Abstract
Aims: Current guidelines recommend an early invasive strategy in patients with non-ST-segment elevation acute coronary syndromes (NSTEACS). The role of an invasive strategy in frail elderly patients remains controversial. The aim of this substudy was to assess the impact of an invasive strategy on outcomes according to the degree of frailty in these patients.
Methods and results: The LONGEVO-SCA registry included unselected NSTEACS patients aged ≥80 years. A geriatric assessment, including frailty, was performed during hospitalisation. During the admission, we evaluated the impact of an invasive strategy on the incidence of cardiac death, reinfarction or new revascularisation at six months. From 531 patients included, 145 (27.3%) were frail. Mean age was 84.3 years. Most patients underwent an invasive strategy (407/531, 76.6%). Patients undergoing an invasive strategy were younger and had a lower proportion of frailty (23.3% vs. 40.3%, p<0.001). The incidence of cardiac events was more common in patients managed conservatively, after adjusting for confounding factors (sub-hazard ratio [sHR] 2.32, 95% confidence interval [CI]: 1.26-4.29, p=0.007). This association remained significant in non-frail patients (sHR 3.85, 95% CI: 2.13-6.95, p=0.001), but was not significant in patients with established frailty criteria (sHR 1.40, 95% CI: 0.72-2.75, p=0.325). The interaction invasive strategy-frailty was significant (p=0.032).
Conclusions: An invasive strategy was independently associated with better outcomes in very elderly patients with NSTEACS. This association was different according to frailty status.
Abbreviations
ACS: acute coronary syndromes
LONGEVO-SCA: Impacto de la fragiLidad y Otros síNdromes GEriátricos en el manejo y pronóstico Vital del ancianO con Síndrome Coronario Agudo sin elevación de segmento ST
MNA-SF: mini nutritional assessment - short form
NSTEACS: non-ST-segment elevation acute coronary syndromes
Introduction
Clinical guidelines recommend an invasive strategy in most patients with non-ST-segment elevation acute coronary syndromes (NSTEACS). However, these recommendations are based on studies in which older patients were underrepresented. Although several studies suggested a clinical benefit from an invasive strategy in highly selected elderly patients1, this benefit could be lost in patients with a high degree of comorbidity2.
Comorbidities and frailty are associated with higher rates of complications and consumption of healthcare resources3. Several authors have described a significant association between frailty and a worse prognosis in patients with ACS4-10. In addition, frail patients are less often treated with recommended drugs at discharge10. However, little information exists about the benefit of an invasive strategy in frail elderly patients with NSTEACS.
The LONGEVO-SCA registry11 (Impacto de la fragiLidad y Otros síNdromes GEriátricos en el manejo y pronóstico Vital del ancianO con Síndrome Coronario Agudo sin elevación de segmento ST) is a multicentre study conducted to assess the characteristics of a cohort of unselected elderly patients with NSTEACS. In this study a comprehensive geriatric assessment was performed during admission. The main results of the study have already been reported12. A complete list of the LONGEVO-SCA registry investigators can be found in Supplementary Appendix 1. In summary, an easy assessment of frailty status at baseline predicted six-month mortality, independently from other important predictors such as age, Charlson index and GRACE score. The goal of this substudy was to assess the impact of an invasive strategy on outcomes according to the degree of frailty in these patients.
Methods
DESIGN AND STUDY POPULATION
This is a prospective, observational study conducted in 44 Spanish hospitals. The design has previously been described in detail11. Briefly, the study included consecutive patients aged ≥80 years admitted for NSTEACS, defined as the presence of chest pain and at least one of the following: a) ECG changes suggestive of myocardial ischaemia, and/or b) elevated markers of myocardial damage. Signed informed consent by the patient or representative in cases of cognitive impairment was required. Patient refusal to participate in the registry and the impossibility of obtaining the geriatric tests were considered exclusion criteria. Patients with severe comorbidities were only excluded if symptoms of myocardial ischaemia were clearly triggered only by other conditions such as acute anaemia, severe decompensated respiratory insufficiency, active infectious diseases or severe coexisting heart valve disease (type 2 myocardial infarction).
