Abstract
Background: In the International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) trial, among participants with stable coronary artery disease, the risk of cardiac events was similar between an invasive (INV) strategy of angiography and coronary revascularisation and a conservative (CON) strategy of initial medical therapy alone. Outcomes according to participant sex were not reported.
Aims: We aimed to analyse the outcomes of ISCHEMIA by participant sex.
Methods: We evaluated 1) the association between participant sex and the likelihood of undergoing revascularisation for participants randomised to the INV arm; 2) the risk of the ISCHEMIA primary composite outcome (cardiovascular death, any myocardial infarction [MI] or rehospitalisation for unstable angina, heart failure or resuscitated cardiac arrest) by participant sex; and 3) the contribution of the individual primary outcome components to the composite outcome by participant sex.
Results: Of 5,179 randomised participants, 1,168 (22.6%) were women. Female sex was independently associated with a lower likelihood of revascularisation when assigned to the INV arm (adjusted odds ratio 0.75, 95% confidence interval [CI]: 0.57-0.99; p=0.04). The INV versus CON effect on the primary composite outcome was similar between sexes (women: hazard ratio [HR] 0.96, 95% CI: 0.70-1.33; men: HR 0.90, 95% CI: 0.76-1.07; pinteraction=0.71). The contribution of the individual components to the composite outcome was similar between sexes except for procedural MI, which was significantly lower in women (9/151 [5.9%]) than men (67/519 [12.9%]; p=0.01).
Conclusions: In ISCHEMIA, women assigned to the INV arm were less likely to undergo revascularisation than men. The effect of an INV versus CON strategy was consistent by sex, but women had a significantly lower contribution of procedural MI to the primary outcome.
In the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial, among participants with chronic coronary artery disease and moderate to severe myocardial ischaemia, there was no difference in the incidence of ischaemic cardiac events over a period of 3.2 years between an initial invasive (INV) strategy (coronary angiography followed by revascularisation via percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG] surgery when indicated) and an initial conservative (CON) strategy; the effect of an INV versus a CON strategy by participant sex was not reported in the original publication.
The pathophysiology of coronary artery disease and its clinical presentation are known to be different between sexes12345678, and the efficacy, safety, and adoption of coronary interventions (both percutaneous and surgical) and of medical therapy varies significantly by sex19101112. It is thus unclear if the overall results of the ISCHEMIA trial hold true in both women and men.
In addition, in the ISCHEMIA trial, the individual components contributed differently to the primary composite outcome1314. Due to the described differences in the adoption and outcomes of the different treatment strategies for coronary artery disease between sexes13, the contribution to the individual components of the primary outcome in the INV and CON arms of the ISCHEMIA trial may be different by sex.
A better understanding of ISCHEMIA data by participant sex may inform the interpretation of the trial. Therefore, we conducted a post hoc analysis of the ISCHEMIA trial data by participant sex. The aims of this analysis were to compare 1) the association between participant sex and the likelihood and modality of revascularisation in the INV arm, 2) the effect of assignment to the INV and CON arms on the primary outcome by participant sex, and 3) the contribution of the individual components to the primary outcome among women and men.
Methods
DATA SOURCE
Data were obtained through the National Heart, Lung and Blood Institute (NHLBI) Biologic Specimen and Data Repositories Information Coordinating Center (BioLINCC). The need for an institutional review board (IRB) review was waived by the Weill Cornell Medicine IRB.
ISCHEMIA TRIAL DESIGN
The ISCHEMIA trial design and results have been previously published1315. In brief, ISCHEMIA was a multicentre, randomised, controlled, open-label trial that assigned participants with moderate to severe ischaemia on non-invasive testing and acceptable levels of angina to either an initial INV strategy (coronary angiography and coronary revascularisation if appropriate) plus medical therapy or to an initial CON strategy with medical therapy alone, with angiography/revascularisation reserved for medical therapy failure (refractory angina or a primary outcome event). In the INV arm, the mode of revascularisation (CABG or PCI) was at the discretion of treating physicians. In the CON arm, 544/2,591 (20.9%) participants (of whom 108 were women) underwent unplanned revascularisation due to worsening clinical status.
The primary outcome was the composite of death from cardiovascular causes, myocardial infarction (MI), and hospitalisation for unstable angina, heart failure, or resuscitated cardiac arrest. Outcome definitions in the ISCHEMIA trial are included in Supplementary Table 1. The definition of non-procedural (spontaneous) MI was based on the Third Universal Definition of Myocardial Infarction (UDMI) types 1, 2, 4b and 4c. Procedural MI (PMI) required higher biomarker thresholds for confirmation than the 3rd UDMI1315. An alternative, secondary definition used the same biomarker thresholds as the 3rd UDMI for defining PMI.
