Abstract
Aims: In patients with acute coronary syndromes (ACS), percutaneous coronary intervention (PCI) is the mainstay of treatment based on current guidelines. In this paper we describe contemporary management and outcomes of patients with ACS treated by PCI in the national ACS Israeli survey (ACSIS) performed in March and April 2010.
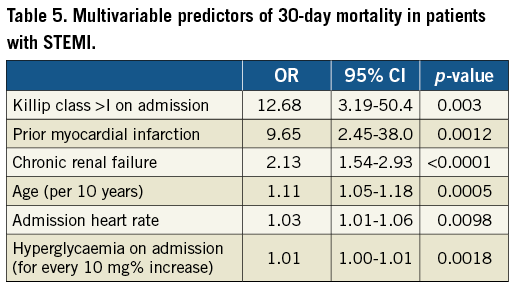
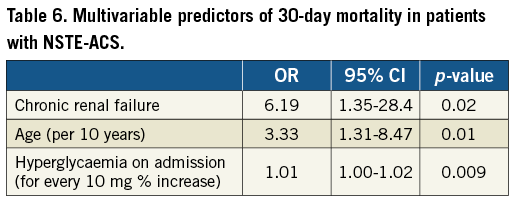
Methods and results: The ACSIS 2010 registry was conducted in all 25 hospitals in Israel and included “all comers” admitted with ACS. In-hospital and 30-day outcome was assessed. The registry included 2,193 patients with ACS. Coronary angiography was performed in 86.1% and PCI in 75.1% of cases. The mean age was 62.5 years, the transradial approach was used in 32% of patients and overall use of drug-eluting stents was 34%. Procedural complications were extremely low at less than 1%. The thirty-day mortality rate was 2.1% and the repeated myocardial infarction (MI) rate was 2.5%. The major adverse cardiac and cerebral events (MACCE) rate was 5.6%. Multivariable analysis identified age, chronic renal failure, and hyperglycaemia on admission as independent predictors of 30-day mortality for all subsets of ACS, and Killip class >I on admission and prior MI for patients with ST-elevation ACS only.
Conclusions: When evidence-based medicine is applied in the treatment of patients with ACS, clinical outcome is favourable. Several clinical predictors identify high-risk patients who require special attention.
Introduction
In patients with ST-elevation (STE) and non-ST-elevation (NSTE) acute coronary syndrome (ACS) percutaneous coronary intervention (PCI) is the mainstay of treatment based on current guidelines1,2. In randomised controlled studies, both primary PCI for STE-ACS3 and early PCI in moderate to high risk NSTE-ACS4 have been shown to lower short- and long-term mortality rates.
Several registries evaluated the “real life” outcomes of patients with ACS. Most of these studies were performed prior to the widespread and comprehensive use of drug-eluting stents, aspiration thrombectomy, and aggressive antiplatelet and potent statins. In this paper we describe contemporary management and outcomes of patients with ACS treated by PCI in the national ACS Israeli survey (ACSIS) performed in March and April 2010.
Methods
THE ACSIS AND ACSIS-PCI 2010 REGISTRIES
The ACSIS is a nationwide survey of all patients admitted during the study period to the intensive cardiac care units and cardiology wards in all 25 hospitals in Israel (10 hospitals with cardiac surgery back-up). This registry has been performed since 2000 every two years over a two-month period (2000, 2002, 2004, 2006, 2008, 2010). In 2010 the survey was conducted in March and April and for the first time a parallel designated survey (ACSIS-PCI) collected detailed parameters of coronary interventions performed in these ACS patients. The survey received the local ethics committee approval in each hospital. Demographic, historical, clinical, and procedural data were recorded on pre-specified forms for all patients admitted with a diagnosis of ACS. Patients were treated at the discretion of each centre. All patients were either seen in the clinic or interviewed by telephone at 30 days. The ACSIS-PCI registry included multiple parameters on the extent of coronary artery disease, culprit vessel, vascular access, procedural strategy and device selection including the type and number of stents used, use of aspiration thrombectomy during primary PCI, procedural complications, and outcome.
