Abstract
Aims: Clinical outcomes in the treatment of acute ST-segment elevation myocardial infarction (STEMI) differ between men and women. The aim of the study was to compare results of STEMI management in a large multicentre national registry.
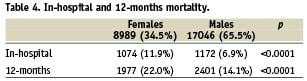
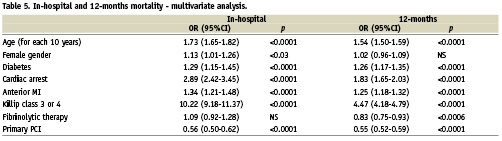
Methods and results: A total of 456 hospitals (including 58 interventional centres) participated in the registry during one year. The study group consisted of 8,989 (34.5%) females and 17,046 (65.5%) males. Women were older (69.7±11 vs. 62±12 years; p<0.0001) and had more risk factors. Percutaneous coronary intervention was performed significantly less in women (47.8% vs. 57.4%; p<0.0001). There was a longer time delay in women at each stage of treatment. The incidence of in-hospital complications was higher in women. In-hospital (11.9% vs. 6.9%; p<0.0001) and 12-months (22% vs. 14.1%; p<0.0001) mortality was significantly higher in women. In multivariate analysis pulmonary oedema, cardiogenic shock, cardiac arrest, age, diabetes and anterior infarction significantly increased both in-hospital and long-term mortality. The in-hospital mortality was higher in the female group.
Conclusions: Despite poor clinical characteristics, less than satisfactory management and a worse prognosis of STEMI in women, being a women itself is not a risk factor for increased long-term mortality, however, other well known risk factors affecting the prognosis relate frequently to the female gender.
Introduction
Despite wide recommendation of guidelines1 on management of ST-segment elevation myocardial infarction (STEMI) and well organised network of high-volume percutaneous coronary intervention (PCI) centres, STEMI is still one of the main causes of death in Poland. Gender-related differences in management of acute coronary syndromes have been discussed for many years. Especially in the nineties, when the term “the Yentl syndrome” appeared2, there existed a conviction that women were treated in the same manner as men only if acute myocardial infarction was the cause of the disease. Since then, many clinical trials with an increasing number of women included were conducted, many of them with conflicting results but introducing some possible causes for the poor clinical outcome after STEMI in women, e.g., risk factors, comorbidities, less aggressive pharmacotherapy, advanced age, etc. The specificity of randomised controlled trials results in a high-percentage of low-risk profile patients included and in the exclusion of women with child bearing potential3,4. The unique strength of this registry is that it reflects the management of all consecutive STEMI patients in our country who searched for any medical help.
Methods
The principles of our registry (the largest acute coronary syndrome registry in Europe) have been reported previously5 and are available on-line6. A total of 26,035 consecutive patients (8,989 females and 17,046 males) with STEMI diagnosed according to current guidelines7 were included during one year (June 2005 - May 2006). The data collected were age, gender, concomitant diseases, coronary risk factors, previous myocardial infarction and revascularisation, time from symptom onset to PCI, type of hospital facility (on-site PCI or transport from another site), time from symptom onset and from admission to PCI, extent of the disease in angiography, TIMI flow before and after revascularisation, adjunctive treatment, left ventricular ejection fraction (LVEF), cardiovascular, neurological and haemorrhagic complications and discharge medication. Bleeding complications were assessed according to TIMI classification8. Mortality data (in-hospital and one year follow-up) after hospital discharge were obtained from the National Health Fund and Civil Registry database and were collected for all included subjects.
Statistical analysis
Continuous variables are expressed as mean±standard deviation or median and interquartile range. The significance of differences between groups was determined by use of Student’s t test or the Mann-Whitney U test for those variables which did not conform to a normal distribution. Homogeneity of variances was tested using the F test. Categorical variables were tested using the chi-square test. Mortality at 12 months was analysed using Kaplan-Meier method with log-rank test. A p value ≤0.05 was considered significant.