REVASCULARISATION BY SEX
To evaluate participant sex differences in revascularisation rates and modality, we examined the unadjusted and adjusted association between participant sex and the likelihood of undergoing revascularisation as well as the revascularisation modality (PCI or CABG) using logistic regression and multinomial logistic regression, respectively.
For these analyses, women and men in the INV arm who were revascularised without a preceding primary outcome event were categorised according to their first revascularisation procedure into the PCI or CABG group (INV-PCI and INV-CABG, respectively). Participants who did not undergo revascularisation or underwent revascularisation after having had a primary outcome event were the reference group. Participants in the CON arm who underwent unplanned revascularisation were not included in this analysis due to confounders related to key differences in clinical status and modality of revascularisation compared to participants who underwent planned revascularisation (Central illustration).
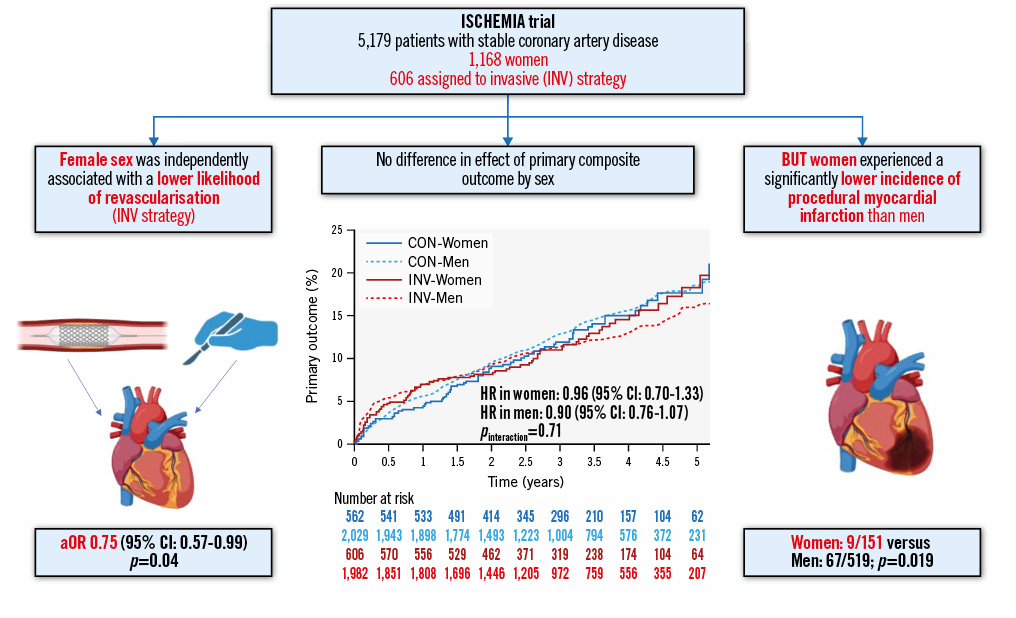
Central illustration. Outcome by sex in the ISCHEMIA trial. aOR: adjusted odds ratio; CI: confidence interval; CON: conservative; HR: hazard ratio; INV: invasive
EFFECT OF AN INVASIVE VERSUS A CONSERVATIVE STRATEGY BY PARTICIPANT SEX
To examine whether the effect of the two trial interventions (INV vs CON) were consistent among women and men, we compared the risk of the primary composite outcome and its components according to randomised treatment arm by participant sex.
The contribution of each individual component to the primary outcome was defined as the proportion of participants who met the primary outcome in whom that specific component was the only primary outcome event, i.e., participants who would not have met the primary outcome definition had they not had that specific event. MI was evaluated both overall (any MI) and stratified by the timing of its occurrence (PMI or spontaneous MI).
REVASCULARISATION OUTCOMES BY MODALITY AND PARTICIPANT SEX
We examined the risk of ISCHEMIA’s primary outcome and its components after each revascularisation modality by participant sex; for this analysis, women and men in the INV arm who underwent revascularisation without a preceding primary outcome event were categorised at the time of their first revascularisation procedure as INV-PCI or INV-CABG, as appropriate. Even in this analysis, participants in the CON arm who underwent unplanned revascularisation were not included because of the potential confounders described above. Time-to-first-event analyses (from the time of revascularisation) were then performed to examine the cumulative risk of the primary outcome and its components after revascularisation by PCI and CABG by participant sex.
