Abstract
Aims: To compare the outcome after primary percutaneous coronary intervention (PPCI) according to sex and age, including comparison of sex- and age-specific mortality of PPCI patients with that of the general population.
Methods and results: This population-based follow-up study included 7,385 STEMI patients treated with PPCI and 42,965 matched general population controls. The primary outcome was the composite endpoint of mortality, reinfarction, and stroke at 30 days, one year, and two years. Women were older and had a more adverse baseline risk profile than men. The risks of the composite endpoint after 30 days, one year, and two years were 9.1%, 16.0%, and 20.0%, respectively, for women compared to 5.8%, 10.6%, and 14.0% for men (adjusted hazard ratio [HR] [30 days]=1.16 [0.95-1.41], adjusted HR [one year]=1.18 [1.02-1.37], and adjusted HR [two years]=1.14 [0.99-1.30]). The risk of an adverse outcome increased similarly among women and men with increasing age. When comparing patients and controls, we found a higher mortality among patients up to 90 days after PPCI. However, after 90 days, the mortality among the PPCI patients was comparable to the mortality in the general population in all sex and age groups.
Conclusions: Clinical outcome after PPCI was comparable in men and women after controlling for possible confounding. After 90 days post-PPCI, the mortality of treated patients was comparable to the mortality of the general population, independent of sex and age.
Introduction
The efficacy of primary percutaneous coronary intervention (PPCI) is documented in a number of randomised controlled trials (RCT) comparing PPCI to thrombolysis in patients with ST-elevation myocardial infarction (STEMI)1. However, women and elderly patients are under-represented in published trials on acute coronary syndromes, which impairs the possibility of translating RCT results into real-world settings2,3. In addition, female and elderly patients eligible for PPCI are less likely to receive the treatment compared to their counterparts4,5. The existing data are conflicting. Some studies report a worse outcome in women compared to men even after adjustment for differences in baseline characteristics4, whereas, no differences are found in other studies6,7. Other studies find the sex-related differences to be age-dependent, suggesting younger women have a particularly adverse prognosis compared to men8. Most studies evaluating age-related differences in outcome after PPCI find elderly patients face a worse prognosis than young patients9. However, none of these studies take into account the higher mortality of elderly people in general. Most of the existing studies lack long-term follow-up, are based on selected populations, or include limited details about patient and treatment characteristics making it difficult to draw more firm conclusions. Thus, the effectiveness and safety of PPCI in women and elderly patients are insufficiently described.
We, therefore, conducted a follow-up study comparing the patient and treatment characteristics, as well as short- and long-term outcome, after PPCI according to sex and age in unselected real-world patients. Further, to indirectly measure effectiveness and safety, we compared the survival of PPCI treated STEMI patients with survival in the general population across sex and age groups, which, to our knowledge, has not been done before.
Methods
We completed a population-based historical follow-up study in Western Denmark with approximately 3.3 million inhabitants (56% of the Danish population). The National Health Service provides tax-supported healthcare, guaranteeing unfettered access to medical care. All acute medical conditions are exclusively treated at public hospitals in Denmark. The Danish Civil Registration System keeps records of sex, date of birth, and vital status. The records carry a 10-digit civil registration number assigned to every Danish citizen and used in all Danish registers, enabling unambiguous record linkage between them.
IDENTIFICATION OF PATIENTS
The Western Denmark Heart Registry (WDHR) collects detailed data related to patients and procedures for all interventions carried out in the three coronary intervention centres of Western Denmark (Odense University Hospital, Aarhus University Hospital [Skejby], and Aarhus University Hospital [Aalborg]). Reporting to the registry is mandatory and data quality is ensured by automatic validation rules at data entry combined with systematic validation procedures and random spot-checks of data after entry10. We identified all Danish STEMI patients from 2002-2008 who underwent PPCI within 12 hours of symptom onset (n=7,385). Each patient was matched by sex, year of birth, and level of comorbidity with up to 10 individuals from the general population who were alive on the date of the associated patient’s PPCI. These controls were sampled using the Danish Civil Registration system. The total number of controls was 42,965. The median number of controls was five and 520 patients did not have a control.
PATIENT CHARACTERISTICS AND TREATMENT
We obtained data regarding hypertension, a family history of coronary heart disease, smoking, Killip class, duration of symptoms, and all procedure-related data from the WDHR. Duration of symptoms was defined as time from symptom onset to guiding catheter insertion during PPCI because time of balloon inflation was only available in a minority of patients and only a few minutes elapse from guiding catheter insertion to first intervention. Whether the procedure was successful was assessed by the treating physician. In-lab complications included contrast reactions, coronary artery perforation, tamponade, acute coronary artery bypass graft/percutaneous coronary intervention (CABG/PCI), and arrhythmias.
The Danish National Patient Registry collects data for all hospitalisations at Danish hospitals, including dates of admission and discharge, and discharge diagnoses assigned by the treating physician and coded according to the International Classification of Diseases, 10th revision (ICD-10) since 1993. Based on the last 10 years of hospitalisation history for each patient and control, we computed the Charlson comorbidity index score11, which was adapted for use with hospital discharge registry data12. We defined three levels of comorbidity: a score of 0 (“low”); a score of 1-2 (“moderate comorbidity”); and a score >2 (“high comorbidity”).
