Abstract
Aims: The elderly constitute an increasing proportion of all patients with acute coronary syndromes (ACS). However, increased age has been identified as an important risk factor for adverse events and complications of ACS and treatment. The purpose of this study was to investigate age-related differences in presentation and diagnostics, as well as contemporary treatment and outcome in a large series of elderly patients receiving an invasive strategy for ACS.
Methods and results: The present study is an analysis of all patients, who were enrolled in the German Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte (ALKK) registry in 2008. To assess age-related differences, subjects were divided into three groups: (<75 yrs, 75 to 85 yrs and >85 yrs). Out of 19,708 consecutive patients who were admitted for the treatment of ACS and enrolled in the ALKK registry, 14,174 (71.9%) were <75 yrs, 4,685 (23.8%) were between 75 and 84 yrs and 849 (4.3%) patients were >85 yrs. Therapy recommendation after diagnostic angiography was conservative in 24.6% of the youngest, in 25.1% of the elderly, and in 25.3% of the very elderly patients. Interventional success rates were 95.2% in the youngest vs. 93.1% in the elderly and very elderly patient group (p<0.001). Overall in-hospital event rate increased significantly with age (3.4% vs. 7.4% vs. 8.3%, respectively; p<0.001).
Conclusions: Our analysis shows that there is a high success rate among the large proportion of elderly patients who are treated for ACS by an intervention. Complication rates increased significantly, however, with age.
Introduction
The elderly constitute an increasing proportion of all patients who are admitted into hospital for treatment of acute coronary syndromes (ACS)1,2. However, increased age has been identified as an important risk factor for death or recurrent myocardial infarction (MI) in this subset3-6. In the past, this resulted in reluctance to perform invasive procedures in elderly patients. Additionally, as the intervention itself conveys a higher risk for complications7,8, investigators have universally observed that the use of invasive diagnosis and therapy decreases with increasing age6,9-13.
However, there is strong evidence that high risk subsets, i.e., elderly patients, may actually gain most from an intervention14-16. This recent observation that elderly patients have the potential for the highest benefit from the intervention has lowered thresholds for considering aggressive revascularisation strategies in this patient group11,12,17. Therefore, we analysed data from the registry of the German Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte (ALKK) to examine the epidemiology and contemporary in-hospital management of patients with ACS to assess age-related differences in presentation, diagnostics and treatment in a large series of patients receiving invasive strategy.
Methods
The ALKK (Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte) registry is a prospective registry that was initiated in 1992 to monitor quality control and contains all consecutive diagnostic angiographic and interventional procedures of the participating hospitals on an intention-to-treat basis18-21. Data were obtained by standardised questionnaires in the 42 participating hospitals, including information about the medical history (prior coronary interventions, congestive heart failure [CHF], diabetes mellitus, renal insufficiency), the indication for the procedure, the adjunctive antithrombotic therapy, the procedure itself (target vessel, success rate, stent used, etc.), and the complications until hospital discharge. All data were analysed centrally at the Karl Ludwig Neuhaus Datenzentrum, Ludwigshafen, Germany.
The present study is an analysis of all patients with ACS, who were consecutively enrolled in 2008 into this registry.
To assess possible age-dependent differences, subjects were divided into three groups according to age (<75 yrs, 75 to 85 yrs and >85 yrs). Our analysis focused on age-associated differences in clinical and angiographic characteristics, the use of revascularisation procedures and in-hospital mortality and complication rates. The first procedure performed in each patient during hospital stay was considered for this analysis.
Data collection
Data on patient characteristics upon admission comprised age, gender, concomitant diseases, cardiovascular risk factors, prior percutaneous coronary intervention (PCI) or prior coronary artery bypass graft (CABG) procedures, prior myocardial infarction and stroke.
Following completion of the procedure, intra-procedural medication, lesion characteristics, details of the intervention and intra-procedural and in-hospital adverse cardiovascular outcomes were recorded on a standardised form by the treating physician and transmitted to the central data registry centre in Ludwigshafen via the Internet by the treating physician.
DEFINITIONS
STEMI (ST-elevation myocardial infarction) was defined as ST-segment elevation of ≥2 mm in ≥2 precordial leads or >1 mm in ≥2 extremity leads, NSTEMI (non-ST-elevation myocardial infarction) was defined as any significant increase in troponin I level without ST-elevation in the defining ECG.