STATISTICAL ANALYSIS
Continuous data are reported as mean±standard deviation for variables with a normal distribution or median (1st quartile [Q1], 3rd quartile [Q3]) for variables with a skewed distribution. Categorical data are reported as frequency (percentage). Kaplan-Meier cumulative event rates were calculated for women and men in the INV and CON arms, and Cox proportional hazards regression, which included an interaction test between female versus male sex and randomised group allocation, was used to derive hazard ratios (HRs) for the INV versus CON strategy in women and men and test for heterogeneity of the treatment effect across sex. The following covariate set was included in the multivariable logistic and multinomial logistic regression models examining the association between female versus male sex and the revascularisation modality used: age, sex, prior MI, current smoker, diabetes, left ventricular ejection fraction <45%, prior CABG, prior heart failure hospitalisation, chronic lung disease, prior stroke, known peripheral vascular disease, White versus non-White race, estimated glomerular filtration rate lower versus higher than 60 ml/min, and the number of diseased vessels (diameter stenosis ≥50%) as assessed by the coronary angiography core lab. Kaplan-Meier cumulative event rates were calculated for women and men in the INV-CABG and INV-PCI groups, censoring participants at the time of a first event or if lost to follow-up. Logistic regression was used to examine the association between female sex and the risk of PMI after revascularisation. These models were adjusted for the revascularisation modality (CABG vs PCI), randomised arm, and the covariates listed above.
All statistical analyses were performed with SAS software, version 9.3 (SAS Institute).
Results
STUDY POPULATION
Of 5,179 randomised participants in the ISCHEMIA trial, 1,168 (22.6%) were women. Baseline characteristics for women versus men are presented in Table 1. Compared with men, women were older and more likely to have hypertension and diabetes. The usage of guideline-directed medical therapy in men and women is presented in Supplementary Table 2 and Supplementary Table 3.
Table 1. Baseline characteristics of patients.
| Baseline characteristics | Women (N=1,168) | Men (N=4,011) | p-value |
|---|---|---|---|
| Age, years | 65.0 [59.0-71.0] | 64.0 [57.0-70.0] | 0.002 |
| Race | <0.001 | ||
| Black or African American | 57/1,154 (4.9) | 147/3,975 (3.7) | |
| Other | 289/1,154 (25) | 1,233/3,975 (31) | |
| White | 808/1,154 (70) | 2,595/3,975 (65) | |
| Hispanic or Latino ethnicity | 188/1,091 (17) | 575/3,724 (15) | 0.17 |
| LVEF, % | 62.0 [58.0-68.0] | 60.0 [55.0-64.0] | <0.001 |
| eGFR, ml/min/1.73 m² | 76.9 [61.7-92.9] | 83.2 [70.2-99.0] | <0.001 |
| Hypertension | 922/1,164 (79) | 2,867/3,997 (72) | <0.001 |
| Diabetes | 522/1,168 (45) | 1,642/4,011 (41) | 0.02 |
| Insulin-treated | 159/1,168 (14) | 333/4,011 (8.3) | <0.001 |
| Smoking status | <0.001 | ||
| Current smoker | 110/1,167 (9.4) | 530/4,007 (13) | |
| Former smoker | 301/1,167 (26) | 2,025/4,007 (51) | |
| Never smoked | 756/1,167 (65) | 1,452/4,007 (36) | |
| Family history of premature CAD | 297/1,016 (29) | 873/3,474 (25) | 0.01 |
| Prior MI | 184/1,165 (16) | 807/3,997 (20) | 0.001 |
| Prior PCI | 189/1,167 (16) | 861/4,008 (21) | <0.001 |
| Prior CABG | 32/1,168 (2.7) | 171/4,011 (4.3) | 0.02 |
| Prior HF | 61/1,168 (5.2) | 145/4,011 (3.6) | 0.14 |
| Atrial fibrillation/atrial flutter | 46/1,166 (3.9) | 175/4,007 (4.4) | 0.59 |
| Prior stroke | 40/1,168 (3.4) | 111/4,010 (2.8) | 0.28 |
| Prior cerebrovascular disease | 89/1,166 (7.6) | 288/3,999 (7.2) | 0.66 |
| Prior peripheral arterial disease | 43/1,165 (3.7) | 161/4,003 (4.0) | 0.67 |
| History of angina | 1,068/1,168 (91) | 3,573/4,011 (89) | 0.02 |
| Multivessel disease by CCTA | |||
| Two-vessel disease | 184/816 (23) | 754/3,093 (24) | 0.28 |
| Three-vessel disease | 205/816 (25) | 1,142/3,093 (37) | <0.001 |
| Data are presented as median [IQR] or n/N (%). CABG: coronary artery bypass grafting; CAD: coronary artery disease; CCTA: coronary computed tomography angiography; eGFR: estimated glomerular filtration rate; HF: heart failure; IQR: interquartile range; LVEF: left ventricular ejection fraction; MI: myocardial infarction; PCI: percutaneous coronary intervention | |||
REVASCULARISATION BY PARTICIPANT SEX IN THE INVASIVE ARM
Among participants who were randomised to the INV arm, 2,406/2,588 (93%) underwent coronary angiography without a preceding primary endpoint event (1,842/1,982 [93%] men and 564/606 [93%] women); of whom 518/2,400 (22%) had either intravascular imaging or coronary physiology performed (399/1,838 [22%] men and 119/562 [21%] women). A total of 2,012/2,588 (78%) participants randomised to the INV arm underwent revascularisation without a preceding primary outcome event (435/606 [72%] women and 1,577/1,982 [80%] men). Female participant sex was independently associated with a lower likelihood of undergoing revascularisation even after adjustment for age and clinical risk factors, as well as after adjustment for angiographic findings (Table 2).