The Integrated Database for Labour Market Research at Statistics Denmark contains information about the Danish population and their affiliation with the labour market. Information about marital status and other socio-economic factors were ascertained here.
The Danish Transfusion Database is a national registry monitoring the use of all blood components. We obtained information regarding the types and number of blood components administered from the day of admission to seven days post admission.
We obtained data regarding the use of cardiovascular drugs from the Danish Medicines Agency’s Register of Medicinal Product Statistics, a national prescription registry that contains information on all redeemed prescriptions for reimbursable drugs dispensed from all pharmacies in Denmark. The information includes type of drug (according to the Anatomic Therapeutic Chemical classification system) and the date dispensed. We identified all prescriptions for aspirin, clopidogrel, nitroglycerine, statins, angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, and selective and non-selective β-blockers filled from hospital discharge until the end of follow-up. All the drugs were available only by prescription, except for aspirin. However, aspirin is available by prescription, and patients with chronic diseases and pensioners are reimbursed for it.
For a subset of the patients (n=4,856), data from the Laboratory Information Systems in Central and North Denmark regions were obtained, including data regarding haemoglobin, total cholesterol, troponin T, creatine kinase-myocardial band (CK-MB), and blood glucose levels. The highest value measured over seven days, starting from the time of admission, was obtained except for haemoglobin where the lowest value was obtained. We calculated the estimated glomerular filtration rate (eGFR) using the four-component modification of diet in renal disease (MDRD) equation incorporating age, race, sex, and serum creatinine level13. Race was not included because Denmark has a primarily Caucasian population and race data were unavailable. Based on haemoglobin values, we classified anaemia as no anaemia (>8.4 mmol/L), borderline (≤8.4 mmol/L to >7.8 mmol/L), mild (≤7.8 mmol/L to >6.5 mmol/L), moderate (≤6.5 mmol/L to >5.3 mmol/L), and severe (≤5.3 mmol/L) for men, and the same categories for women with all intervals starting and ending 1 mmol/l below the corresponding intervals for men.
CLINICAL OUTCOMES
The primary endpoint was a composite endpoint of all-cause mortality, reinfarction (ICD-10 I21), and stroke (ICD-10 I61, I63-64) at 30 days, one year, and two years. We defined a reinfarction as hospitalisation for myocardial infarction occurring >28 days after the index PCI14. Thus, the composite endpoint at 30 days consisted of death and stroke on day 0-30 and reinfarction on day 28-30. Data on reinfarction and stroke were obtained from the National Patient Registry (data available until the end of 2009), and deaths were ascertained from The Danish Civil Registration System (data available until the end of 2010).
STATISTICAL ANALYSES
The patients were censored at the time of death or followed up for two years. We compared baseline characteristics using the Student’s t-test for continuous variables and the χ2-test for categorical variables. We used the Cox proportional hazards regression model to compute crude and adjusted hazard ratios (HR) and 95% confidence intervals (CI) for the endpoints. The patients were divided into three age groups (<65 years, 65-80 years, and >80 years). The male patients and the youngest age group served as the reference in all analyses and all tests of significance were two-tailed with p<0.05 considered statistically significant. The hazards were not proportional throughout the follow-up period when comparing patients and general population controls; therefore, we estimated the HR within the periods during which the proportionality assumption held in these analyses (i.e., 0-90 days and >90 days-2 years); and we used a Cox model with delayed entry using age as the time scale. The general population controls served as the reference. We also did the analyses using conditional Cox regression to see if survival bias was present. This did not change the estimates.
The number of patients with complete data for all variables was 2,408 (33%). For most of the variables, only a minor proportion of the patients had missing data (0.0%-13%); however, 23% to 40% of patients had missing data for the laboratory data, smoking status, family history of ischaemic heart disease, history of hypertension, and hypercholesterolaemia. We used multiple imputation to impute missing values for all variables. Besides all measured variables, we included the event indicator and the Nelson-Aalen estimator of the cumulative hazard to the survival time in the imputation model15. Analyses were conducted on five imputed datasets and the results combined using Rubin’s rules16.
Sex, age, comorbidity, and duration of symptoms were forced into all of the multivariable analyses. To optimise the precision of the risk estimate, we used the change-in-estimate method when selecting additional covariates to be included.17 Using this method, covariates were selected based on a relative change of more than 10% in the estimated exposure effect. The eGFR and grade of anaemia were in this way identified as possible confounding factors and consequently also included in the final multivariable model. When comparing patients and general population controls, we adjusted for comorbidity as a continuous variable to reduce residual confounding.
We analysed data using Stata version 11.0 (StataCorp, College Station, TX, USA) software. Our study was approved by the Danish Data Protection Agency (journal number 2008;41-1835).