Adverse outcome (major adverse cardiac or cerebrovascular event [MAC{C}E]), defined as in-hospital death, myocardial infarction, stroke and reinfarction was evaluated.
Myocardial infarction was defined as a two-fold rise in creatine-kinase level above normal.
Cerebrovascular event (CVA) was defined as stroke, transitory or reversible cerebral ischaemic attacks that were confirmed clinically as a permanent neurological deficit or by CT-scan.
Besides the above, pulmonary embolism, resuscitation, complications at the puncture site, acute renal failure, requirement of dialysis, septicaemia and urgent coronary artery bypass graft procedure were reported as in-hospital events.
Statistical methods
Statistical analysis was performed using the SAS software package version 9.1 (SAS Inc., Cary, NC, USA) The study population is described in absolute numbers, percentages and medians with 25th and 75th percentiles, as appropriate. Trends in distribution of binary variables across the age groups were analysed using a Cochran-Armitage test, trends of continuous variables using a Jonckheere-Terpstra test. The Pearson χ2 test was used to examine differences and trends in categorical variables. Continuous variables were compared by the Mann-Whitney-Wilcoxon test. Statistical significance was defined as 2-sided p-values ≤0.05.
Results
The present analysis was based on the data of 19,708 patients enrolled in the ALKK registry, who had been admitted consecutively for treatment of ACS in 43 hospitals in Germany. Of these, 14,174 (71.9%) were <75 yrs, 4,685 (23.8%) were between 75 and 84 yrs and 849 (4.3%) patients were >85 yrs.
In patients receiving PCI, median hospitalisation time increased significantly with age from six days in patients <75 yrs to seven days in patients ≥75 yrs (p<0.0001).
Clinical characteristics and baseline data
The baseline characteristics of the patients in the three different age groups are shown in Table 1. The percentage of women increased with age. Regarding conventional cardiovascular risk factors, only cigarette smoking was more prevalent in the youngest age group. The prevalence of hypercholesterolaemia and diabetes was highest between 75 and 85 years. Hypertension increased with age. Previous PCI and coronary artery bypass graft (CABG) procedures were more frequent among patients between 75 and 84 years and were seen significantly less often in patients aged >85 years (previous PCI: 22.6% vs. 27.8% vs. 21.3%, respectively [p<0.001]; previous CABG: 7.9% vs. 13.9% vs. 8.6%, respectively [p<0.001]).
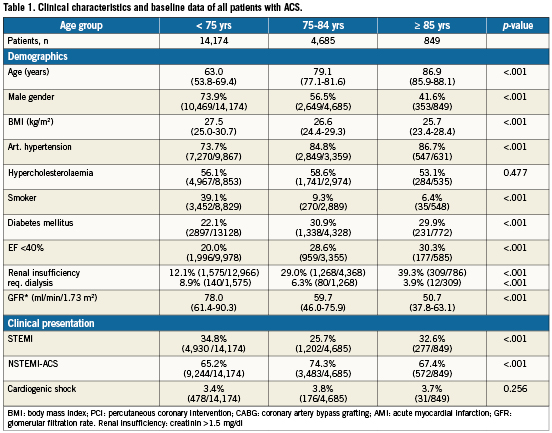
Regarding 1,392 (10.1%) patients presenting with congestive heart failure, we noted a significant increase the higher the age (8.9% vs. 12.6% vs. 15.7%, respectively; p<0.001) in patients, in whom PCI was performed. However, rates of cardiogenic shock and the use of haemodynamic support devices were not significantly different between the three age groups.
Diagnostic coronary angiography
In total 19,527 coronary angiographies were performed, primarily via a femoral access (85.7% vs. 87.4% vs. 87.8%, respectively; overall 86.2%; p=0.06). The proportion of three-vessel disease was highest in the very elderly group (35.8% vs. 49.7% vs. 49.7%, respectively; p<0.001). No coronary artery disease (CAD) was diagnosed during angiography in significantly more patients of the younger group (5.3% vs. 2.5% vs. 1.7%, respectively; p<0.001).