In this study we describe the baseline characteristics, procedural details and outcome of consecutive ACS patients included in the ACSIS-PCI registry attempting to emphasise the contemporary use of PCI across the ACS spectrums (STE-ACS and NSTE-ACS). Thirty-day endpoints were defined as death, repeat myocardial infarction, stroke, major bleeding, definite stent thrombosis according to the academic research consortium (ARC) definitions5 and major adverse cardiac and cerebral events (MACCE) (combined endpoint of death, myocardial infarction, stroke and stent thrombosis). Our outcome data were compared to the most contemporary randomised study that included ACS patients undergoing PCI – the CURRENT-OASIS 7 study6. By multivariable analysis, predictors of 30-day mortality in STE-ACS and NSTE-ACS were identified. Furthermore, we show a longitudinal trend in 30-day mortality over a decade from 2000 to 2010.
STATISTICAL ANALYSIS
Data are presented as percentages and as mean±SD for categorical and continuous variables, respectively. Multivariable stepwise logistic regression analysis was performed including all baseline variables that were presumed to influence outcome in order to find independent predictors for 30-day mortality in terms of odds ratio with 95% confidence intervals (CI), separately for patients with STEMI and NSTE-ACS using SPSS software (version 8.2) (SPSS Inc., Chicago, IL, USA).
Results
PATIENTS INCLUDED IN THE ACSIS-PCI REGISTRY
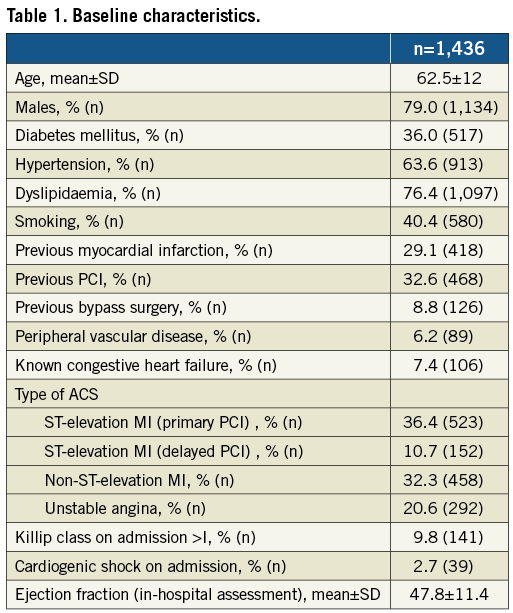
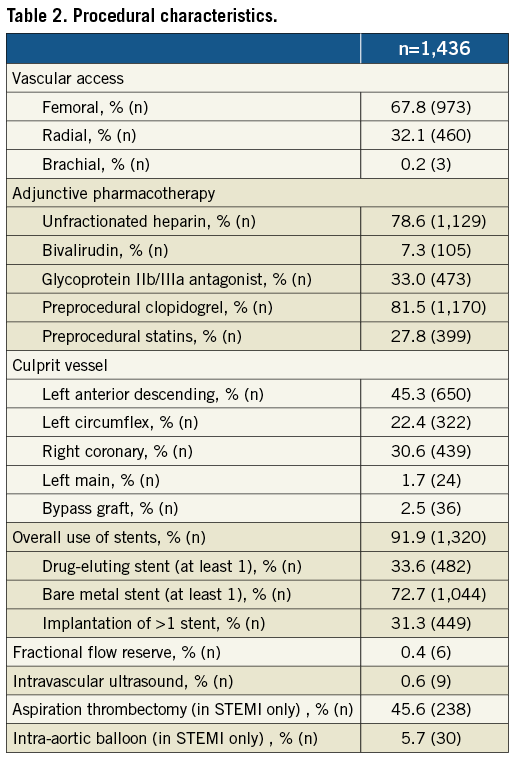
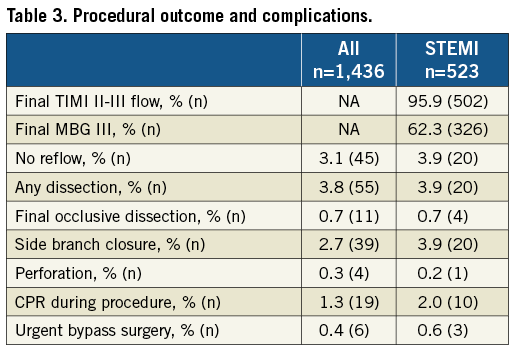
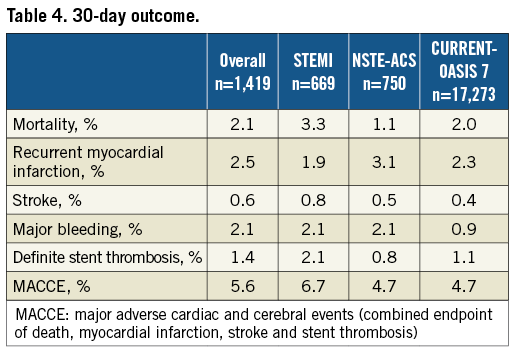
The 2010 registry included 2,193 patients with ACS. Diagnostic coronary angiography was performed in 1,890 (86.1%). PCI was performed in 1,419 patients (75.1% of diagnostic procedure or 64.7% of all ACS patients) in 1,794 lesions. Baseline characteristics of all patients undergoing PCI are summarised in Table 1. Mean age was 62.5 years with 79% of males. Risk factor profile showed 36% with diabetes mellitus, 64% with hypertension and 76% with