Results
PATIENT AND TREATMENT CHARACTERISTICS
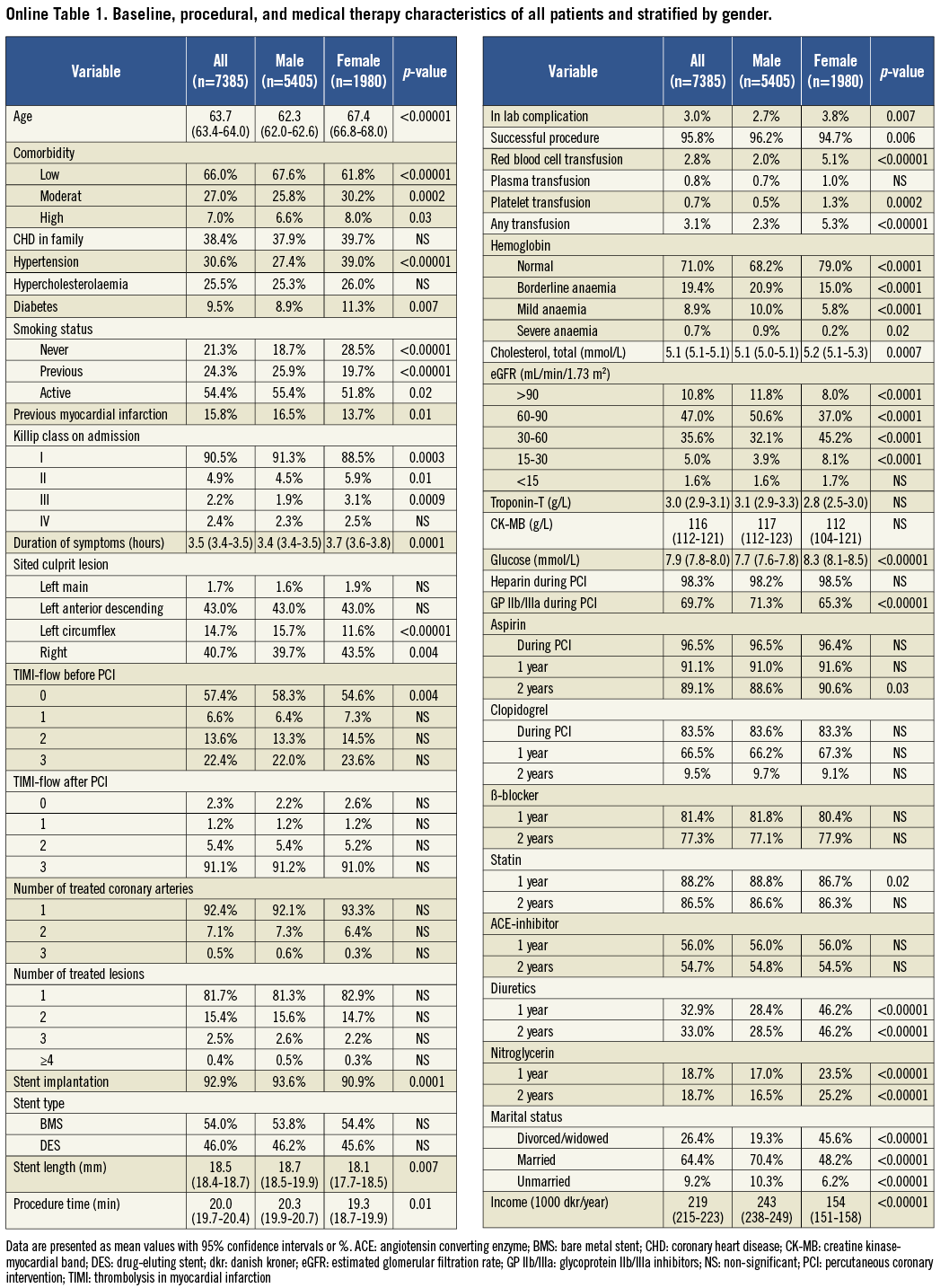
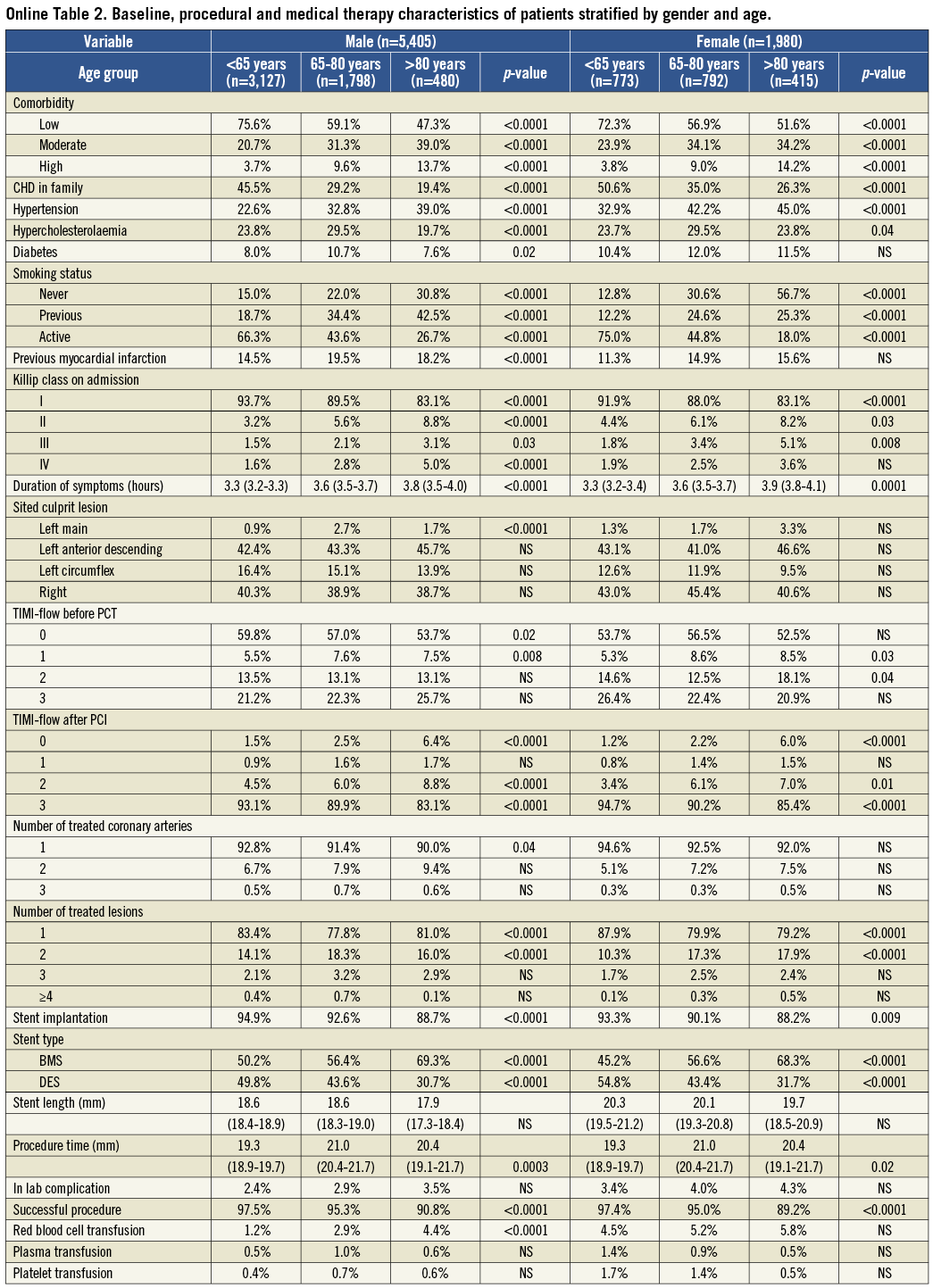
Compared to men overall, women were older, had more comorbidities, a longer duration of symptoms, and a higher Killip class. More women had a family history of coronary heart disease; whereas, fewer women were smokers or previous smokers or had previous myocardial infarctions. Compared to men, women had shorter mean stent lengths and procedure times, fewer women had a stent implanted, women had a higher incidence of in-lab complications, and more women received red blood cell and platelet transfusions. Women had lower troponin T and eGFR levels and a lower prevalence of anaemia