Results
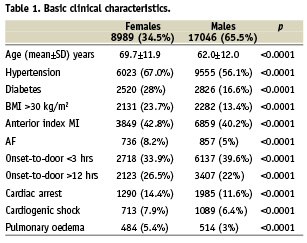
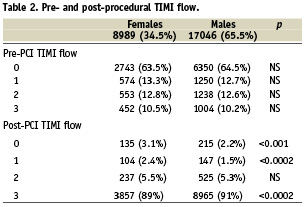
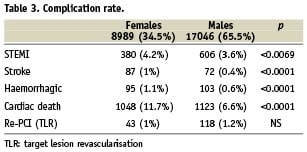
Women were significantly older than men (69.7±11,9 vs. 62.0±12 years; p<0,0001). Known cardiovascular risk factors, i.e., hypertension, diabetes and obesity and worse clinical presentation (anterior MI, atrial fibrillation, cardiac arrest, cardiogenic shock and pulmonary oedema) appeared significantly more frequently in women (Table 1). Coronary angiography was performed in 15,286 (58,7%) patients, significantly less in women (52.4% vs. 62.1%; p< 0.0001) as well as primary PCI (47.8% vs. 57.4%; p<0.0001). Moreover, fewer women than men underwent primary PCI earlier than 12 hours from symptoms onset (35.8% vs. 44.0%; p<0,0001). There was a significant difference in aspirin (92.2% vs. 93.4%; p=0.0002), clopidogrel (51% vs. 59.2%; p<0.0001), unfractionated heparin (36.5% vs. 41.5%; p<0.0001) and glycoprotein IIb/IIIa inhibitors (12.2% vs. 16.8%; p<0.0001) administration in favour of men. Single vessel disease was more frequent in women (45.1% vs. 43%; p<0.02), whereas the difference in the prevalence of multivessel disease between genders was insignificant (22.8% vs. 23%). Onset-to-balloon time in primary PCI was also significantly longer in women (255 [175-375] vs. 241 [165-360] min; p<0.0001), as well as door-to-balloon time (45 [30-70] vs. 44 [30-68] min; p=0.032). Primary PCI was performed in patients who presented directly to PCI capable centres or were transported from another site (45% vs. 55% of all PCIs; p<0.0001). No significant differences in basic clinical characteristics between these two groups were observed. However, onset-to-balloon time was significantly longer both in women and in men transported from a non-PCI facility than in those who presented directly to a PCI centre. In both groups onset-to-balloon time was significantly longer in women (direct transport: 231 vs. 220 min, p=0.0081; transport from another site: 272 vs. 260 min, p=0.0009). The success rate in primary PCI was lower in women, TIMI 0 and 1 grade flow after PCI were more frequent, whereas TIMI 3 grade flow significantly less frequent in women (Table 2). These results were similar in patients presented directly to PCI centres and in those referred from another site with no significant differences in distribution of pre- and post-procedural TIMI flow grades between groups. The complication rate was also higher in women, with excessively high bleeding rate in women (1.1% vs. 0.6%; p<0.0001) (Table 3). Women were less likely to receive modern pharmacotherapy with significantly lower frequency of administration of clopidogrel (28.1% vs. 33.5%; p<0.0001), beta blockers (73.3% vs. 74.9%; p=0.007) and statins (79% vs. 80.9%; p=0.0005) at discharge when compared to men. During follow-up, we were able to collect data with respect to all deaths. Mortality rate was significantly higher in women, both in in-hospital and 12-months observation (Table 4). In multivariate analysis age, diabetes, cardiac arrest, anterior MI, Killip class 3 or 4 were independent factors of increased mortality in short- and long-term follow-up. Moreover, the female gender affected in-hospital, but not 12-months mortality (Table 5). When analysing mortality trends in men transported from a non-PCI site and those who presented directly to a PCI centre there was no significant differences, however, in 12-months of observation there was a non-significant tendency for higher mortality in women transported from another hospital (12.3% vs. 10.3%; p=0.08).
Discussion
Gender-related differences in patients with acute coronary syndromes has become one of the most interesting topics of cardiology congresses in the last decade. Some investigators ascribe higher mortality among women to a worse risk profile and less aggressive treatment strategy9-11, others believe that the female gender is an independent predictor of adverse outcome12,13. It is also well-known that women are more prone to complications related to invasive procedures14. Much emphasis is put on exploring the reasons for discrepancy between the management of STEMI in men and women, however women are still poorly represented in randomised controlled trials, and the results are not reported in the context of gender. The unique strength of our report is that the population has not been selected in any way and the results reflect the management in all consecutive patients with respect to gender-related differences.
Basic clinical characteristics of women with STEMI was similar to those reported in other registries. In general, women were older and had more cardiovascular risk factors and comorbidities than men, which is consistent with other reports15-21.