treated dyslipidaemia. One third of patients had previously known coronary artery disease. Procedural data are summarised in Table 2. Radial access was used in 32% of patients and the overall use of at least one drug-eluting stent was 34%. Use of adjunctive invasive imaging or physiological assessment during angiography was extremely low at less than 1%. In STE-ACS patients, thrombus aspiration was attempted in almost 50%. Procedural complications (Table 3) were relatively low with an overall rate of urgent bypass surgery of 0.4%. Thirty-day mortality rate was available in 98% of patients and was favourable at 2.1% and re-MI was observed in 2.5% of patients. Other outcome measures are summarised in Table 4. After multivariable analysis, independent predictors for 30-day mortality are presented for STE-ACS and NSTE-ACS in Table 5 and Table 6, respectively. As shown in Table 6, when compared to the most contemporary PCI randomised study in ACS patients, the CURRENT-OASIS-7 trial, outcome measures were similar to our registry.
TEMPORAL TRENDS
Thirty-day mortality in patients with ACS undergoing PCI was reduced significantly from 2000 to 2010 (Figure 1) (overall 4.6% to 2.3% [p for trend=0.008]; in STE-ACS from 6.6% to 3.3% [p for trend=0.02]; and for NSTE-ACS from 1.7 to 1.3% [p for trend=NS]). In our registry, 30-day mortality in patients with ACS who were treated conservatively was 3.8%. From 2000 to 2010, in all ACS patients, the rate of coronary angiography had increased from 58.4% to 86.1% (p for trend <0.0001). Among patients undergoing coronary angiography, the PCI rate had increased from 64.2% to 75.1% (p for trend <0.0001). Moreover, from 2000 to 2010, the rate of primary reperfusion in STE-ACS had increased from 56.4% to 71.5%. The mode of primary reperfusion changed significantly over this period: where in 2000 only 18.3% received primary PCI, in 2006 76.7% received primary PCI and the rate in 2010 was 96.9% (p for trend <0.001).
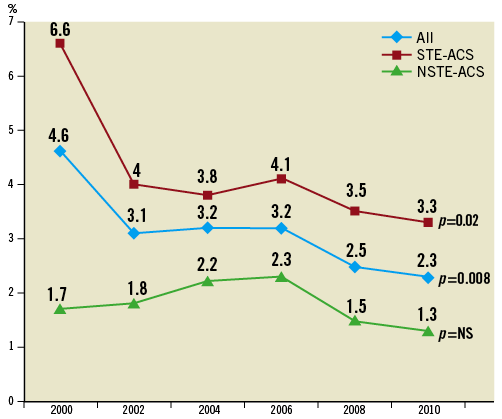
Figure 1. Trends of 30-day mortality rates from 2000 to 2010.