than men; whereas, total cholesterol and blood glucose levels were higher compared with men. When comparing medical treatments that occurred during PPCI and one and two years afterwards, there were no differences between men and women except that diuretics and nitroglycerine were used more frequently among women and fewer women received a glycoprotein IIb/IIIa inhibitor during PPCI. Compared to men, women were less likely to be married and had a lower income. After stratifying by age, the same differences were present in the young and middle age groups except that no differences in comorbidity, procedure times, and levels of troponin T and total cholesterol were found. In the old age group, the only differences were a more frequent use of diuretics after one and two years, a lower prevalence of anaemia and previous and active smokers among women than men (Online Table 1 and Online Table 2).
CLINICAL OUTCOME AMONG PPCI PATIENTS
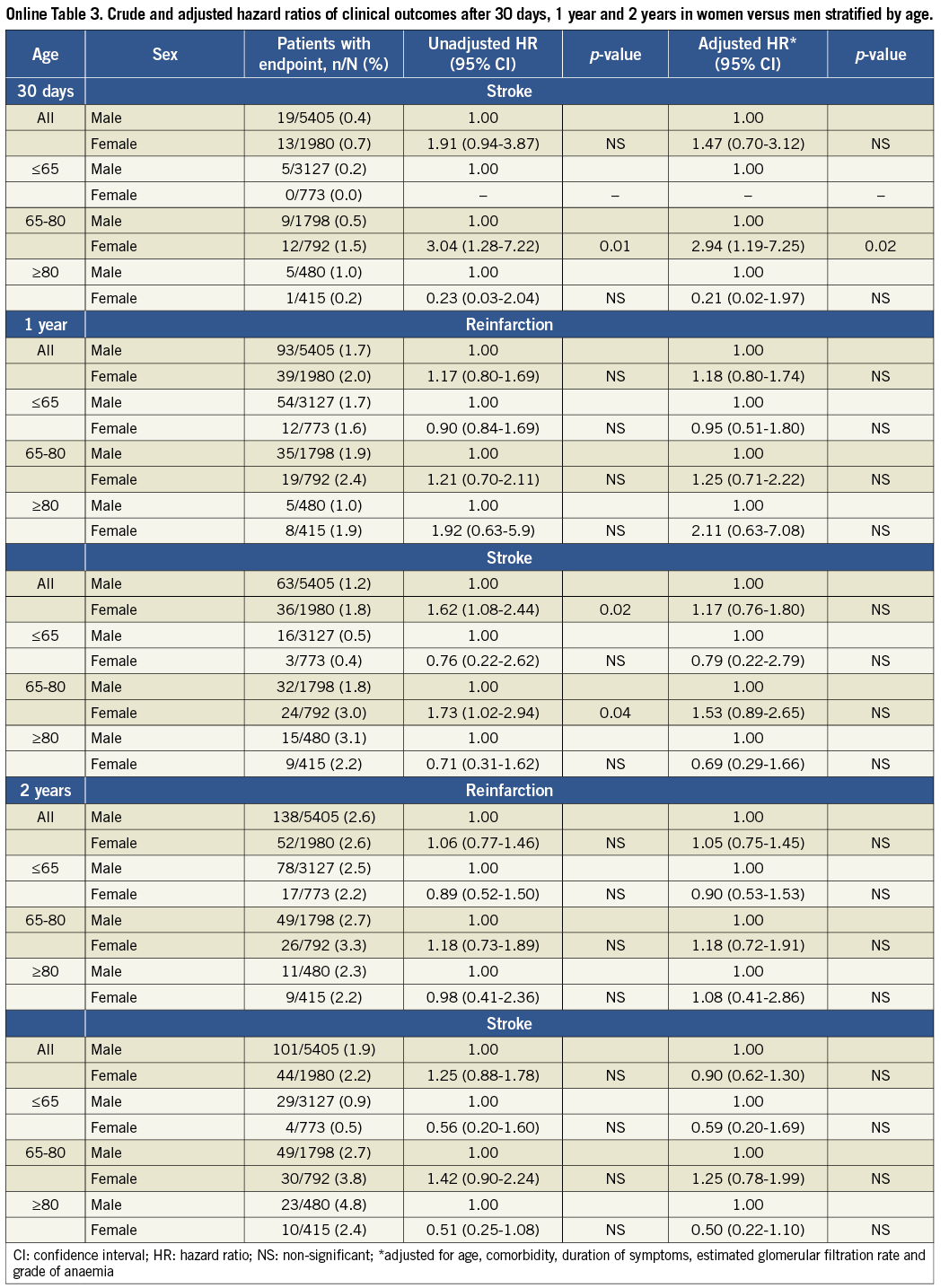
Table 1 presents the composite endpoint and cumulative mortality after 30 days, one year, and two years stratified by sex and age. Without stratifying by age, women had a higher cumulative risk of the composite endpoint and a higher mortality than men. However, after adjustment for possible confounding factors (sex, age, comorbidity, duration of symptoms, eGFR and grade of anaemia), only the difference in the cumulative risk of the