Decisions on antithrombotic treatment and performance of coronary angiography were left to the discretion of each medical team according to current recommendations. If coronary angiography was performed, vascular access, antithrombotic drugs and the choice of stents or other devices were left to the operator’s decision.
DATA COLLECTION
Data were prospectively collected by local investigators during the admission, using standardised case report forms. Demographics, baseline clinical features, electrocardiographic data and echocardiographic, laboratory and angiographic parameters were collected. GRACE13 and CRUSADE14 risk scores were calculated for each patient. In-hospital clinical outcomes were also registered, such as the need for invasive procedures and in-hospital complications. Major bleeding was defined according to the CRUSADE definition14. An invasive strategy was defined as the performance of coronary angiography during the admission.
BASELINE GERIATRIC ASSESSMENT
This was carried out during admission by trained physicians through interviews with the patient and/or family/caregivers and referring to the patient’s status prior to admission. In order to avoid selection bias, investigators were encouraged to include all patients during the first 72 hours. Geriatric assessment included frailty15, disability16,17, cognitive status18, comorbidity19 and risk of malnutrition20 (Supplementary Appendix 2).
ENDPOINTS
The primary endpoint of this study was the composite of cardiac death, reinfarction or need for unplanned coronary revascularisation at six months of follow-up. The assignment of the cause of death was based on the clinical judgement of the physician taking care of the patient at the time of death. Death was deemed cardiac when it was attributed to myocardial infarction, heart failure or sudden death. Clinical follow-up was carried out by medical visit, review of medical history or telephone contact with the patient, family or referring physician at six months.
ETHICS
All patients or their representatives signed an informed consent before being recruited for the study. Confidential information concerning the patients was protected according to national standards. This manuscript was revised for publication by the Clinical Research Ethics Committee of Bellvitge University Hospital (IRB00005523).
STATISTICAL ANALYSIS
Continuous variables are described either by the mean and standard deviation, or by the median and interquartile range when appropriate. Categorical variables are expressed as number and percentage. Baseline characteristics, clinical management and in-hospital clinical course were compared across groups according to the performance of an invasive strategy. The association between categorical variables was analysed with the chi-square test, with the correction of continuity when indicated. The analysis of quantitative variables according to frailty categories was performed using the Student’s t-test. For non-normally distributed variables this analysis was performed by Mann-Whitney U test.
The association between an invasive strategy and the primary endpoint at six months was assessed by a Fine and Gray competing risks regression model, considering the primary endpoint as dependent variable and non-cardiac death as a competing event. Variables included in the multivariate analysis were those with an association (p<0.1) with both the exposition (invasive strategy) and the effect (the composite of cardiac death, reinfarction or new revascularisation at six months), and not considered to be an intermediate variable between them. Variables included in the multivariate analysis are shown in Supplementary Table 1. Additionally, the association between an invasive strategy and the incidence of the primary endpoint was assessed separately in two groups according to frailty status (non-frail, n=386, and frail, n=145). Survival analysis was performed using Kaplan-Meier curves. Statistical significance of differences was assessed by log-rank test. PASW Statistics, Version 18 (SPSS Inc., Chicago, IL, USA) and Stata v14.1 (StataCorp, College Station, TX, USA) were used for the analyses.
