Abstract
Aims: Despite recommendations in recent guidelines for a routine invasive strategy for non-ST-segment elevation acute coronary syndrome (NSTE-ACS), long-term data on the implementation of treatment strategies in clinical practice are not available. Our aim was to provide long-term data on the implementation of a routine invasive strategy in NSTE-ACS in clinical practice.
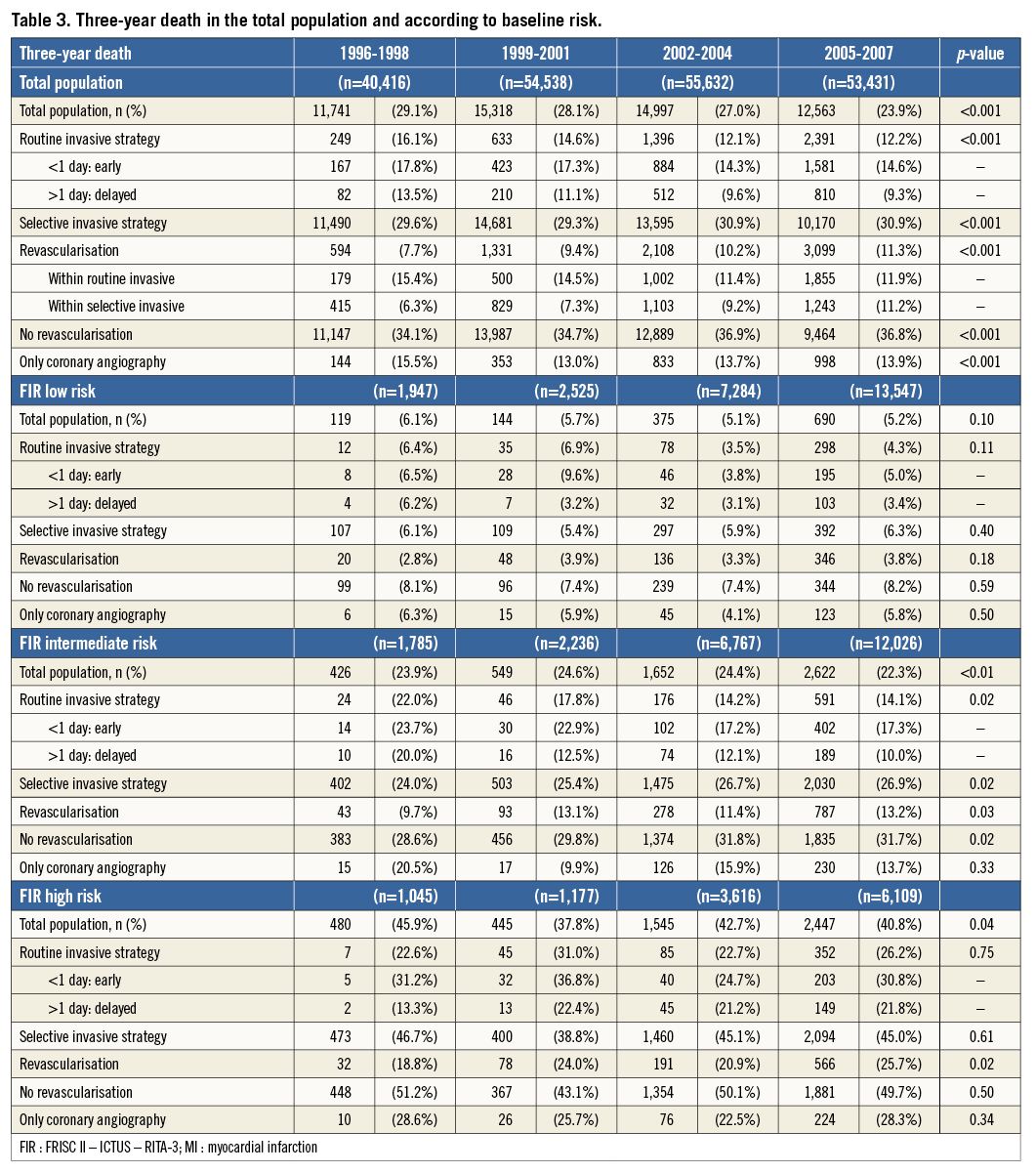
Methods and results: In the SWEDEHEART registry, data from 204,092 consecutive NSTE-ACS patients admitted between 1996 and 2007 were recorded. The use of the routine invasive strategy, retrospectively defined as coronary angiography (and subsequent revascularisation) within three days after admission, increased from 3.8% in the period 1996-1998 to 37.4% in the period 2005-2007. The largest absolute increase in the use of this strategy was observed in low-risk patients, while a similar relative increase was observed in all risk categories. The use of the selective invasive strategy, defined as coronary angiography later than three days after admission or none at all, decreased from 96.2% in the period 1996-1998 to 62.5% in the period 2005-2007. In the total population, there was a gradual decrease in three-year all-cause mortality, from 29.1% in the period 1996-1998 to 23.9% in the period 2005-2007.