composite endpoint after one year remained statistically significant. Among patients aged 65-80 years, women had a higher cumulative risk of the composite endpoint than men after one and two years. After adjustment, there were no differences between men and women in this age group. There were no differences between men and women in the other age groups in the crude or adjusted estimates.
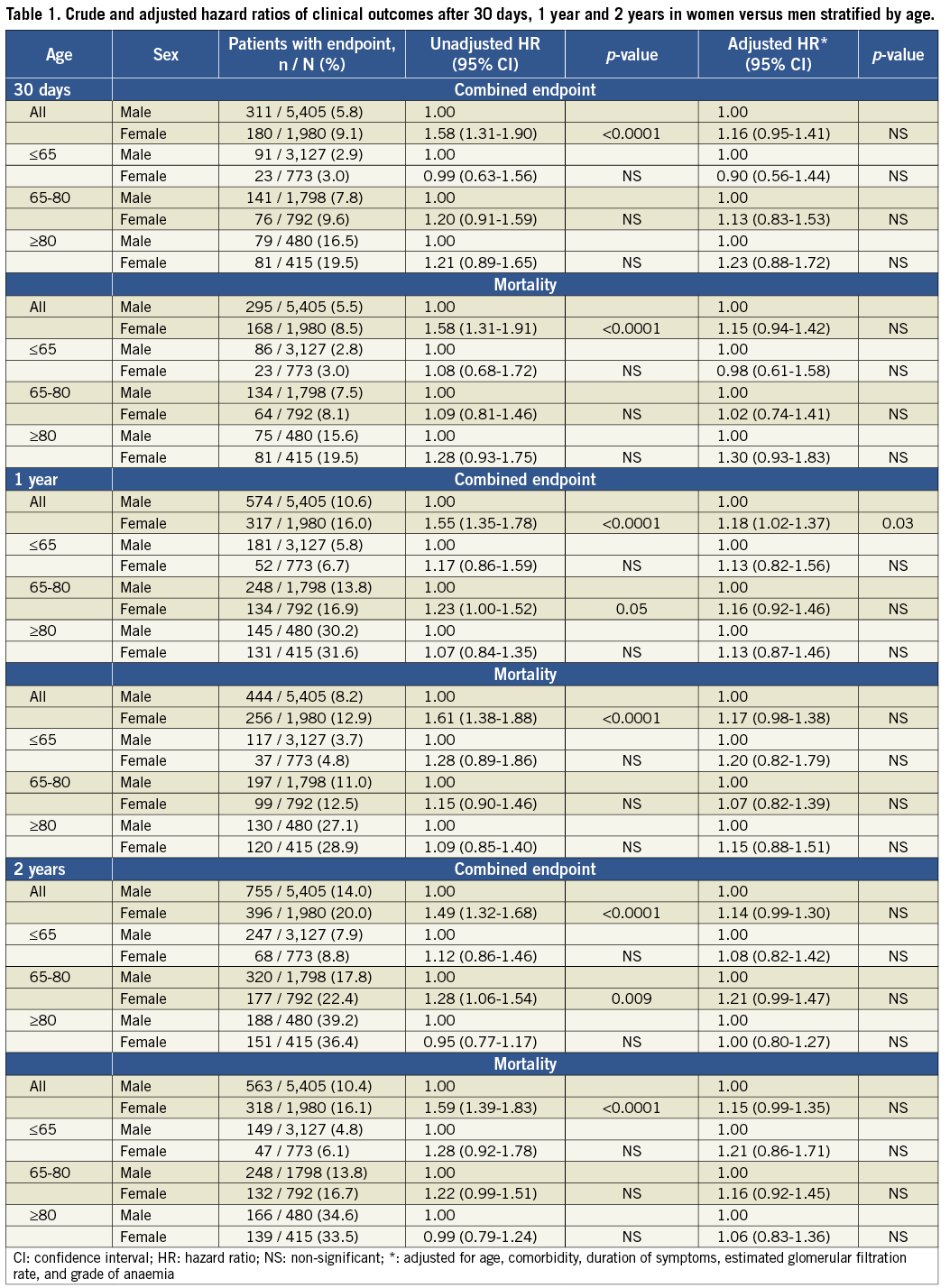
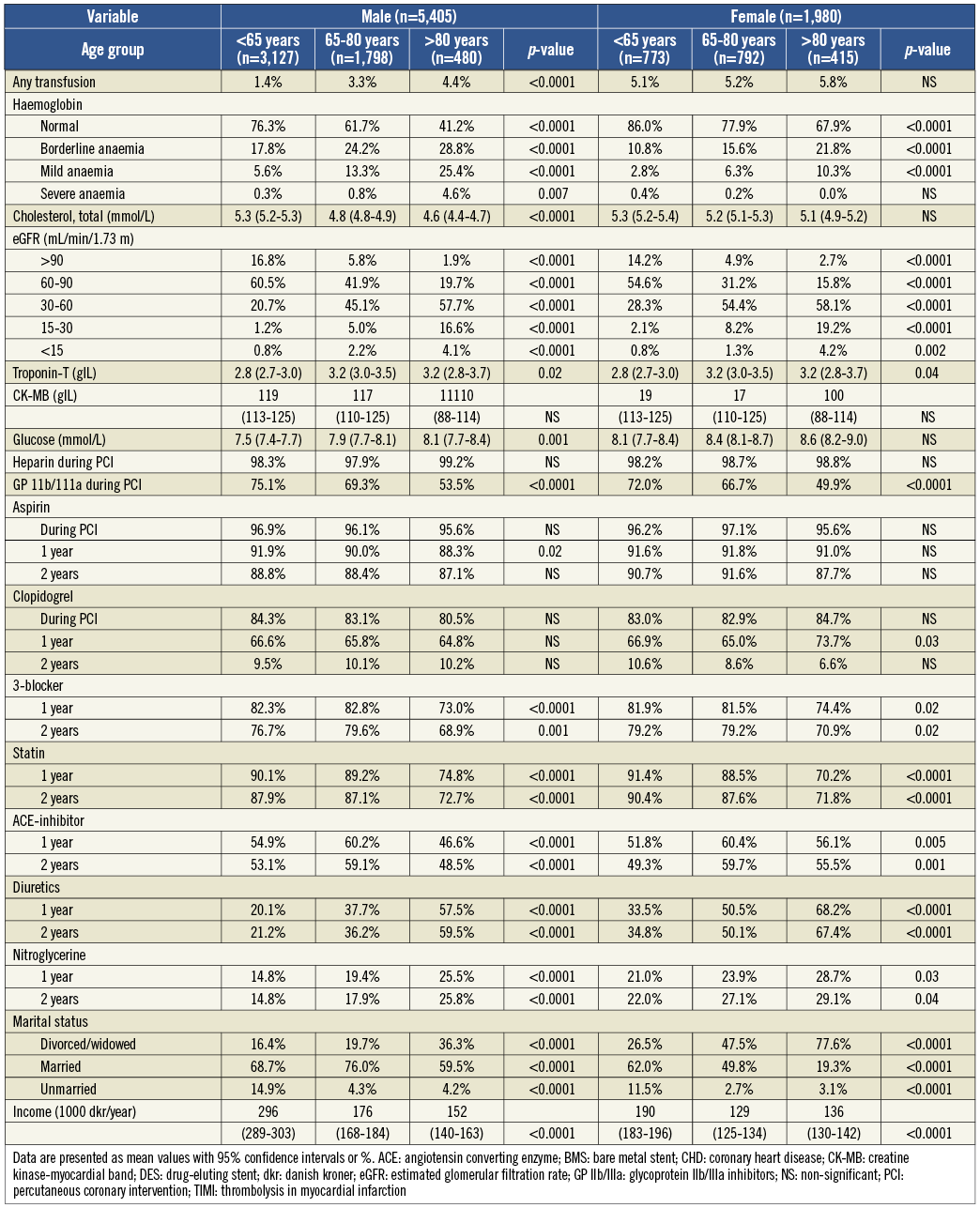
No differences were found in the cumulative risk of reinfarction or stroke, except that women had a higher cumulative risk of stroke after 30 days compared to men. However, this finding was based on very few outcomes (Online Table 3).