Results
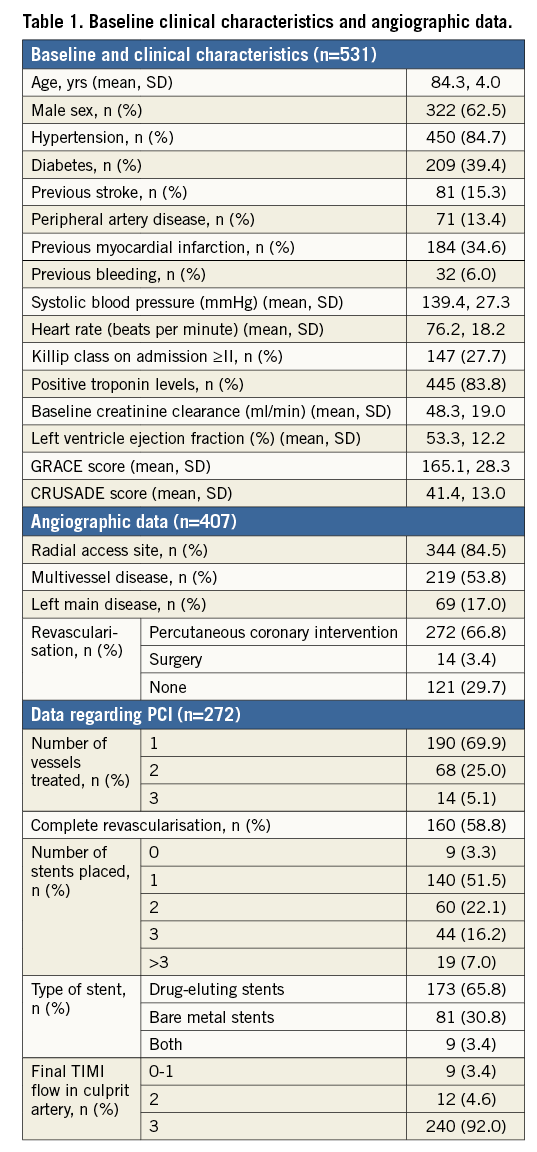
A total of 531 patients were included. Mean age was 84.3 years, and 61.7% were male. Most patients had a high-risk profile, with a high proportion of diabetes mellitus, elevated troponin levels, signs of heart failure on admission, frailty criteria and high mean GRACE score values (Table 1). Most patients underwent an invasive strategy during in-hospital stay (407/531, 76.6%). Cardiac catheterisation was performed by radial access in the majority of patients. Multivessel disease was found in 53.8% of patients, and revascularisation was performed in more than 70% of cases, mostly percutaneous. A complete revascularisation was achieved in 160 patients (58.8%).
CLINICAL CHARACTERISTICS AND IN-HOSPITAL MANAGEMENT ACCORDING TO THE PERFORMANCE OF AN INVASIVE STRATEGY
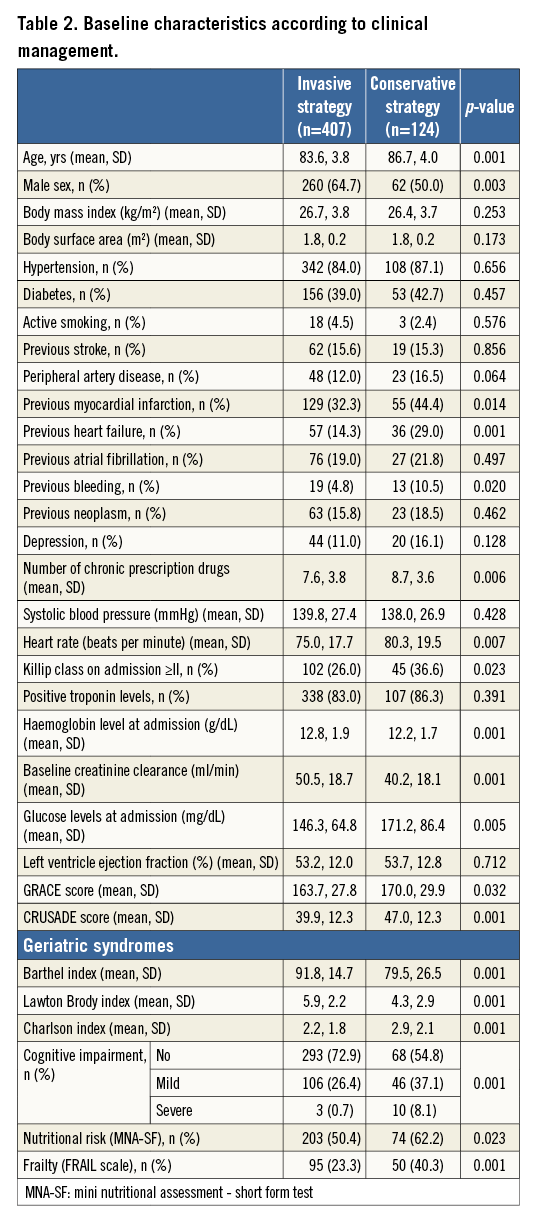
Patients undergoing an invasive strategy were younger, were more often male and had a lower prevalence of comorbidities. They also had lower heart rate, lower Killip class at admission and lower GRACE and CRUSADE score values. Patients undergoing an invasive strategy also had a lower degree of comorbidity, a better functional performance and a lower proportion of cognitive impairment, nutritional risk and frailty (Table 2).
