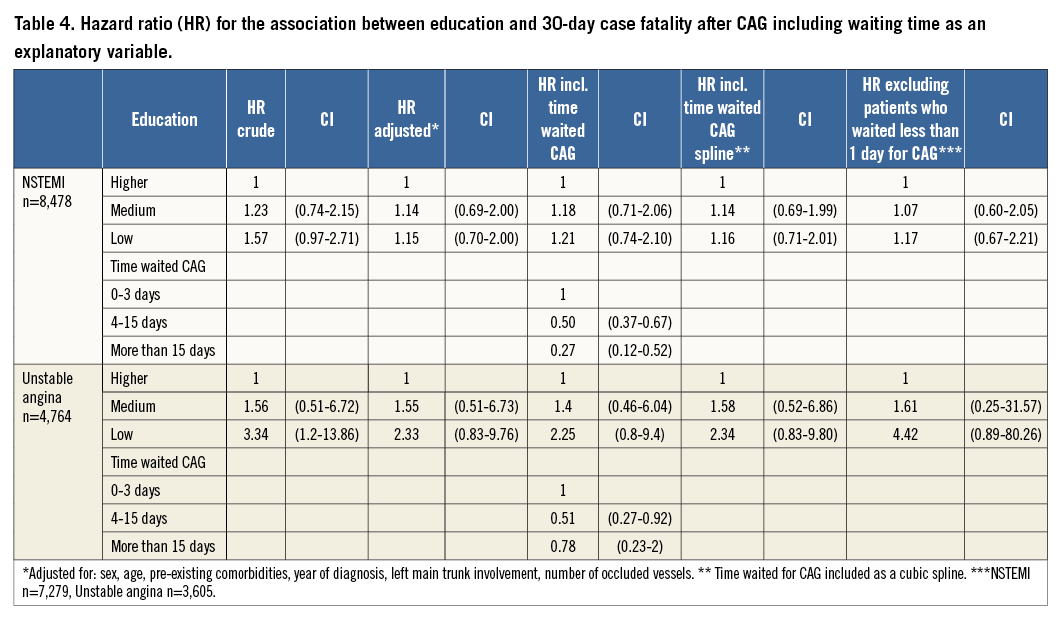
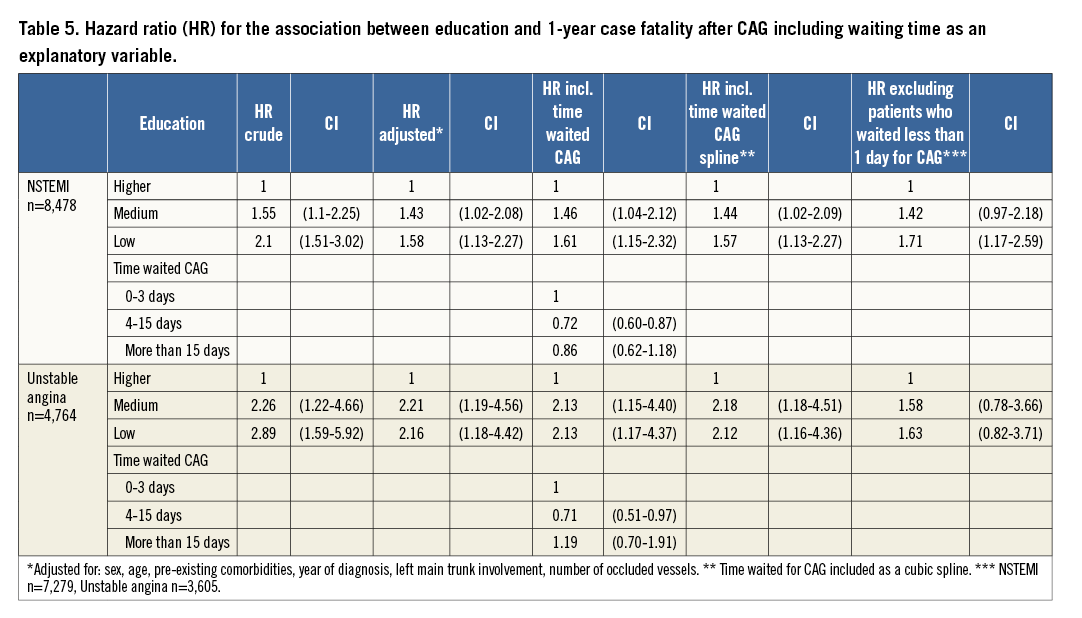
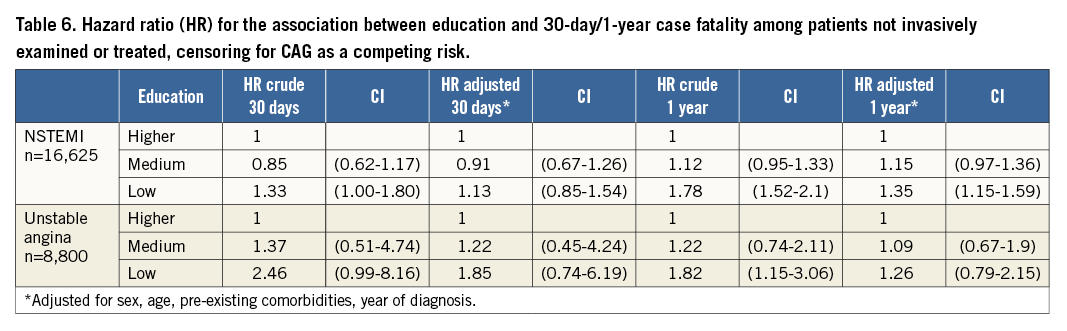
For the patients who were not invasively examined, the lower educated had a higher 30-day and one-year case fatality compared to patients with higher education for both NSTEMI and unstable angina. The effect was only significant for NSTEMI patients and one-year case fatality (analysis 4) (Table 6).
Discussion
We found educational inequality in both 30-day and one-year case fatality for both NSTEMI and unstable angina patients. There was inequality in access to CAG (receiving it or not) and patients with the lowest education also waited longer; however, this did not explain the social inequality in case fatality. NSTEMI patients with a lower education who were not invasively examined had a higher one-year case fatality rate compared to patients with higher education. Overall, our results lead us to believe that the inequality in case fatality is primarily explained by differences in case severity, lifestyle, rehabilitation, adherence to medical treatment or other factors of health and healthcare that we could not observe – a hypothesis that is consistent with the literature11,15,16. Other Danish studies have likewise found that even though there are differences in treatment this does not explain the social inequality in case fatality25,26. However, in a society such as in Denmark, with supposedly equal and easy access to healthcare, it is worrying to find that access to the recommended invasive examination, which is a prerequisite for further invasive treatment, is influenced by the patient’s educational level. Even though this inequality in access does not seem to impact on inequality in case fatality we cannot exclude that there can be other negative effects on the health and wellbeing of the patients with the lowest educational level. Our study gives no explanation as to why individuals with lower levels of education are less likely to receive CAG, but other studies have shown that patients with low SEP wait longer before presenting at the hospital and may therefore have a worse prognosis. Further, they have a larger comorbidity burden which may complicate and prolong the decision process on whether or not to examine the patients invasively2. However, our results indicated that the inequality persisted even after adjusting for comorbidities, suggesting that comorbidity is not the only explanatory factor. The finding of the inverse relationship between time waited for CAG and case fatality could suggest that time waited for CAG can be seen as a proxy for disease severity (and thus, the need for early CAG). We can speculate that the inverse relationship is generated by residual confounding caused by unobservable case mix factors. Our results suggest that more urgent cases with a higher risk of death are correctly given higher priority, and thus early access to invasive examination and treatment. This interpretation is in accordance with the findings of Montalescot et al27 from GRACE (Global Registry of Acute Coronary Events).