Conclusions: There has been an increase in the use of a routine invasive strategy in NSTE-ACS patients over the course of 12 years in Sweden. There was a decrease in three-year mortality over the same time course.
Introduction
Current European Society of Cardiology (ESC) guidelines on myocardial revascularisation recommend a routine invasive strategy over a selective invasive strategy for patients with intermediate to high-risk non-ST-segment elevation acute coronary syndrome (NSTE-ACS)1. This recommendation is partly based on a meta-analysis of the FRISC II, ICTUS and RITA-3 (FIR) trials2, showing a direct relationship between baseline risk and the long-term benefit of the routine invasive strategy by reducing the composite of mortality and myocardial infarction (MI). Regarding baseline risk and treatment strategies, an important treatment-risk paradox exists in the management of ACS3. Patients considered high-risk were less likely to undergo coronary angiography and subsequent revascularisation. However, there were only weak correlations between risk assessment by the treating physicians and those by validated risk scores.
Data on the implementation of these treatment strategies in clinical practice and clinical outcomes over a longer time period are currently not available. In the Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART) registry, consecutive patients with ACS have been “captured” since 19954. The aim of the current analysis was to describe the use of invasive strategies and related three-year outcomes, according to baseline risk, in these NSTE-ACS patients in Sweden over a twelve-year period.
Methods
SOURCE DATA
Data were derived from the SWEDEHEART registry. SWEDEHEART has been enrolling consecutive ACS patients admitted to hospitals in Sweden since 1995, and currently includes all Swedish hospitals providing cardiac care. Information is collected prospectively, and the variables in SWEDEHEART comply with the international Cardiology Audit and Registration Data Standards5. The technical platform was developed by Uppsala Clinical Research Center, Uppsala University. SWEDEHEART is funded by the Swedish public healthcare provider and is independent of commercial funding. The protocol is available at http://www.ucr.uu.se/swedeheart, and the registry has been described previously4.
STUDY POPULATION
For the current analysis, we included all patients with a discharge diagnosis of NSTE-ACS between 1996 and 2007, including non-ST-segment elevation MI (NSTEMI) and unstable angina pectoris (UAP). The standardised criteria used for the diagnosis of NSTEMI and UAP were according to the World Health Organization6. The biochemical criteria for diagnosing MI were in accordance with the ESC/American College of Cardiology consensus documents7,8. All patients were informed about their participation in the registry and the follow-up, and had the right to request to be excluded. The registry, merging of databases and the current analysis were approved by the local ethics committee at Uppsala University, Sweden. Our study complies with the Declaration of Helsinki.
TREATMENT STRATEGIES
SWEDEHEART does not capture the intended treatment strategy by the treating physician; therefore, we used the following definitions based on coronary angiography during initial hospitalisation. The routine invasive strategy group comprises patients who underwent coronary angiography (and subsequent revascularisation if suitable) within three days after admission. The selective invasive strategy group comprises patients who underwent coronary angiography (and subsequent revascularisation if suitable) later than three days after admission or no coronary angiography at all. Coronary angiography after index hospitalisation was not included. The definitions were based on current guidelines. Because the intended treatment strategy was not captured in the SWEDEHEART registry, there is potential crossover from either intended strategy because of clinical signs or symptoms. In-hospital revascularisation was defined as revascularisation by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) before discharge.
OUTCOMES AND FOLLOW-UP
The main outcome for the current analysis was three-year all-cause mortality. Mortality data were obtained by synchronising SWEDEHEART with the National Death Registry, which contains the vital status of all Swedish citizens.