The benefit of early reperfusion in STEMI is now unquestionable, as infarct size is correlated with duration of coronary artery occlusion. De Luca has demonstrated that every 30 min delay of revascularisation will increase annual mortality by 7.5%22. In contrast, in the NRMI-2 (National Registry of Myocardial Infarction) and GRACE (Global Registry of Acute Coronary Events) registries reperfusion therapy was not offered to 30% of STEMI patients without any contraindication to such treatment23,24. In our study, a percentage of 31.5% in the conservative approach in men corresponds to this, however, more than 40% of women without reperfusion raises a concern that compliance with current guidelines is not sufficient. The analysis of invasive or fibrinolytic therapy is not optimistic either, as it was less effective in women at each stage. Primary PCI was performed less frequently in women and even if performed, the percentage of women treated earlier than 12 hours from the symptom onset was significantly lower. To explain this, it should be emphasised that women presented later than men and that prolongation of time to treatment was mainly due to onset-to-door time, while door-to-balloon time differed slightly, but significantly, in favour of men. This confirms findings by DeLuca et al that every minute of delay counts22.
The multivessel disease (MVD) incidence in patients with acute coronary syndromes varies from 40% till 65% of all STEMI patients25-27. It is also well known that MVD has a deleterious impact on survival as it frequently coincides with a large number of cardiovascular risk factors, diminished left ventricular ejection fraction and cardiogenic shock in general population. The data on gender-related differences in extent of the coronary artery disease, especially in the important context of STEMI, are not easily available. It would be tempting to blame MVD for the increase in mortality in women, however, an insignificant difference in MVD prevalence between men and women and a high proportion of women with single vessel disease tends to contradict established theories on this subject.
Bleeding following PCI affects nearly one third of all acute coronary syndrome patients. However, serious or life threatening bleeding complications are reported in randomised controlled trials or registries in a wide range of 1.4-15%. In the GRACE registry, there were 4.8%28 and in TIMI I trial29 15% STEMI patients with serious bleeding. Unfortunately, the fact that diagnostic criteria are not unified does not help to compare results. Moreover, there is a variety of patient- and procedure-related risk factors which may coincide in different combinations and increase the probability of serious bleeding. In our study serious bleeding was significantly more frequent in women what is consistent with other registries. What is important, the complication rate (1.1%) was relatively low, when compared to GRACE registry (5%). Interestingly, an intuitive assumption that a higher complication rate in women is related to anticoagulant or antiplatelet therapy was not confirmed by our findings – women were treated less aggressively. Nevertheless, female gender has been found by Nikolsky et al to be an independent risk factor of serious bleeding with OR 1.930 whereas Hamon et al in a meta-analysis of 10 studies found bleeding as a strong predictor of death and the female gender as one of the major predictors of bleeding31. Thus, it is not surprising that an increased bleeding complication rate coincides with a higher mortality in women in our study and in other reports.
The role of adjunctive and post-discharge medication following acute myocardial infarction is definite nowadays. Several agents have been proved to reduce mortality and reinfarction after STEMI1. The detailed explanation of lower usage of aspirin, heparin, clopidogrel, beta blockers and statins in women is difficult, and only a few circumstances justifies the lower percentage of clopidogrel (i.e., bleeding complications) use in women.
Multiple trials and registries concerning different aspects of STEMI have shown increased mortality in women when compared to men and a variety of possible reasons have been reported32. One of the most important is time to reperfusion, which is often prolonged due to lack of PCI capable centre located in the area of primary hospitalisation. In an effort to reduce delay from symptom onset to recanalisation of the infarct-related artery, physicians in hospitals without invasive cardiac facilities frequently face a dilemma on whether to transfer a patient to a cathlab or provide treatment on-site. Nevertheless available evidence suggests that transport for primary angioplasty improves the short- and long-term outcomes better than immediate thrombolysis33,34. The DANAMI-235 and PRAGUE-236 trials demonstrated a positive effect of transport to primary angioplasty as compared with fibrinolysis on site on 30-day survival in women. Gender-related differences in patients with STEMI without transport and transferred to another site to undergo primary PCI have not been thoroughly investigated so far. The most interesting and the most surprising finding is that in transported men prolongation of occlusion did not affect one-year mortality, whereas in transported women the tendency of higher mortality, however not significant, is clearly noticeable.
Conclusions
On the basis of this large multicentre national acute coronary syndrome registry, we conclude that despite poor clinical characteristics, less than satisfactory management, lower success rates after invasive approaches, and worse prognosis of women with STEMI, being a women itself, is not a risk factor for increased long-term mortality, however, other well known risk-factors deeply affecting the prognosis coincide frequently with the female gender.