Among participants in the INV arm who were revascularised, PCI rather than CABG was used in 345/435 (79.3%) women versus 1,155/1,577 (73.2%) men (p=0.01). After adjustment for age and other clinical risk factors, as well as after adjustment for angiographic findings, women were less likely than men to undergo PCI as well as CABG, but there was a stronger negative association between female participant sex and the likelihood of undergoing surgery (Table 3).
Table 2. Association between sex and the likelihood of undergoing revascularisation for patients randomised to an invasive strategy.
| Model | OR for women vs men (95% CI) |
|---|---|
| Unadjusted | 0.65 (0.53-0.80);p<0.001 |
| Adjusted for age | 0.66 (0.53-0.81);p<0.001 |
| Adjusted for clinical risk factors* | 0.62 (0.49-0.78);p<0.001 |
| Adjusted for clinical and angiographic risk factors† | 0.75 (0.57-0.99);p=0.04 |
| Adjusted for clinical and angiographic risk factors¶ | 0.69 (0.52-0.90);p=0.006 |
| *Adjusted for the following covariate set: age, sex, prior MI, current smoker, diabetes, left ventricular ejection fraction <45%, prior CABG, prior heart failure hospitalisation, chronic lung disease, prior stroke, known peripheral vascular disease, White versus non-White race, and eGFR <60 ml/min. †Fully adjusted to prior variables in addition to the number of diseased vessels (>50% diameter stenosis per angiographic core lab analysis). ¶Fully adjusted to prior variables in addition to the number of diseased vessels (>70% diameter stenosis per angiographic core lab analysis). CABG: coronary artery bypass grafting; CI: confidence interval; eGFR: estimated glomerular filtration rate; MI: myocardial infarction; OR: odds ratio | |
Table 3. Association between sex and the likelihood of undergoing PCI and CABG for patients randomised to an invasive strategy.
| Model | OR for women vs men (95% CI) | |
|---|---|---|
| OR for PCI | OR for CABG | |
| Unadjusted | 0.71 (0.57-0.88); p=0.001 | 0.51 (0.38-0.67); p<0.001 |
| Adjusted for age | 0.71 (0.58-0.89); p=0.003 | 0.51 (0.38-0.68); p<0.001 |
| Adjusted for clinical risk factors* | 0.67 (0.53-0.86); p=0.001 | 0.48 (0.35-0.66); p<0.001 |
| Adjusted for clinical and angiographic risk factors† | 0.76 (0.58-1.01); p=0.06 | 0.64 (0.44-0.94); p=0.02 |
| Adjusted for clinical and angiographic risk factors¶ | 0.70 (0.54-0.93); p=0.01 | 0.58 (0.40-0.83); p=0.003 |
| *Adjusted for the following covariate set: age, sex, prior MI, current smoker, diabetes, left ventricular ejection fraction <45%, prior CABG, prior heart failure hospitalisation, chronic lung disease, prior stroke, known peripheral vascular disease, White versus non-White race, and eGFR <60 ml/min. †Fully adjusted to prior variables in addition to the number of diseased vessels (>50% diameter stenosis per angiographic core lab analysis). ¶Fully adjusted to prior variables in addition to the number of diseased vessels (>70% diameter stenosis per angiographic core lab analysis). CABG: coronary artery bypass grafting; CI: confidence interval; eGFR: estimated glomerular filtration rate; MI: myocardial infarction; OR: odds ratio; PCI: percutaneous coronary intervention | ||
CROSSOVER BY PARTICIPANT SEX IN THE CONSERVATIVE ARM
Among participants who were randomised to the CON arm, 487/2,591 (19%) underwent coronary angiography without a preceding primary endpoint event (375/2,029 [18%] men and 112/562 [20%] women); and 382/2,591 (15%) underwent revascularisation without a preceding primary outcome event (79/562 [14%] women and 303/2,029 [15%] men).