COMPARISON WITH THE GENERAL POPULATION
Table 2 and Figure 1 present mortality rates and cumulative mortality curves of the PPCI patients and sex, age and comorbidity matched general population controls stratified by sex and age. For both sexes the 90-day mortality rate was significantly higher among patients than controls in all age groups. The mortality rates were highest among women and older patients compared to men and younger patients. The adjusted mortality rate ratios during the first 90 days were higher for women compared to men except for the old age group, although the differences were not statistically significant. For both men and women, the adjusted mortality rate ratios were highest in younger patients and lowest in older patients. After 90 days, there were no differences in the mortality rates compared with the general population, except for a higher mortality rate among the youngest women. (For demographic information on patients and controls, Online Table 4).
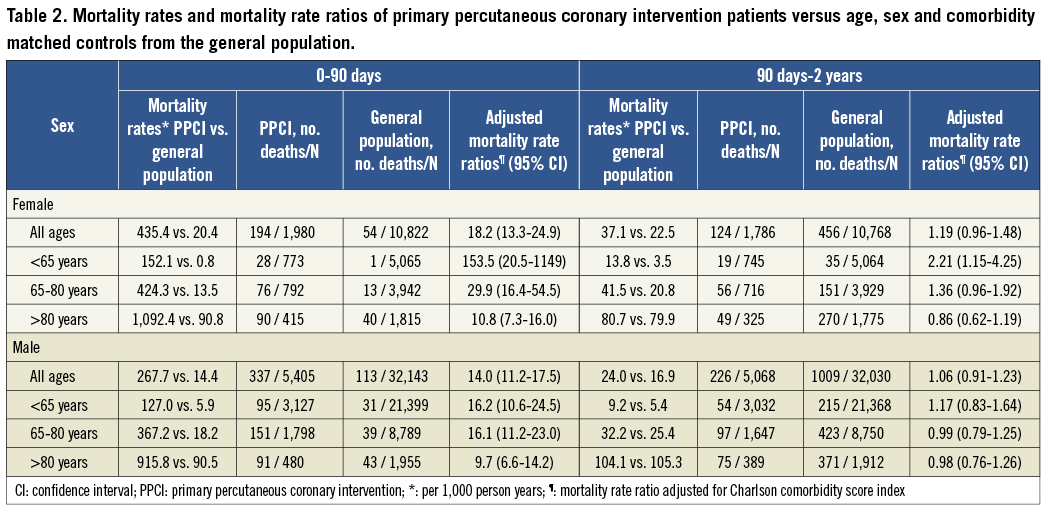
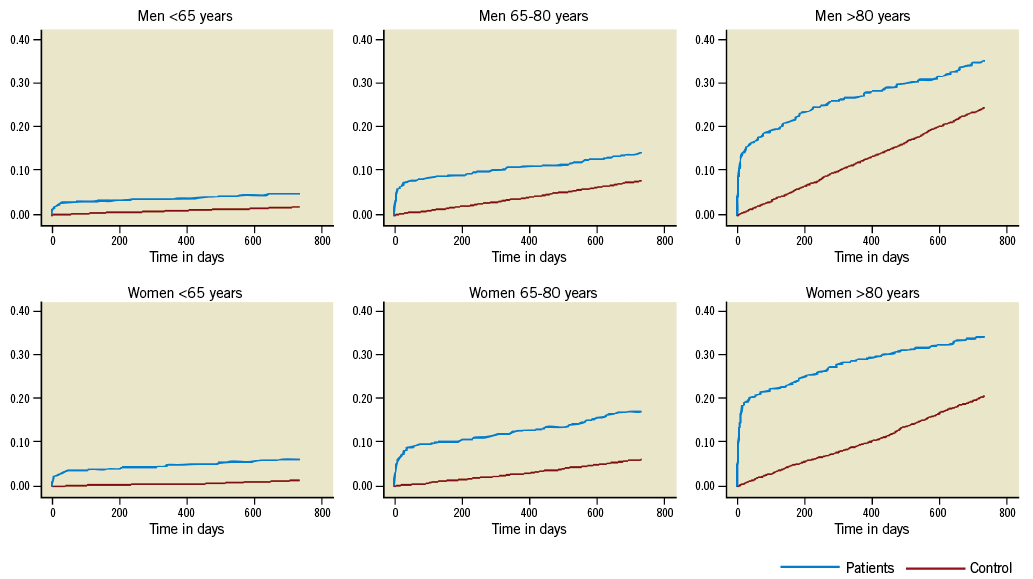
Figure 1. Kaplan-Meier curves of the cumulative mortality in PPCI patients and controls stratified by sex and age. PPCI: primary percutaneous coronary intervention
Discussion
The present study shows that women presenting with STEMI and treated with PPCI had adjusted short- and long-term outcomes similar to men. Women were older and overall had a more adverse baseline risk profile than men, which explained their higher risk in some of the crude and non-stratified analyses. There were no substantial differences in the medical treatments received during the PPCI procedure or after discharge.
We found a higher mortality among patients up to 90 days after admission for STEMI when comparing mortality between patients and general population controls. This difference was present in both men and women of all ages, but the mortality rates were highest among women and older patients compared to men and younger patients. The adjusted mortality rate ratios during the first 90 days were highest in younger patients and lowest in older patients. After 90 days the mortality among the PPCI patients dropped to a level comparable with the mortality in the background population.
Women in the present study had a higher baseline risk than men and we saw no differences in adjusted outcomes between men and women, which is consistent with previous STEMI studies5-7,18. However, few studies have previously focused on PPCI-treated STEMI patients6,7,18, and these studies have included relatively few patients, with a maximum follow-up period of one year.