IN-HOSPITAL OUTCOMES
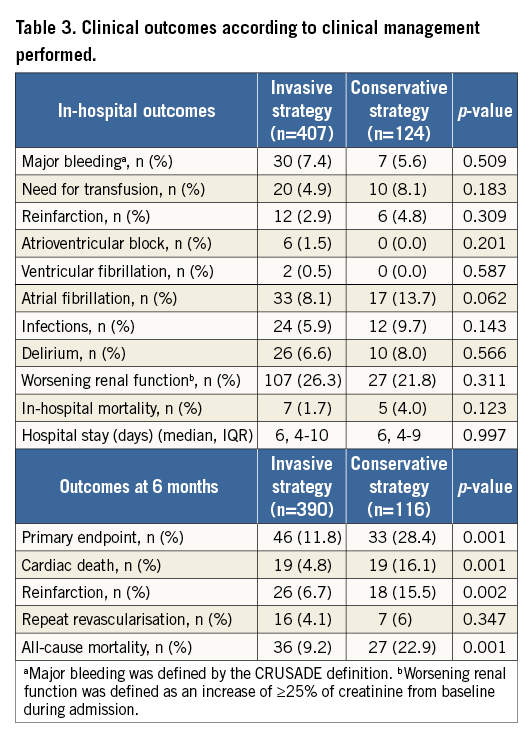
No significant differences regarding in-hospital clinical course were observed between the groups, except for a trend towards a higher incidence of atrial fibrillation in patients managed conservatively (Table 3). The incidence of major bleeding or worsening renal function during admission was not significantly different between the groups.
MANAGEMENT AT HOSPITAL DISCHARGE
Patents managed conservatively were less often treated with clopidogrel and ticagrelor at discharge and less often received dual antiplatelet or triple antithrombotic therapy. The proportion of patients receiving diuretics at discharge was higher in the conservative group. In contrast, fewer patients from this group were treated with statins at hospital discharge (Supplementary Table 2).
POST-DISCHARGE CLINICAL OUTCOMES
Follow-up at six months was obtained in 506/531 patients (95.3%). A total of 79 (14.9%) patients suffered the primary endpoint at six months. The occurrence of the primary endpoint was significantly more common in the non-invasive group (26.6% vs. 11.5%, sub-hazard ratio [sHR] 2.66, 95% confidence interval [CI]: 1.71-4.13, p<0.001).
Patients suffering the primary endpoint were significantly older and had a higher prevalence of diabetes, previous myocardial infarction, previous heart failure and previous bleeding. These patients also had poorer Killip class, lower haemoglobin levels, lower creatinine clearance at admission and poorer left ventricular ejection fraction. In addition, patients presenting events at six months had poorer functional and cognitive status, higher degree of comorbidity and higher prevalence of frailty and risk of malnutrition (Supplementary Table 3).
The association between an invasive strategy and the primary endpoint remained significant after adjusting for potential confounding factors (sHR 2.32, 95% CI: 1.26-4.29, p=0.007) (Supplementary Table 1).