EFFECT OF AN INVASIVE VERSUS A CONSERVATIVE STRATEGY BY PARTICIPANT SEX AND CLINICAL OUTCOMES BY REVASCULARISATION MODALITY AND PARTICIPANT SEX
The risk of the primary composite outcome was similar between the INV and CON trial arms for both women and men (Figure 1). There was no statistically significant interaction between participant sex and the risk of the primary outcome or any of its components including death, any MI, stroke, or rehospitalisation for unstable angina, heart failure, or resuscitated cardiac arrest (Figure 1, Supplementary Figure 1). In the analysis of MI stratified by the timing of the event, however, women experienced significantly less PMI than men, while there were no differences in spontaneous MI (Table 4).
The association between female participant sex and PMI was not statistically significant after adjustment for the revascularisation modality (CABG vs PCI; odds ratio [OR] 0.52, 95% confidence interval [CI]: 0.23-1.05; p=0.058) or after adjustment for the revascularisation modality, randomised arm, and clinical risk factors (OR 0.62, 95% CI: 0.26-1.30; p=0.236); these results were consistent when using the alternative PMI definition (Supplementary Table 4).
Among patients in the INV arm who underwent revascularisation, there was no statistical interaction between female participant sex and revascularisation modality (CABG vs PCI) for the risk of the primary outcome or its individual components (Figure 2, Supplementary Figure 2).
Among patients who met the primary outcome, women were more likely than men to experience more than one type of primary outcome event. The proportion of participants who had MI as the only primary outcome event (i.e., the contribution of MI to the primary outcome) was significantly lower in women compared with men (Table 5). Specifically, women were less likely than men to have PMI as their only primary outcome event.
Similarly, when restricting the analysis to patients in the INV arm who met the primary outcome after undergoing revascularisation, MI was less commonly the only primary outcome event for women than for men (Table 6), a difference that was predominantly driven by the rates of PMI.
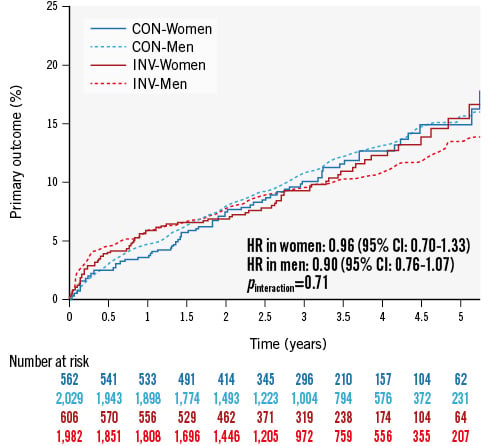
Figure 1. Cumulative incidence of the primary outcome according to randomised group assignment for female and male participants. CI: confidence interval; CON: conservative; HR: hazard ratio; INV: invasive
Table 4. Cumulative incidence of primary outcome components by participant sex.
| CON | INV | All | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Women (N=562) | Men (N=2,029) | p-value | Women (N=606) | Men (N=1,982) | p-value | Women (N=1,168) | Men (N=4,011) | p-value* | |
| Cardiovascular death | 8.9% (30) | 5.8% (77) | 0.19 | 7.2% (28) | 4.7% (60) | 0.07 | 8.1% (58) | 5.3% (137) | 0.03 |
| Any MI | 11.2% (43) | 12.4% (185) | 0.46 | 10.5% (44) | 10.5% (163) | 0.32 | 10.8% (87) | 11.5% (348) | 0.21 |
| PMI | 0.6% (3) | 1.2% (21) | 0.27 | 1.3% (8) | 3.3% (62) | 0.02 | 1.0% (11) | 2.2% (83) | 0.01 |
| Spontaneous MI | 10.6% (40) | 11.4% (168) | 0.59 | 9.1% (36) | 7.4% (105) | 0.74 | 9.8% (76) | 9.5% (273) | 0.79 |
| Hospitalisation | 3.4% (13) | 3.6% (47) | 0.93 | 6.1% (22) | 3.4% (45) | 0.08 | 4.8% (35) | 3.5% (92) | 0.21 |
| *log-rank. Kaplan-Meier rates are provided for each event. CON: conservative; INV: invasive; MI: myocardial infarction; PMI: procedural myocardial infarction | |||||||||
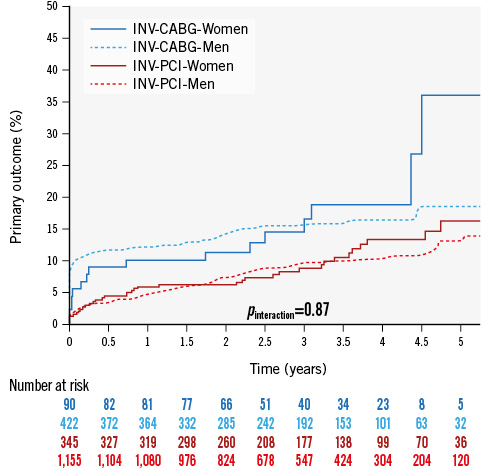
Figure 2. Cumulative incidence of the primary outcome after revascularisation by CABG or PCI (median follow-up after revascularisation 2.09 years [0.17, 3.66]) for women and men randomised to an invasive strategy. CABG: coronary artery bypass grafting; CON: conservative; INV: invasive; PCI: percutaneous coronary intervention
Table 5. Contribution of individual components to primary outcome components by participant sex by intention-to-treat.