QUALITY OF THE DATA
To ensure the validity of the information entered into the database, a single specially trained monitor visited randomly selected participating hospitals every year and compared information in the patient records with the information entered into the SWEDEHEART database. This involved 30 to 40 randomly chosen patients for each hospital.
STATISTICAL ANALYSIS
The data are presented as cohorts of patients admitted over three-year periods. Categorical data are reported as frequencies (percentage). P-values presented are for linear trend. The allocation to different treatment strategies and outcomes was also presented according to the patients’ baseline risk profiles. Because cardiac biomarker data were not available, we used the integer-based FIR risk score, which was developed for the evaluation of risk and benefit of a routine invasive strategy in the FIR collaboration2. Using this score, a patient’s baseline risk profile was estimated as low (<5), intermediate (5-8) or high (>8). The FIR risk score is defined as follows: age (years): <60=0 points, 60-64=1, 65-69=2, 70-74=3, and ≥75=5; diabetes=4; hypertension=1; previous MI=3; ST-segment depression=2; body mass index: <25 kg/m2=1, 25-<35 kg/m2=0, and ≥35 kg/m2=22. Because age is a major driver of the baseline risk profile of patients, we also present the allocation to different treatment strategies and occurrence of outcomes according to different age categories as a sensitivity analysis.
Three-year cumulative mortality was estimated with the Kaplan-Meier method. Three-year death rates are reported according to the time periods, treatment strategy and baseline risk as estimated with the FIR risk score. Changes over time in the hazard for mortality compared with the oldest time interval were calculated with univariable and multivariable Cox proportional hazards models. The multivariable model included adjustments for FIR risk score and revascularisation within the initial hospitalisation.
Results
PATIENTS AND TREATMENT STRATEGIES
From January 1996 to December 2007, 204,092 patients were hospitalised for NSTE-ACS. The discharge diagnosis was NSTEMI in 90,603 and UAP in 113,489 patients.