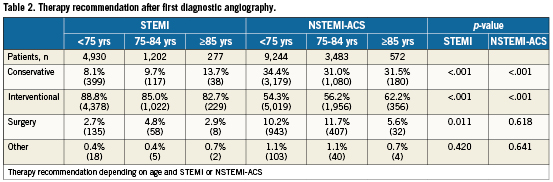
Therapy recommendation after diagnostic angiography was conservative in 24.6% (STEMI: 8.1%; NSTEMI: 34.4%) of the youngest, in 25.1% (STEMI: 9.7%; NSTEMI: 31.0%) of the elderly, and in 25.3% (STEMI: 13.7%; NSTEMI: 31.5%) of the very elderly patients (Table 2).
Percutaneous coronary intervention
If therapy recommendation was interventional after diagnostic angiography, ad hoc PCI was performed in the majority of cases in all age groups (98.0% vs. 96.8% vs. 97.0%, respectively; p=0.0002). Only patients who had at least a diagnostic angiography were included in the registry.
Patients with STEMI
In elderly and very elderly patients, significantly, more often >1 vessel was treated or PCI was performed in the presence of three-vessel disease (<75 yrs: STEMI:7.2% and NSTEMI: 9.8%; 75> yrs<85: STEMI: 9.9% and NSTEMI: 12.5%; >85 yrs: STEMI:8.5% and NSTEMI: 17.7%; STEMI: p=0.009; NSTEMI p<0.001; Table 3).
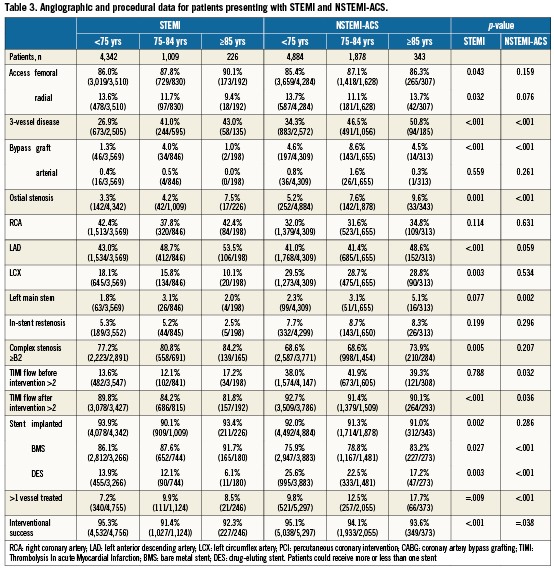
A significantly higher proportion of the elderly and very elderly patients presented with signs of severe congestive heart failure during intervention (572 of 4,756 [12.0%] in the youngest age group vs. 194 of 1,124 [17.3%] of the intermediate age group vs. 48 of 256 patients [19.5%] in patients >85 yrs; p<0.001) but not of cardiogenic shock. In 6.9%, haemodynamic support devices were used with no significant age-dependant differences.
Intervention of an ostial stenosis in one of the three main vessels or of an unprotected left main stenosis was significantly more common in the group > 75 yrs. Rates of intervention utilising a saphenous vein graft were higher in the elderly than in the younger and very elderly groups. Treatment for total occlusion decreased with increasing age, but this finding was not significant. Overall success rates were highest in the youngest age group and significantly lower for both the elderly and very elderly (Table 3).
Patients with NSTEMI
In NSTEMI patients a continuous, age-dependant rise in congestive heart failure was noted (5.9% vs. 10.0% vs. 13.1%, respectively; p<0.001). In contrast to that, the application of haemodynamic support devices, predominantly the use of an intra-aortic balloon pump and the incidence of cardiogenic shock did not differ significantly. Comparable to the STEMI cohort, significantly, more often >1 vessel was treated or PCI was performed in the presence of three-vessel disease.
The complexity of the intervention increased with age. The rates of intervention in the cases of an ostial stenosis in one of the three main vessels, unprotected left main stenosis, intervention of a saphenous vein graft, intervention in the last remaining vessel or intervention of a complete occlusion were significantly lower in the 75> yrs<85 group with a further decrease in the very elderly group (Table 3).
Vascular closure devices (VCD) were used significantly less often in elderly and very elderly NSTEMI-ACS patients, whereas in STEMI patients VCD were used slightly more frequently in STEMI patients, but this difference in finding was not significant.