| CON | INV | All | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Women (N of events =74/562) | Men (N of events =278/2,029) | p-value 0.11 | Women (N of events =77/606) | Men (N of events =241/1,982) | p-value 0.07 | Women (N of events =151/1,168) | Men (N of events =519/4,011) | p-value 0.02 | |
| Cardiovascular death only | 20 (27.0) | 53 (19.1) | 0.14 | 15 (19.5) | 42 (17.4) | 0.73 | 35 (23.2) | 95 (18.3) | 0.20 |
| Any MI only | 34 (46.0) | 155 (55.8) | 0.15 | 32 (41.6) | 138 (57.3) | 0.018 | 66 (43.7) | 293 (56.5) | 0.007 |
| PMI only | 2 (2.7) | 16 (5.8) | 0.38 | 7 (9.1) | 51 (21.2) | 0.017 | 9 (5.9) | 67 (12.9) | 0.019 |
Spontaneous MI only |
31 (41.9) | 137 (49.3) | 0.30 | 25 (32.5) | 81 (33.6) | 0.89 | 56 (37.1) | 218 (42.0) | 0.30 |
| Hospitalisation only | 5 (6.8) | 33 (11.9) | 0.29 | 13 (16.9) | 29 (12.0) | 0.33 | 18 (11.9) | 62 (11.9) | 0.99 |
| More than one type of primary outcome event | 15 (20.3) | 37 (13.3) | 0.14 | 17 (22.1) | 32 (13.3) | 0.07 | 32 (21.2) | 69 (13.3) | 0.02 |
| Data are presented as N (%). CON: conservative; INV: invasive; MI: myocardial infarction; N: number; PMI: procedural myocardial infarction | |||||||||
Table 6. Contribution of individual components to primary outcome components by participant sex and revascularisation modality in the INV arm and by revascularisation modality.
| INV-REVASC | INV-CABG | INV-PCI | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Women (N of events =52/445) | Men (N of events =179/1,609) | p-value 0.027 | Women (N of events =16/93) | Men (N of events =68/437) | p-value 0.018 | Women (N of events =36/352) | Men (N of events =111/1,172) | p-value 0.41 | |
| Cardiovascular death only | 10 (19.2) | 28 (15.6) | 0.53 | 3 (18.8) | 8 (11.8) | 0.43 | 7 (19.4) | 20 (18.0) | 0.81 |
| MI (any) only | 21 (62.0) | 111 (62.0) | 0.007 | 5 (31.3) | 47 (69.1) | 0.009 | 16 (44.4) | 64 (57.7) | 0.18 |
| PMI only | 7 (13.5) | 51 (28.5) | 0.030 | 3 (18.8) | 31 (45.6) | 0.087 | 4 (11.1) | 20 (18.0) | 0.44 |
Spontaneous MI only |
14 (26.9) | 55 (30.7) | 0.73 | 2 (12.5) | 14 (20.6) | 0.73 | 12 (33.3) | 41 (36.9) | 0.84 |
| Hospitalisation only | 9 (11.2) | 20 (11.2) | 0.24 | 4 (25.0) | 7 (10.3) | 0.21 | 5 (13.9) | 13 (11.7) | 0.77 |
| More than one type of primary outcome event | 12 (23.1) | 20 (11.2) | 0.039 | 4 (25.0) | 6 (8.9) | 0.09 | 8 (22.2) | 14 (12.6) | 0.18 |
| Data are presented as N (%). CABG: coronary artery bypass grafting; INV: invasive; MI: myocardial infarction; N: number; PCI: percutaneous coronary intervention; PMI: procedural myocardial infarction; REVASC: revascularisation | |||||||||
Discussion
The key findings of this sex-stratified analysis of the ISCHEMIA trial are as follows: 1) female participant sex was independently associated with a lower likelihood of revascularisation among participants randomised to an INV treatment strategy even after adjustment for angiographic and clinical risk factors, and this negative association was stronger for CABG than for PCI; 2) at the median follow-up of 3.2 years, the incidence of the primary composite outcome of cardiovascular death, MI, or hospitalisation for unstable angina, heart failure, or resuscitated cardiac arrest was similar in the INV and CON arms in both sexes; 3) PMI contributed significantly less to the primary composite outcome in women than in men.