Baseline characteristics and treatment strategies are presented in Table 1.
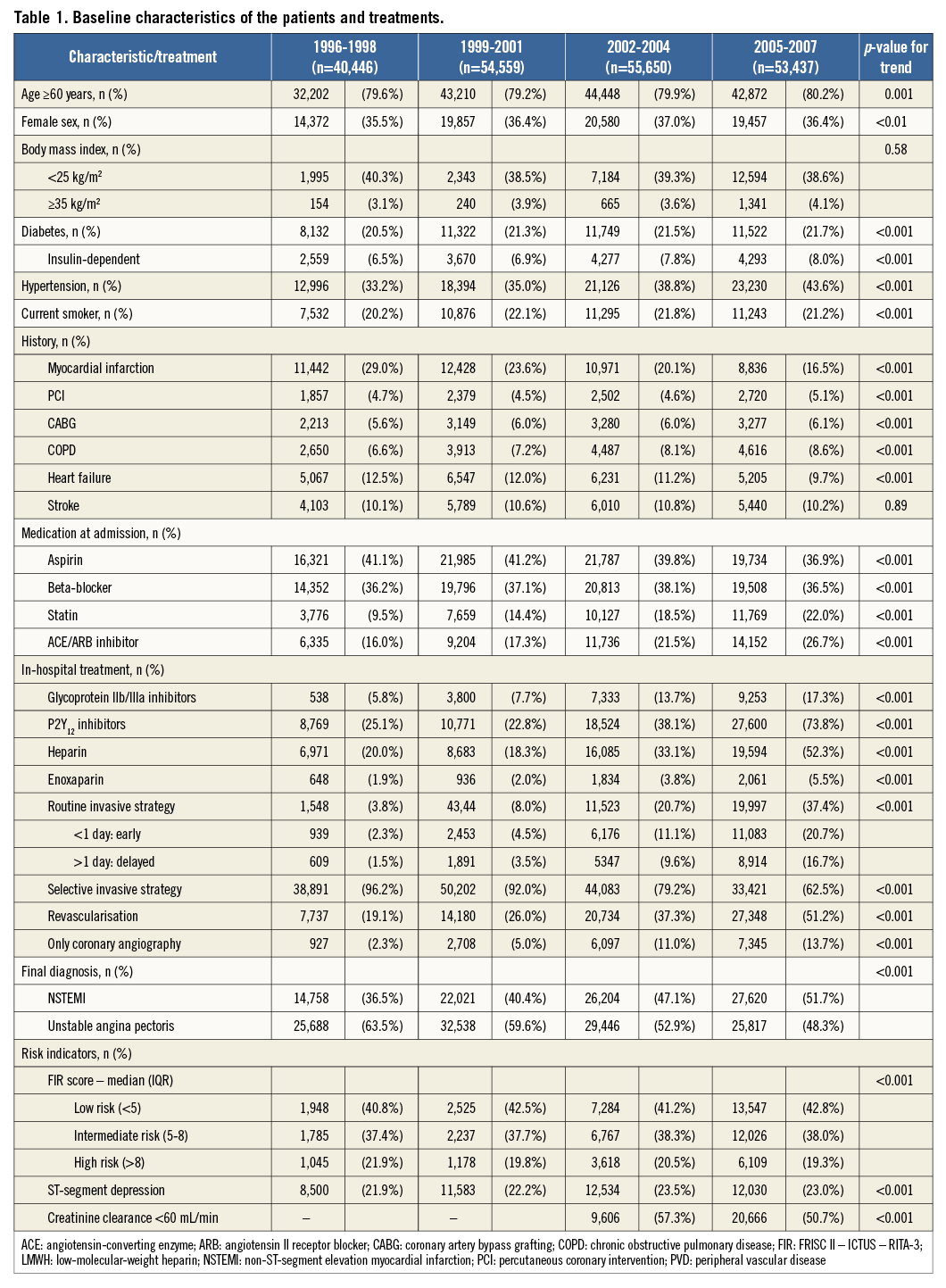
During the course of 12 years, patients became older, had a greater body weight, and more often had diabetes and hypertension. The use of the routine invasive strategy increased gradually over time, resulting in increasing percentages of patients who were revascularised during the initial hospitalisation. In patients aged 70 years or older, the use of a routine invasive strategy rose from 2.5% in the period 1996-1998 to 27.5% in the period 2005-2007 (p<0.001). Comparable trends were observed in octogenarians and nonagenarians.
TREATMENT STRATEGIES ACCORDING TO BASELINE RISK
The largest absolute increase in the use of the routine invasive strategy was observed in patients at low risk for ischaemic events, as indicated by the FIR risk score. In this group, 9.6% of the patients underwent a routine invasive management in the period 1996-1998, compared with 52.8% in the period 2005-2007 (Table 2). The smallest absolute increase was observed in high-risk patients, from 3.0% in the period 1996-1998 up to 22.6% in the period 2005-2007. In patients in whom one or more of the variables that were needed to calculate the FIR risk score were missing, 3.4% received a routine invasive management in the period 1996-1998, 7.1% in the period 1999-2001, 20.2% in the period 2002-2004, and 32.8% in the period 2005-2007. Missing values were observed in 0% of the patients for the risk score component age, 1.8% for diabetes, 2.4% for history of MI, 3.5% for ST-segment depression on admission, 2.9% for hypertension, and 69.6% for BMI. Because we were unable to calculate the FIR risk score mainly because of missing BMI values, we also present the results according to a modified FIR risk score excluding BMI. As shown in Table 2, there was an increase in the use of the routine invasive strategy in all age categories. Although the largest absolute increase in the use of a routine invasive strategy was observed in low-risk patients, the FIR risk score without BMI and the age categories indicate that the relative increase in the use of a routine invasive strategy was comparable in all groups.