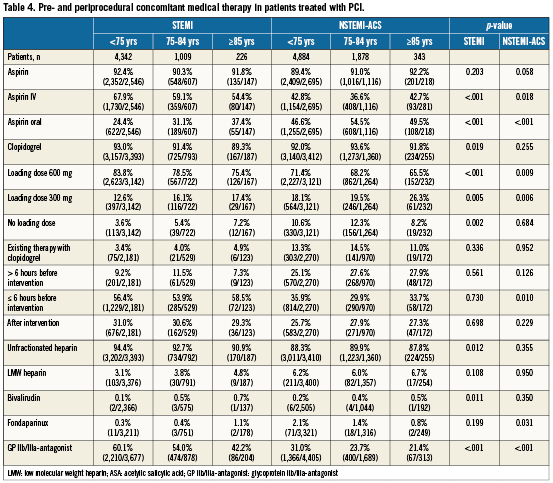
Medical treatment in patients undergoing PCI
Elderly patients were less likely to receive a guideline recommended antithrombotic therapy (Table 4). Elderly patients with either STEMI or NSTEMI-ACS were less likely to receive a loading dose of 600 mg of clopidogrel but more frequently a loading dose of 300 mg (STEMI p<0.001; NSTEMI p=0.003). With increasing age, more patients were on oral aspirin prior to the intervention (p<0.001). The use of IIb/IIIa antagonists decreased with increasing age for both patients with STEMI and NSTEMI (p<0.001). There was no significant difference found in the use of heparin, low molecular weight heparin, bivalirudin or fondaparinux in both groups.
In-hospital event rates
Overall intraprocedural events increased with increasing age (Table 5). Intraprocedural mortality rate was highest in the very elderly patients (0.4% vs. 0.6%. vs. 1.3%, respectively; p=0.002). In-hospital MACE rate was 3.0% (2.1% vs. 5.2% vs. 6.2%, respectively; p<0.001). Overall event rate increased significantly with age (3.4% vs. 7.4% vs. 8.3%, respectively, and was nearly four-fold in patients >85 years.
Regarding the different cohorts (STEMI or NSTEMI-ACS) overall intraprocedural event rate increased with increasing age in patients with NSTEMI, but not in patients with STEMI, where a maximum of patients was found in the intermediate, >75 yrs and <85 yrs, group. In both STEMI and NSTEMI-ACS patients, a significantly higher stroke rate was found in the very elderly group (p<0.001).
Pertaining to the group of patients with STEMI there was a significantly higher periprocedural mortality rate found for patients >75 yrs (p=0.014), with no further increase in the very elderly group. The rates of procedural-related cardiogenic shock, coronary occlusion of the infarct-related artery and reanimation were not significantly different.
In patients with NSTEMI a significantly higher mortality rate was found in the very elderly group. Although STEMI patients did have a higher rate of intraprocedural resuscitation, there was no significant difference found in all other procedural-related events mentioned earlier.
Event rate in patients with purely diagnostic angiography
In STEMI patients, in-hospital mortality, overall event rate (MAC[C]E including pulmonary embolism, non-MACE resuscitation, septicaemia, complications at the puncture site, acute renal failure and dialysis) was highest in the intermediate age group. In contrast, NSTEMI-ACS patients’ event rates were highest in the very elderly group.
Event rates in patients with diagnostic angiography and PCI
In STEMI-patients, higher event rates were found in patients who received PCI in comparison to those who received non-interventional angiography. Rates of mortality, MAC(C)E and of all in-hospital events were highest in the very elderly group.
Similarly to that, in patients with NSTEMI-ACS hospital mortality and MAC(C)E-rates, as well as the proportion of all in-hospital events were highest in the very elderly cohort (Table 5).
Discussion
In recent years, increasing evidence has suggested that patients at risk, including elderly patients, gain most from invasive procedures in the presence of ACS14-16. The extent to which this evidence has impacted on real world management of elderly patients with ACS remains unclear. The present analysis was performed to investigate the common practice in diagnosing and treating elderly patients with ACS.
In this multicentre observation we found substantial, age-related differences in the diagnosis and treatment of elderly patients presenting to the hospital with acute myocardial infarction.