Discussion
We describe herein a comprehensive, contemporary national registry of unselected patients admitted with a wide spectrum of ACS and undergoing PCI. In the majority of patients (86%), coronary anatomy was assessed by invasive angiography and most of these patients had subsequent PCI as indicated by current guidelines. In this contemporary description of our consecutive “all comers” ACS patients we observed a favourable short-term outcome in general, and as compared to a contemporary clinical trial including selected ACS patients undergoing PCI6.
In our national registry, drug-eluting stents (DES) were used in ~30% of our ACS patients. Drug-eluting stents were shown to be superior for restenosis prevention compared to bare metal stents in patients undergoing primary PCI7. Moreover, manual aspiration devices were shown to improve one-year survival in patients undergoing primary PCI for STE-ACS8,9. This was significantly implemented in our registry with almost half of the patients having this intervention during primary PCI. Thus in general, the implementation of evidence-based guidelines was frequent in the ACSIS-PCI registry.
Major bleeding is considered an independent predictor of mortality in all ACS patients regardless of their clinical presentation10,11. Major bleeding has been demonstrated to be lower in patients with ACS undergoing PCI via the radial approach12. Radial access has been adopted by many interventional cardiologists in Israel over the last few years as shown in this registry (32.1%). The transradial approach is probably particularly advantageous in patients with ACS due to the administration of an adjunctive potent antithrombotic regimen therefore leading to an increased risk of bleeding13.
In the ACSIS registry, the mortality rate at 30 days was 2.1%, which is an extremely low figure for an “all comers” ACS registry. When compared to the most contemporary randomised clinical trial, CURRENT-OASIS 76, which enrolled younger ACS patients with a lower prevalence of diabetes, mortality rates were similar at 30 days. This low mortality rate may be attributable to the immediate access to emergent PCI in all hospitals throughout Israel, with primary PCI performed seven days a week and 24 hours a day. Serious procedural complications such as final occlusive dissection, perforation, cardio-pulmonary resuscitation during the procedure and the need for urgent bypass surgery were extremely low. This may support the approach that complex PCI in the setting of ACS can be safely performed in hospitals without surgical backup (in our registry 15 out of 25 hospitals).
We identified clinical independent predictors of 30-day mortality separately for patients with NSTE-ACS and STE-ACS. Variables included age, chronic renal failure and hyperglycaemia on admission for both subsets, and prior myocardial infarction and heart failure on admission for patients with STE-ACS only. With some similarities, a sub-analysis of the ACUITY study found renal insufficiency, biomarker elevation, ST-segment deviation, non-use of aspirin or thienopyridine, insulin-treated diabetes, older age, baseline lower haemoglobin value, history of percutaneous coronary intervention, and current smoking to be independently associated with 30-day or one-year ischaemic events14. Fefer et al have previously shown that in patients undergoing primary PCI, increased fasting glucose and previously diagnosed diabetes mellitus were associated with less spontaneous reperfusion and less myocardial reperfusion, resulting in worse clinical outcomes15. Similar to our finding, in patients admitted with NSTE-ACS, analysis from the Canadian ACS registries showed that in NSTE-ACS patients, heart failure on admission was associated with a two-fold increase in one-year mortality16.
Limitations
Our study has several limitations. Data in the present study are derived from a registry rather than from a randomised clinical trial. However, these types of registries represent real-world practice and include a much broader range of patients with older age and comorbidities that often lead to exclusion from randomised trials. Moreover, national ACSIS and ACSIS-PCI registries are unique by the inclusion of all ACS patients in Israel including all hospitals.
Conclusions
In conclusion, when evidence-based medicine is applied in the treatment of patients with acute coronary syndromes, including such measures as transradial approach, selection of drug-eluting stents, aspiration thrombectomy, and the use of an aggressive antithrombotic regimen, the clinical outcome is favourable and improved significantly over a decade. Older age, the presence of chronic renal failure and heart failure on admission identify high-risk patients who require special attention.
Acknowledgements
We are indebted to all the physicians and nurses who participated in ACSIS 2010. The Israel Society for the Prevention of Heart Attacks for the data management and analysis, Interventional Cardiology and Intensive Cardiac Care Working Groups of the Israel Heart Society, and the Israel Center for Disease Control.
Conflict of interest statement
The authors have no conflicts of interest to declare.