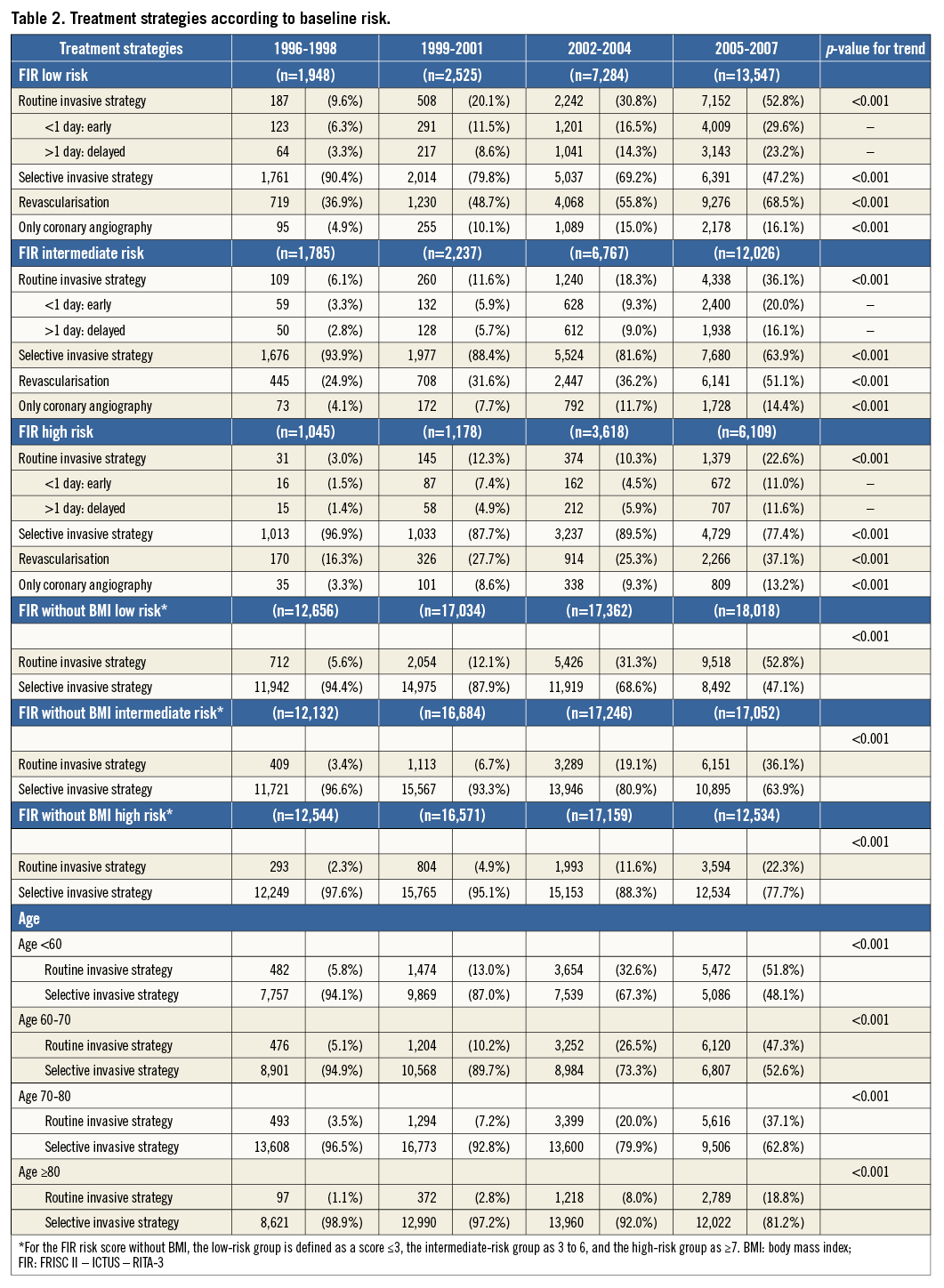
An increase in revascularisation rates, regardless of the treatment strategy, was observed in all risk groups. In the period 2005-2007, the percentages of revascularised patients were 68.5%, 51.1% and 37.1% in the low-, intermediate- and high-risk groups, respectively.
OUTCOMES
In the total population, there was a gradual decrease in three-year all-cause mortality over time, from 29.1% in the period 1996-1998 to 23.9% in the period 2005-2007 (Table 3). This was mainly driven by a decrease in three-year mortality in patients undergoing a routine invasive management. Event rates were relatively stable in patients undergoing a selective invasive management (Figure 1). Figure 1 shows that the three-year mortality hazards are decreasing in the routine invasively managed patients and are constant in the selective invasively managed patients and remain after adjustments for the risk profile of the patient and revascularisation status. Table 3 also shows the three-year death rates over time with regard to the baseline risk profile of the patients. The decrease in mortality was most obvious in the low-risk and intermediate-risk groups undergoing a routine invasive management. In patients in whom one or more of the variables needed to calculate the score were missing, the event rates were higher compared to patients with a calculated score (21.5% versus 30.1% in the period 1996-1998; 19.2% versus 29.2% in the period 1999-2001; 20.2% versus 30.1% in the period 2002-2004; 18.6% versus 31.6% in the period 2005-2007).