Our results confirm that elderly patients are a significant and increasing proportion of the total population treated for ACS1,2,19. The proportion of 28.1% elderly patients in the more recent 2008 ALKK registry data is 2.4% higher than the numbers enrolled in the older Global Registry of Acute Coronary Events (GRACE) registry, which included 24,165 patients with a rate of 25.7% subjects >75 yrs, possibly suggesting an increase in patients >75 yrs over time1.
In a recently published registry of patients with NSTEMI ACS, over 35% of the population were >75 yrs, emphasising the growing importance of examining outcomes in the older age group22. In contrast to a significant difference in treatment modalities between elderly and younger patients (invasive strategy 39% vs. 56% with a 30-day mortality nearly four times higher in the elderly population) reported in that study, age-related differences in diagnostics or the percentage of patients who were treated with PCI in comparison to the younger patient cohort were much less pronounced.
Therefore, our data show a trend towards a stronger adherence to evidence-based medicine with increased utilisation of resources in elderly patients albeit that the recommendations were primarily based on younger cohorts.
Consistent with other studies, we found higher rates of atherosclerotic disease in the elderly, whereas the rate of patients with a history of previous CABG and PCI was not significantly different from younger patients; hypertension was more common and hypercholesterolaemia and cigarette smoking were less common in the elderly2,6,7.
In the presence of a higher rate of three-vessel disease, we found a significantly lower success rate in elderly patients. Attempting to explain this phenomenon, our analysis reveals that although TIMI flow rates after the intervention were not significantly different between the three age groups, a significantly higher proportion of elderly patients had interventions with specific characteristics. Besides the category “intervention in a completely occluded artery”, lesions in elderly patients were more than two-fold more complex in all other categories, i.e., intervention in >1 vessel, left main intervention, ostial stenosis and intervention in the last remaining vessel. Lesion complexity results in a significantly higher proportion of stents with smaller diameter, which is a potential source of stent thrombosis and in-stent restenosis. This factor may, at least partly, explain the lower success rates found in this registry.
Secondary to the negligibly lower use of bivalirudin, we found significantly lower rates in the loading dose for elderly patients with either 300 or 600 mg of clopidogrel. Additionally, use of GP IIb/IIIa antagonists was significantly lower in elderly patients, mainly due to the fear of bleeding complications.
Complication rates were three-fold in very elderly patients. However, although primary success rates were worse, the number of AE in the elderly remained in a range that is concordant with the literature and, thus, the benefits gained from intervention outweigh the complications9,14-16,21,22.
Despite technical advances in recent years, percutaneous revascularisation in the elderly still has a relatively high mortality rate, primarily due to increased multimorbidity as an inherent consequence of advanced age, but secondarily as a consequence of a greater prevalence of multivessel disease and depressed left ventricular function23-25.
Conclusion
Our analysis shows a high interventional success rate in elderly patients treated with PCI for ACS, which is comparable to a younger patient cohort. It shows an increase in the use of effective therapies for those patients who are forwarded to PCI after diagnostic angiography and the complication rates, which are higher in an elderly and very elderly population compared to a younger patient cohort. Albeit that the present study provides valuable information about the current treatment of and outcome for elderly patients with ACS, the impact of age on clinical decision-making requires further evaluation and more attention should be devoted to the elderly population with ACS in clinical research and especially in randomised trials.
Limitations
The present analysis is an observational registry and not a randomised trial. Since the treatment of elderly patients was effectively left to the discretion of the treating cardiologist, the registry only reflects those patients who proceeded to an intervention. On the one hand, this may result in a selection bias, but on the other hand perhaps this strategy reflects the current clinical practice in Germany.
The rates of in-hospital myocardial infarction reported in this registry are very low. This might be caused by the fact that death was reported as death and the underlying re-infarction was not reported as MI. Although of interest, the registry does not provide the answer to the question of in how many cases a staged procedure was performed. A further limitation is that there was no multivariate analysis performed regarding variables, which could have potentially affected the outcome, such as the influence of a loading dose of clopidogrel and the use of IIb/IIIa-inhibitors or a relation between bleeding and in-hospital death in the elderly group.
Conflict of interest statement
All authors have no conflict of interest to declare in relation to this paper.