A lower likelihood of women compared with men to be referred for coronary revascularisation is consistent with the results of large registry studies161718, but it is unclear if the lower referral rates of women for revascularisation is due to physician bias or sex differences in baseline clinical status or the extent of coronary artery disease. The ISCHEMIA trial authors have previously reported that among enrolled trial participants, the extent of coronary disease was lower in women compared with men, but the prevalence of left anterior descending artery disease (one of the key drivers in the decision to revascularise) was similar between sexes4. In our analysis, the difference in revascularisation rates between sexes persisted even after adjustment for clinical and angiographic covariates, suggesting that referral bias may have played an important role.
The confirmation that randomisation to an INV versus CON strategy resulted in a similar risk of the primary composite outcome for both women and men contributes to a more complete understanding of the ISCHEMIA trial, since the results of the primary analysis were driven predominantly by the results in men. The relative effect of an INV versus CON strategy could have differed between women and men due to known sex differences in the efficacy and utilisation of medical therapy11920 and several key prevention strategies (including the use of antiplatelet and lipid-lowering therapy21222324) that were confirmed among participants enrolled in the ISCHEMIA trial4. In addition, the procedural risk of coronary revascularisation by both PCI and CABG has been shown to be higher in women, who also have a higher risk of cardiovascular events during the years after a coronary intervention compared with men1910.
As regards the individual components of the primary composite outcome, we found that women had significantly lower rates of PMI compared with men. We have previously reported that in ISCHEMIA the incidence of PMI was dependent on the revascularisation modality and significantly higher for CABG than for PCI25, and in the present study the lower incidence of PMI among women was likely explained, at least in part, by the lower adoption of surgery as the coronary revascularisation modality in women.
The negative association of female participant sex with PMI did not remain statistically significant after adjustment for revascularisation modality and clinical and procedural risk factors; our study therefore does not directly support an independent association between participant sex and PMI. However, we cannot rule out the possibility that other participant sex-related factors contributed to the observed lower incidence of PMI in women versus men. For example, troponin levels are known to be lower in women26 compared to men12272829, and since the PMI definitions used in ISCHEMIA rely on biomarker criteria that are not sex specific, it is possible that PMI rates were artificially reduced in women.
In any case, the observation of a significant difference in PMI contribution to the primary outcomes by participant sex in ISCHEMIA is important because of the unclear clinical and prognostic relevance of PMI compared with the other clinical events included in the primary outcome1430.
Lastly, it must be noted that the crude rate of cardiovascular death in the overall, INV, and CON cohorts was significantly higher in women than in men in the present analysis. This observation is consistent with previous studies10313233, but this finding may be due to multiplicity in testing and low statistical power rather than a truly significant difference between the sexes3435.
Limitations
This post hoc analysis has important limitations. While our adjustment models were based on all available clinical and angiographic data and the initial participant cohort was relatively homogeneous (as all participants met the ISCHEMIA inclusion criteria), it is likely that there are unaccounted confounders in the reported comparisons. As in many cardiovascular trials, the number of women enrolled in ISCHEMIA was relatively low, and lower than anticipated (actual: 23% vs anticipated: 35%), hence, the reported comparisons may be underpowered. Any nominal differences in event rates should therefore be interpreted with caution. In addition, the comparisons between revascularisation modalities suffer from an intrinsic treatment allocation bias and must only be seen as hypothesis-generating.
Conclusions
In conclusion, in the ISCHEMIA trial, women were significantly less likely to undergo revascularisation when assigned to the INV treatment arm. The similarity in cardiac outcomes between an INV versus a CON strategy seen in the overall population was confirmed in both women and men, but women had a significantly lower incidence of PMI than men.
