Introduction
Prasugrel was proven to be superior to clopidogrel in reducing ischaemic events in the setting of acute coronary syndromes (ACS) but failed to improve outcomes in elderly patients at higher bleeding risk1. Despite the fact that elderly patients often present with increased ischaemic risk2 and a more potent P2Y12 inhibition was suggested to be preferable in terms of longer dual antiplatelet therapy (DAPT) duration3,4 or potent drug use5, evidence supporting the use of prasugrel in this specific subset is lacking. The aim of this paper was to evaluate the impact of high clinical and PCI complexity on the investigational treatment in elderly patients with ACS.
Methods
The Elderly ACS II trial1 (NCT01777503) was a randomised, open-label, blinded endpoint trial carried out at 32 centres in Italy. Eligible patients were >74 years with ST-segment elevation myocardial infarction (STEMI) or non-STEMI (NSTEMI) undergoing PCI during the index admission. Participants were randomised to clopidogrel (75 mg daily) or prasugrel (5 mg once daily). We performed a post hoc subgroup analysis to evaluate the role of coronary atherothrombotic burden as a potential effect modifier of the investigational treatment on the outcomes of interest. We hypothesised that the lack of benefit of low-dose prasugrel observed in the pilot study1 depended on the individual ischaemic burden. The markers explored were: a priori high ischaemic risk profile (defined according to the 2019 ESC guidelines on chronic coronary syndromes as diffuse multivessel coronaropathy and medically treated diabetes mellitus or recurrent MI or peripheral vascular disease or chronic kidney disease) and PCI complexity (defined if ≥3 lesions were treated, if ≥3 stents were deployed, or if any bifurcation, trifurcation, chronic total obstruction or moderate-to-severe calcified lesions were treated)4. The primary endpoint of the analysis was the composite of mortality, MI, disabling stroke and re-hospitalisation for cardiovascular (CV) causes or bleeding. The secondary endpoint was the aggregate of major adverse cardiac events (MACE) including mortality, MI, disabling stroke and re-hospitalisation for CV causes. Safety endpoints were all-cause mortality and any bleeding event. Follow-up was censored at one year.
Results
Of the 1,443 enrolled subjects, 605 (41.9%) underwent complex PCI (Supplementary Table 1) and 1,025 (71.0%) presented with a high ischaemic risk profile; neither of these was associated with worse outcome in terms of the primary endpoint (p=0.21 and p=0.11, respectively) (Supplementary Figure 1). Among those who underwent complex PCI, 309 (51.1%) were randomised to receive low-dose prasugrel and 296 (48.9%) clopidogrel, while 502 (48.9%) of those with a high ischaemic risk profile were randomised to low-dose prasugrel and 523 (51.1%) to clopidogrel. The baseline characteristics were well balanced according to the randomisation arm. Similar rates of the primary endpoint were observed irrespective of the randomisation arm in patients with complex PCI features (low-dose prasugrel arm 19.4% vs clopidogrel arm 16.9%; hazard ratio [HR] 1.14, 95% confidence interval [CI]: 0.8-1.7; p=0.48) and with high ischaemic risk features (18.1% vs 17.2%; HR 1.04, 95% CI: 0.8-1.4; p=0.82). Other results of the survival analysis are shown in Supplementary Table 2. Of note, a tendency towards more bleedings was observed in high ischaemic risk patients receiving low-dose prasugrel (5% vs 2.7%; HR 1.82, 95% CI: 0.95-3.5; p=0.07). Therefore, neither complex PCI nor high ischaemic risk was found to be an effect modifier on the primary endpoint (interaction p=0.34 and 0.68, respectively) (Figure 1). This finding was consistent among secondary and safety endpoints including MACE (interaction p=0.18 and 0.73, respectively), all-cause death (interaction p=0.36 and 0.43, respectively) and bleedings (interaction p=0.76 and 0.26, respectively).
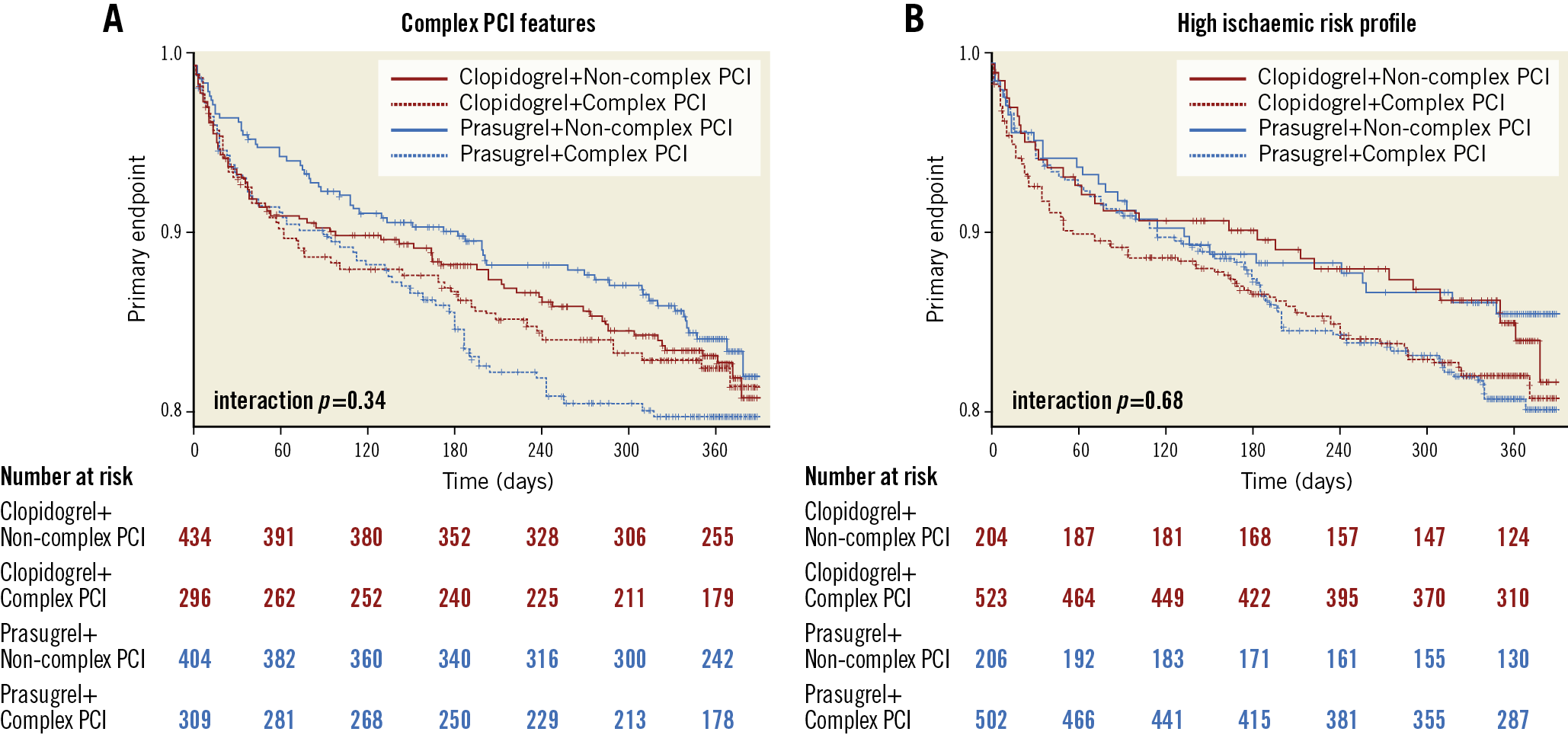
Figure 1. Survival analysis of the primary endpoint at follow-up according to randomisation arm and PCI complexity (A) and ischaemic risk profile (B).
Discussion
The main findings of this study are as follows:
1. In a cohort of elderly patients admitted for ACS, no significant impact of high clinical or PCI complexity was found on clinical endpoints at one year.
2. P2Y12 inhibition with low-dose prasugrel had comparable results versus standard clopidogrel treatment regardless of PCI complexity or of high ischaemic risk.
3. A non-significant trend towards more bleeding was observed with low-dose prasugrel administration when a high coronary atherothrombotic burden was present.
Elderly patients are underrepresented in clinical trials and therefore an age-specific evidence-based clinical strategy is often lacking. Results from the POPULAR-AGE trial showed that full-dose prasugrel and ticagrelor might be associated with similar results in terms of ischaemic endpoints in elderly subjects (Gimbel ME. Randomised comparison of clopidogrel versus ticagrelor or prasugrel in patients of 70 years or older with non-ST-elevation acute coronary syndrome – POPular AGE. Presented at ESC Congress 2019, Paris, France, 31 August 2019) but the relative importance of high ischaemic burden remains unclear in this setting. In the present subgroup analysis, no effect modification of a high ischaemic risk profile or of PCI complexity was found on the administration of investigational treatment. No benefit of low-dose prasugrel versus standard clopidogrel was observed in terms of clinical and ischaemic endpoints in our cohort of elderly patients at high ischaemic risk or in those who underwent complex PCI. Considering the high prevalence of high ischaemic risk profile and complex PCI features in the elderly population, the interpretation of ischaemic risk in the elderly might not be straightforward. First, previous studies stratified the benefit of longer DAPT duration according to ischaemic risk as measured by PCI complexity but without including age for risk adjustment3. As patients with complex PCI features are often older2, this might represent an important confounder; complex PCI may not be appropriate for ischaemic risk stratification in the elderly. Second, considering the prevalence of other inherent comorbidities (such as atrial fibrillation, anaemia, chronic lung disease, renal and liver dysfunction, etc.) in elderly subjects, secondary mechanisms of myocardial ischaemia might play a major role over primary mechanisms of atherothrombosis. This might contribute to blunting the benefit of potent antithrombotic drugs such as prasugrel which still carry a higher likelihood of bleedings. In fact, a non-significant increase in bleeding events was observed in elderly subjects with a high ischaemic risk profile randomised to low-dose prasugrel. Third, our results reinforce the need for appropriate risk stratification in this population which has not yet been addressed by dedicated external validation initiatives. In fact, conditions inherent to ageing put elderly patients at a peculiar bleeding risk, and variables which stratify for high ischaemic risk also identify patients at higher bleeding risk. In conclusion, even if prasugrel might represent an option for elderly patients with ACS and high clinical or PCI complexity, it should be prescribed taking into account the individual bleeding risk profile.
Limitations
First, our study was a non-pre-specified post hoc subgroup analysis. Our neutral results might reflect those of the pilot study. Second, the main trial was interrupted before complete enrolment of patients and might be underpowered to detect differences between smaller subgroups. Therefore, our conclusions should be generalised with caution and are mainly hypothesis-generating.
Conclusions
In elderly patients presenting with ACS and high clinical or PCI complexity, low-dose prasugrel is comparable to clopidogrel but it should be prescribed in the light of the individual bleeding risk profile.
|
Impact on daily practice Low-dose prasugrel is an evidence-based option in elderly patients presenting with acute coronary syndromes and high clinical or PCI complexity. Nonetheless, no benefit was observed versus clopidogrel in terms of clinical outcomes. Higher bleeding risk should be taken into consideration when prescribing low-dose prasugrel. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.