INVASIVE STRATEGY AND OUTCOMES ACCORDING TO THE DEGREE OF FRAILTY
The association between an invasive strategy and the incidence of the primary endpoint was different according to the degree of frailty (Figure 1). In non-frail patients, a conservative management was strongly associated with a higher incidence of the primary endpoint (sHR 3.85, 95% CI: 2.13-6.95, p=0.001). In contrast, no significant association was observed in patients with frailty criteria (sHR 1.40, 95% CI: 0.72-2.75, p=0.325). When the interaction invasive strategy-frailty was included in the model, the effect of an invasive strategy varied among frailty status (p-value for interaction =0.032). Figure 2 shows the cumulative incidence of cardiac death, reinfarction or new revascularisation in non-frail (A) and frail patients (B).
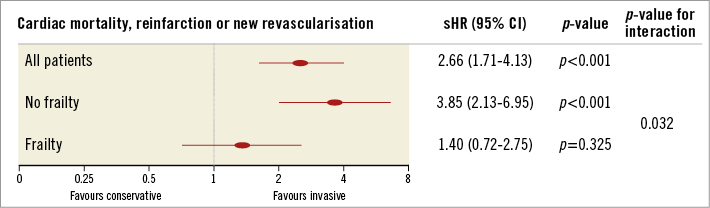
Figure 1. Prognostic effect of an invasive strategy across frailty.
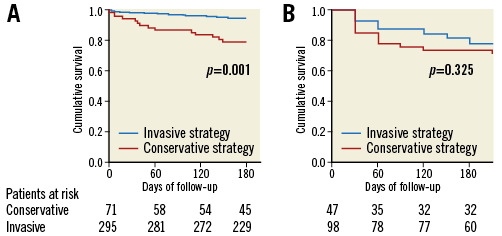
Figure 2. Cumulative incidence of cardiac death, reinfarction or new revascularisation according to the performance of an invasive strategy. A) Non-frail patients. B) Frail patients.
In patients undergoing an invasive management, frailty was associated with a significantly higher incidence of the primary endpoint at six months (sHR 2.82, 95% CI: 1.59-5.01, p=0.001).
Discussion
The main findings from this study are: a) most of these very elderly unselected patients with NSTEACS underwent an invasive strategy during the admission; b) patients undergoing an invasive strategy were younger, with a lower prevalence of comorbidities, frailty and disability; c) an invasive management was associated with better outcomes at six months, and this association remained significant after adjusting for potential confounders; and d) the association between an invasive approach and outcomes was different according to frailty status.
Few randomised clinical trials have addressed the role of an invasive strategy in elderly patients with NSTEACS, showing conflicting results. The Italian ACS Elderly Trial21 included 313 patients ≥75 years of age with NSTEACS, who were randomly allocated to an early invasive strategy or an initially conservative strategy. The primary outcome (the composite of death, myocardial infarction, disabling stroke, and repeat hospital stay for cardiovascular causes or severe bleeding within one year) occurred in 43 patients (27.9%) in the invasive group and 55 (34.6%) in the conservative group (hazard ratio [HR]: 0.80, 95% CI: 0.53 to 1.19; p=0.26). The rates of mortality, myocardial infarction, and repeat hospital stay did not differ between groups.
The After Eighty trial1 included 457 patients aged ≥80 years with NSTEACS from 16 hospitals in Norway. Patients were randomly assigned to an invasive or a conservative strategy. During a median follow-up of 1.53 years, the primary outcome (a composite of myocardial infarction, need for urgent revascularisation, stroke, and death) occurred in 93 (40.6%) of 229 patients assigned to the invasive group and 140 (61.4%) of 228 patients assigned to the conservative group (HR 0.53, p=0.0001). It is important to note that patients included in these two studies were highly selected and had a relatively low prevalence of comorbidities. In fact, the proportion of eligible patients who were finally included was low in both trials (48.5% in the Italian Elderly ACS trial and 10.9% in the After Eighty trial).