STRENGTHS AND LIMITATIONS
One of the main strengths of this study is the large unselected cohort of all patients admitted to hospital in Denmark with a diagnosis of NSTEMI and unstable angina from 2001 to 2009. Further, we had access to high-quality information on education at an individual patient level. We used advanced methods of data analysis and also explored social inequality in fatality among patients who were not invasively examined or treated, as patients who are not followed up may potentially be a major driver of the inequality in case fatality after diagnosis. We had information on the severity of the disease from the CAG described by number of occluded vessels and LMCA involvement. This information was missing for 28% of NSTEMI patients and 24% of unstable angina patients, but this was not related to education. We did not include patients who died before reaching the hospital, which has previously been reported to be a more frequent occurrence in lower SEP groups28: this might have led to an even larger inequality in case fatality. We did not have information on biomarkers or results from echocardiograms, but had to rely on the information registered in the DNPR. However, we restricted our analysis to patients admitted to wards, as recommended by Joensen et al. To validate our results further we excluded patients (in analysis 3) who received a CAG within the first day as these patients may be more acute (and hence not NSTEMI or unstable angina patients). We did not have access to information on medical treatment in the hospital, thus we could not identify whether patients who were not examined and treated invasively received other relevant antithrombotic treatment.
Conclusion
Socioeconomic inequality in case fatality for NSTEMI and unstable angina patients is present for both the patients who were invasively examined and those who were not. There was inequality in access to CAG; however, this did not explain the inequality in case fatality. Future research should explore why the rate of CAG examination differs across socioeconomic groups and whether this impacts negatively on outcomes other than case fatality.
| Impact on daily practice When studying the relationship of social inequalities to fatality in patients with first-time, non-ST-elevation myocardial infarction or unstable angina, the cause does not seem to be related to timing or access to invasive examination or treatment. Consequently, effort to minimise social inequality in case fatality should focus on other socially related factors which have a known impact on survival such as comorbidity, patient delay or lack of adherence to secondary preventive medication. |
Funding
This work was supported by the Danish Heart Association [grant number 10-04-R78-A2806-22609], The Health Insurance Foundation [grant number 2011B037], Fabrikant Ejner Willumsens Mindelegat og Aase og Ejner Danielsens Foundation.
Conflict of interest statement
The authors have no conflicts of interest to declare.
SUPPLEMENTARY DATA
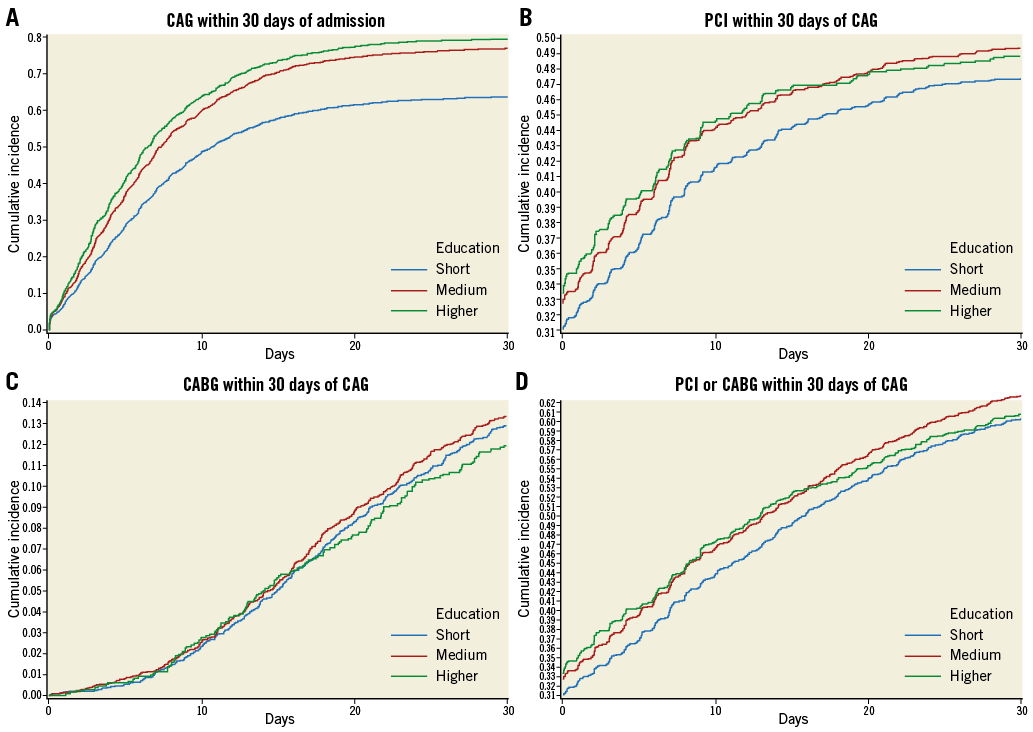
Online Figure 1. NSTEMI: cumulative incidence of CAG, PCI, CABG and PCI/CABG for the three educational groups.
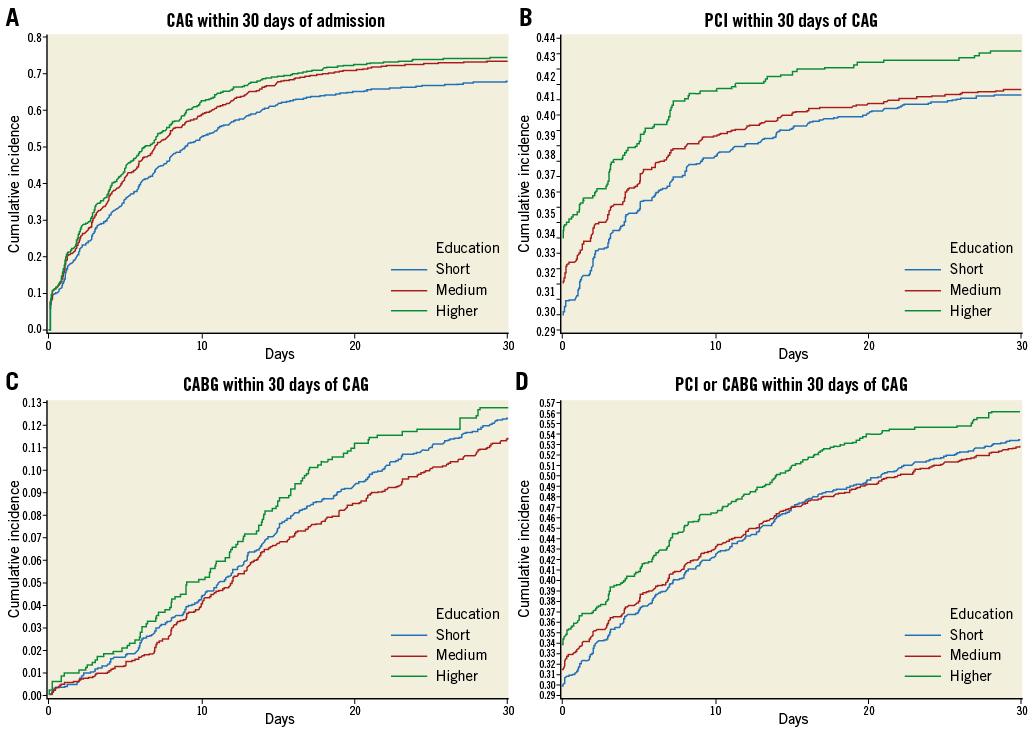
Online Figure 2. Unstable angina: cumulative incidence of CAG, PCI, CABG and PCI/CABG for the three educational groups.