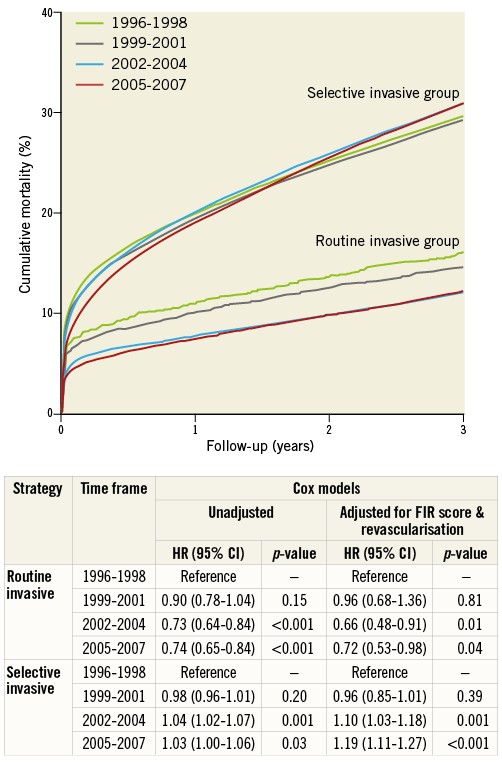
Figure 1. Three-year cumulative mortality according to treatment strategy. Cumulative unadjusted mortality estimated with the Kaplan-Meier method. The table presents the unadjusted and adjusted hazard ratios (HR) and 95% confidence intervals (CI) for mortality calculated with Cox proportional hazards models using the 1996-1998 time period as the reference.
Although patients who were revascularised during the initial hospitalisation had numerically lower mortality than non-revascularised patients, no reduction in mortality was observed in this patient group over the course of 12 years.
Discussion
Several implications can be drawn from the current report, describing the use of treatment strategies in a large NSTE-ACS population over a 12-year period in Sweden. First, there was a gradual increase in the use of a routine invasive strategy. Second, the routine invasive strategy was primarily utilised in patients at low baseline risk, although a similar relative increase over the 12 years was observed in all risk groups. Third, three-year mortality was reduced over the course of 12 years.
PREVIOUS STUDIES
Fox et al described temporal changes in hospital management and outcomes in ACS patients in the period 1999-2006, where an increase in coronary angiography and subsequent revascularisation was shown9. The increase in coronary angiography and subsequent revascularisation from 2002 to 2005 has also been shown in the CRUSADE quality improvement initiative10. The current study corroborates these results and extends it with information regarding the baseline risk profile of the patients. A comparable result has been observed in the Canadian GRACE population11.
ROUTINE INVASIVE VERSUS SELECTIVE INVASIVE MANAGEMENT
A recent patient-pooled meta-analysis has shown a long-term benefit in terms of cardiovascular death and MI with a routine invasive strategy2. One of the trials included in the meta-analysis, the ICTUS trial, could not demonstrate a benefit of the routine invasive strategy. However, in contrast to the other trials, the selective invasive strategy of ICTUS was characterised by a high rate of coronary angiography and subsequent revascularisation procedures12. Despite the intended treatment strategy, patients revascularised within the initial hospitalisation have lower event rates than non-revascularised patients13,14. In the current study, revascularised patients had a lower three-year mortality compared with non-revascularised patients. There was no trend to lower mortality in revascularised patients. However, these results are difficult to interpret because there are multiple factors that may causally interfere. We hypothesise that there was an increase in the baseline risk of revascularised patients over the years. Furthermore, changes over time in the revascularisation procedure in terms of technique, material, operator experience, and pharmacological treatment may have influenced these results.
RISK STRATIFICATION
Current international guidelines emphasise the importance of risk stratification in ACS. In the above-mentioned patient-pooled FIR analysis, the largest benefit of the routine invasive strategy was observed in high-risk patients2. In a report covering the Australian and New Zealand population of GRACE, temporal changes in baseline patient risk and intensity of evidence-based therapies were investigated15. Invasive management of the NSTE-ACS patients remained higher in patients at low to intermediate risk, compared with high-risk patients. Although the current report shows that the increase in the use of a routine invasive management and revascularisation was observed in the total cohort, the increase was paradoxically absolutely greatest in low-risk patients. There might be several explanations for the treatment-risk discrepancy. First, higher age is an important contributor to a high risk, and is also associated with multiple comorbidities. Undertreatment of elderly patients might occur because of overestimation of the procedural risk and an underestimation of the long-term benefits in elderly patients. A recent analysis by the FIR collaboration has shown that the largest benefit of the routine invasive strategy is observed in elderly patients16. This analysis also showed that age is the most important driver of the FIR risk score. Therefore, we hypothesise that the increase in low-risk patients can also be explained because cardiologists tend to perform coronary angiography earlier in younger patients. One has to keep in mind that this may also be related to the fact that the gradient of baseline risk between intervened and non-intervened elderly patients is greater than in younger patients, in other words, the elderly intervened patients are at potentially lower baseline risk.