Conflict of interest statement
D.L. Bhatt discloses the following relationships - advisory board: Angiowave, Bayer, Boehringer Ingelheim, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, High Enroll, Janssen, Level Ex, McKinsey, Medscape Cardiology, Merck, MyoKardia (now part of Bristol-Myers Squibb), NirvaMed, Novo Nordisk, PhaseBio, PLx Pharma, and Stasys; board of directors: AHA New York City, Angiowave (stock options), Bristol-Myers Squibb (stock), DRS.LINQ (stock options), and High Enroll (stock); consultant: Broadview Ventures, Hims, SFJ, and Youngene; data monitoring committees: Acesion Pharma, Assistance Publique-Hôpitaux de Paris, Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Boston Scientific (Chair, PEITHO trial), Cleveland Clinic, Contego Medical (Chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo; for the ABILITY-DM trial, funded by Concept Medical; for ALLAY-HF, funded by Alleviant Medical), Novartis, Population Health Research Institute, and Rutgers University (for the NIH-funded MINT Trial); honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Chair, ACC Accreditation Oversight Committee), Arnold and Porter law firm (work related to Sanofi/Bristol-Myers Squibb clopidogrel litigation), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), Canadian Medical and Surgical Knowledge Translation Research Group (clinical trial steering committees), CSL Behring (AHA lecture), Cowen and Company, Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), K2P (Co-Chair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Oakstone CME (Course Director, Comprehensive Review of Interventional Cardiology), Piper Sandler, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), WebMD (CME steering committees), and Wiley (steering committee); other: Clinical Cardiology (Deputy Editor); patent: sotagliflozin (named on a patent for sotagliflozin assigned to Brigham and Women’s Hospital who assigned to Lexicon; neither D.L. Bhatt nor Brigham and Women’s Hospital have received any income from this patent); research funding: Abbott, Acesion Pharma, Afimmune, Aker BioMarine, Alnylam, Amarin, Amgen, AstraZeneca, Bayer, Beren, Boehringer Ingelheim, Boston Scientific, Bristol-Myers Squibb, Cardax, CellProthera, Cereno Scientific, Chiesi, CinCor, Cleerly, CSL Behring, Eisai, Ethicon, Faraday Pharmaceuticals, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Garmin, HLS Therapeutics, Idorsia, Ironwood, Ischemix, Janssen, Javelin, Lexicon, Lilly, Medtronic, Merck, Moderna, MyoKardia (now part of Bristol-Myers Squibb), NirvaMed, Novartis, Novo Nordisk, Otsuka, Owkin, Pfizer, PhaseBio, PLx Pharma, Recardio, Regeneron, Reid Hoffman Foundation, Roche, Sanofi, Stasys, Synaptic, The Medicines Company (now part of Novartis), Youngene, and 89bio; royalties: Elsevier (Editor, Braunwald’s Heart Disease); site co-investigator: Abbott, Biotronik, Boston Scientific, CSI, Endotronix, St. Jude Medical (now Abbott), Philips, SpectraWAVE, Svelte, and Vascular Solutions; trustee: American College of Cardiology; unfunded research: FlowCo. J.H. Alexander has had research grants through Duke University from Artivion, Bayer, Bristol-Myers Squibb, CSL Behring, Ferring, the U.S. FDA, Humacyte, and the US NIH; and received advisory board, consulting, or honoraria payments from AbbVie, Akros, Artivion, AtriCure, Bayer, Bristol-Myers Squibb, Ferring, GlaxoSmithKline, Janssen, Novostia, Pfizer, Portola, Quantum Genomics, Theravance, Teikoku, and Veralox. G.W. Stone discloses speaker honoraria from Medtronic, Pulnovo, Infraredx, Abiomed, Amgen, and Boehringer Ingelheim; consultant to Abbott, Daiichi Sankyo, Ablative Solutions, CorFlow, Cardiomech, Gore, Robocath, Miracor, Vectorious, Abiomed, Valfix, Apollo Therapeutics, Elucid Bio, TherOx, HeartFlow, Neovasc, Ancora, Occlutech, Impulse Dynamics, Adona Medical, Millennia Biopharma, Oxitope, Cardiac Success, HighLife, Elixir, and RCE; equity/options from Ancora, Cagent, Applied Therapeutics, Biostar family of funds, SpectraWave, Orchestra Biomed, Aria, Cardiac Success, Valfix, and Xenter; his employer, Mount Sinai Hospital, has received research grants from Abbott, Abiomed, BioVentrix, Cardiovascular Systems Inc, Philips, Biosense Webster, Shockwave Medical, Vascular Dynamics, Pulnovo, and V-Wave. L. Harik is partially supported by a T-32 multidisciplinary research training grant in cardiovascular disease from the National Heart, Lung, and Blood Institute (1 T32 HL160520-01A1). M. Gaudino has received research grants from the National Institutes of Health, the Canadian Health and Research Institutes, and the Starr Foundation. S. Sandner has been supported by the Austrian Science Fund KLI1147-B. The other authors have no disclosures.Impact on daily practiceWomen with stable coronary artery disease were less likely to undergo revascularisation than men. The effect of an invasive or conservative management strategy on cardiovascular death and myocardial infarction as well as rehospitalisation for unstable angina, heart failure or resuscitated cardiac arrest was overall similar for both sexes, but women had less procedural myocardial infarction.
Supplementary data
To read the full content of this article, please download the PDF.