More recently, the MOSCA trial2 included 106 patients with NSTEACS aged ≥70 years with a high degree of comorbidity, defined as the presence of at least two of the following: peripheral artery disease, cerebral vascular disease, dementia, chronic pulmonary disease, chronic renal failure or anaemia. Patients were randomised to an invasive (routine coronary angiogram) or conservative (coronary angiogram only if recurrent ischaemia or heart failure) strategy. There were no differences between groups in the rate of all-cause mortality, reinfarction and readmission for cardiac cause at 2.5-year follow-up. Although the invasive strategy tended to improve three-month outcomes in terms of mortality and of mortality or ischaemic events (reinfarction or post-discharge revascularisation), this benefit declined during follow-up.
In our opinion, these different findings might be related to a higher degree of comorbidity in the MOSCA trial. A comprehensive geriatric assessment might have helped to compare these different populations in a better way and to assess the relevance of these results to the general elderly population. During the last decade the assessment of frailty and other variables related to ageing has received growing interest. However, no data about these variables were available in these trials1,2,21. Information about the role of an invasive strategy in elderly patients with NSTEACS according to frailty status is scarce.
Data from our study revealed an association between an invasive strategy and better outcomes at six months. This association remained significant after adjusting for potential confounders. This is an important issue, since these patients have been systematically excluded from clinical trials, and current guidelines recommend carefully assessing comorbidities, frailty and life expectancy before deciding whether to perform an early angiography in this clinical setting. Interestingly, the prognostic impact of an invasive strategy was different according to frailty status, with a lack of association in patients with established frailty. In contrast, a recent study suggests that PCI can improve outcomes in frail patients with NSTEACS7. However, this was a smaller size registry which used different tools for frailty assessment and included only survivors at discharge.
In our opinion, our results might support the hypothesis that in elderly patients with a high degree of frailty the benefit of an invasive strategy might be diluted by the weight of comorbidities, as observed in the MOSCA trial. In any case, larger studies and randomised trials of frail patients with NSTEACS22 are mandatory in order to clarify the role of invasive management in this setting.
Limitations
This study has several limitations. The sample size of subgroups was moderate (especially the group of patients with frailty) and the number of events was relatively small. This was an observational study, so we cannot rule out the presence of selection and confounding bias. We performed this extensive study collecting a lot of clinical and geriatric data in order to minimise residual confounding. However, in the absence of randomised clinical trials including patients with frailty, this should be considered a hypothesis-generating study. In addition, a six-month follow-up may not have been sufficient to detect the impact of an invasive strategy on outcomes fully.
However, we believe that this study adds novel and interesting data about the role of an invasive strategy in non-selected very elderly patients with NSTEACS from routine clinical practice and its association with the degree of frailty in this clinical setting. Refining the risk stratification of these patients could be crucial to improving their quality of life and outcomes, thus potentially contributing to a more rational management of healthcare resources.
Conclusions
An invasive strategy during admission was widely used in this cohort of very elderly unselected patients with NSTEACS. Patients undergoing an invasive strategy were younger, with a lower prevalence of comorbidities, frailty, cognitive impairment and disability. The association between an invasive approach and better outcomes at six months was independent from other important predictors for prognosis, and was different according to frailty status.
| Impact on daily practice Little information exists about the benefit of an invasive strategy in frail elderly patients with NSTEACS. An invasive strategy was independently associated with better outcomes in very elderly patients with NSTEACS. This association was different according to frailty status. An invasive management seems to be useful in non-selected very elderly patients with NSTEACS. Frailty should be assessed in these patients in order to optimise their clinical outcomes. |
Funding
The LONGEVO-SCA project has received a research grant from the Spanish Society of Cardiology.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix 1. LONGEVO-SCA registry investigators.
Supplementary Appendix 2. Baseline geriatric assessment.
Supplementary Table 1. Association between conservative strategy and primary endpoint at 6 months (multivariate analysis).
Supplementary Table 2. Management at hospital discharge.
Supplementary Table 3. Baseline characteristics according to the occurrence of the primary endpoint.
To read the full content of this article, please download the PDF.