Second, physicians may fail to recognise intermediate- to high-risk patients adequately. Previous studies have shown a misperception of the patients’ baseline risk by the treating physician17. The study by Lee et al showed that the primary reason for not referring a patient for cardiac catheterisation was that the patient was not considered high risk enough. However, according to the Thrombolysis In Myocardial Infarction risk score, around 60% of these patients were at intermediate to high risk. Finally, although most of the available risk scores include multiple components, many physicians rely on a few risk factors in their risk assessment18. These risk factors frequently include cardiac biomarkers and ST-segment deviation.
CLINICAL AND RESEARCH IMPLICATIONS
Two important implications arise from the current manuscript. First, it emphasises the importance of adequate risk stratification in clinical practice. Apparently, the group of patients with the highest rate of revascularisation is the group of low-risk patients. The routine use of one of the established risk scoring systems might assist in the triage of patients to different treatment strategies.
Second, while improvements in outcomes over time were observed in patients undergoing a routine invasive management, mortality rates seemed stable in the selective invasively managed patients. The majority of the clinical trials within NSTE-ACS focus on patients undergoing a routine invasive management, while the selective invasive group is underrepresented.
PHARMACOLOGICAL TREATMENT
Besides differences in treatment strategies over time with regard to coronary angiography, there have been developments in pharmacological treatment. Over time, there was a significant increase in guideline-recommended statins, platelet aggregation inhibitors (P2Y12 and GP IIb/IIIa inhibitors), and anticoagulants. These improvements in pharmacological treatments are potentially associated with the observed improvement in outcomes.
STRENGTHS AND LIMITATIONS
The strengths of the study are that it covers consecutive NSTE-ACS patients admitted to unselected hospitals in the Swedish nationwide registry over a time period spanning more than 12 years. The data are prospectively collected, and the quality is validated by random monitor checks.
Several limitations deserve mention. First, we defined the routine invasive and selective invasive treatment strategies in line with the definitions used in current guidelines1. However, the intended treatment strategy was not captured in the SWEDEHEART registry. This could have caused a selection bias because of crossover to either strategy from the intended strategy because of clinical signs or symptoms. Because of potential crossover, the event rates in the routine invasive group are not directly comparable to those in the selective invasive group. However, the data are representative for the invasive management over 12 years with respect to the patients’ baseline risk profile. Second, we were not able to calculate the FIR risk score for all patients because of missing values. However, even though this group with missing values was characterised by higher event rates than complete cases, the increase in the use of the routine invasive strategy was still lower than that observed in the low-risk group. Finally, although the results are adjusted for in-hospital revascularisation, there might be a residual survival bias with catheterisation/revascularisation as a marker for survival.
Conclusion
In conclusion, there has been an increase in the use of a routine invasive strategy in NSTE-ACS patients over the course of 12 years in Sweden. An absolute increase was mainly observed in low-risk patients, while a similar relative increase was observed in all risk groups. There was a decrease in long-term mortality over the same time course.
| Impact on daily practice There has been an increase in the use of a routine invasive strategy in NSTE-ACS patients over the course of 12 years in Sweden. There was a decrease in three-year mortality over the same time course. Paradoxically, the routine invasive strategy was primarily utilised in patients at low baseline risk, emphasising the importance of implementation of guideline-recommended risk stratification. |
Acknowledgements
We thank all the participating hospitals and patients contributing to the SWEDEHEART registry.
Funding
The SWEDEHEART registry is supported by the National Board of Health and Welfare, the Swedish Society of Cardiology, and the Swedish Association of Local Authorities and Regions.
Conflict of interest statement
The authors have no conflicts of interest to declare.
References