In contrast to our results, other studies found a worse prognosis among women compared to men, even after adjustments4,8,19. Few of these studies focused on PPCI-treated STEMI patients19. Furthermore, the patient populations have in general been relatively small, with short follow-up periods and limited information available on patient and treatment characteristics, especially information on medical treatments used during follow-up. Thus, it is not clear whether the reported differences are related to sex or caused by differences in medical treatments used during follow-up, since several studies of myocardial infarction have reported that men more often than women receive guideline-recommended medical treatments at discharge4,5. In our study population, we found no differences in the use of heparin, aspirin, and clopidogrel during the PPCI procedure or in the use of guideline-recommended medical treatments after one and two years. Women used diuretics and nitroglycerine more often than men. Some previous studies found an interaction between sex and age, with a worse prognosis among women compared to men in younger age groups and no differences between men and women in older age groups8. We could not confirm the existence of such an interaction.
To our knowledge, no previous study has compared the mortality of a PPCI-treated STEMI population with the mortality of the corresponding background population. Launbjerg et al20 found the annual mortality to be twice as high in patients with myocardial infarction compared to the corresponding background population for up to 10 years. In contrast, we only found the overall mortality to be higher in our STEMI population compared to the background population during the first 90 days. The adjusted mortality rate ratios were highest in younger patients compared to older patients for both men and women. Thus, even in the acute phase, there is no excess relative mortality among older patients compared to younger patients. After 90 days we found no difference in mortality between the two populations, except for a higher mortality in the youngest women. This difference was caused by very few deaths due to the low mortality in the general population controls. This indicates that men and women of all ages benefit from PPCI to the same degree.
Study strengths and limitations
The main strengths of our study are the large number of patients, the long follow-up period, the prospective, population-based design, and the possibility of unambiguous individual-level linkage between public data sources, which provided detailed information on patient characteristics, treatments, and use of medications, and allowed complete follow-up, minimising the risk of selection bias. The Danish Civil Registration System and the Danish National Patient Registry made it possible to identify matched controls from the background population, which is unique.
Some previous study populations come from databases based on RCT19. This may cause problems with the external validity of these studies because of the strict inclusion and exclusion criteria in the RCT and the potential exclusion of more women than men, as more women than men present with shock or hypotension6-8, which are characteristics that often lead to exclusion from trials. Thrombolysis is still widely used in most countries. It is unclear what factors are used to determine whether thrombolysis or PPCI is used. If these factors are different between men and women, as some studies indicate4, it may cause bias. Our study was carried out in Denmark, where PPCI is the standard treatment of STEMI. Thus, STEMI patients are almost exclusively treated with PPCI, optimising the external validity and minimising the risk of bias, since the WDHR contains data on all procedures without any inclusion or exclusion criteria. This also means that our study population is different from most other registry study populations and a direct comparison of patient characteristics might be problematic. However, it might explain why our study population has a better baseline risk-profile compared to other registry studies6-8. This is the case for both women and men of all ages, and thus we have no reason to believe that it had any substantial influence on the relative risk estimates.
We used hospital discharge diagnoses, which may not always be accurate. However, the validity of the diagnoses included in this study were high (e.g., misclassification occurring in approximately 20% of cases)21,22. We controlled for a wide range of factors possibly affecting outcome; yet, due to the observational study design, we cannot exclude the possibility that confounding factors still influenced the results, factors for which information was not available, including lifestyle habits and patient compliance.
Conclusion
Clinical outcome after PPCI was comparable in men and women after controlling for differences in baseline risk profiles. After 90 days post-PPCI, the mortality rates of PPCI-treated patients were comparable to the mortality of the general population independent of sex and age.
Acknowledgements
This work was supported by the Danish Heart Foundation (grant numbers 07-10-R60-A1633-B597-22410 and 10-04-R78-A2784-22593), the Western Danish Research Forum for Health Sciences, and the Central Denmark Research Foundation.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Table 1. Baseline, procedural, and medical therapy characteristics of all patients and stratified by gender.
Table 2. Baseline, procedural and medical therapy characteristics of patients stratified by gender and age.
Table 3. Crude and adjusted hazard ratios of clinical outcomes after 30 days, 1 year and 2 years in women versus men stratified by age.
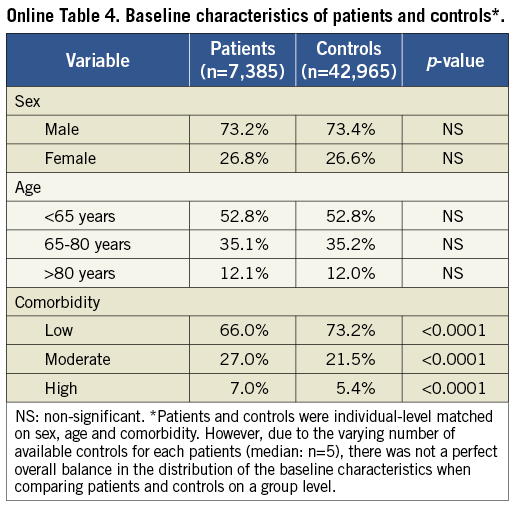
Table 4. Baseline characteristics of patients and controls.