Abstract
Several expert documents on sex-based differences in interventional outcomes are now available; however, this is the first position paper from the EAPCI Women Committee discussing the potential influence of sex in the percutaneous treatment of coronary and structural heart disease. Despite the misconception that coronary artery disease is a “man’s disease”, contemporary data show a growing incidence in women. However, women are under-represented in randomised coronary clinical trials (~25%). The generalisation of such studies is, therefore, problematic in decision making for females undergoing coronary intervention. Differences in pathophysiology between sexes exist, highlighting the need for greater awareness amongst healthcare professionals to enable best evidence-based therapies for women as well as for men. Reassuringly, women represent half of the population included in transcatheter aortic valve implantation clinical trials and may actually benefit more. Growing evidence is also emerging for other interventional atrial procedures which may well be advantageous to women. Awareness of sex disparities is increasing, and we must all work collaboratively within our profession to ensure that we provide effective care for all patients with heart disease. The EAPCI Women Committee aims to highlight such issues through this position paper and through visibility within the interventional community.
Abbreviations
ACS: acute coronary syndrome
BMS: bare metal stent
BVS: bioresorbable vascular scaffold
CABG: coronary artery bypass grafting
CAD: coronary artery disease
CTO: chronic total occlusion
CVA: cerebrovascular accident
DES: drug-eluting stent(s)
EAPCI: European Association of Percutaneous Coronary Interventions
ECG: electrocardiogram
EES: everolimus-eluting stent
HR: hazard ratio
LAA: left atrial appendage
LVEF: left ventricular ejection fraction
MACE: major adverse cardiovascular events
MR: mitral regurgitation
PCI: percutaneous coronary intervention
RR: relative risk
SAVR: surgical aortic valve replacement
STEMI: ST-elevation myocardial infarction
TAVI: transcatheter aortic valve implantation
TR: tricuspid regurgitation
ULMCA: unprotected left main coronary artery
VARC: Valve Academic Research Consortium
Introduction
Despite the common misconception that coronary artery disease (CAD) is a “man’s disease”, some contemporary data show a growing incidence of CAD across Europe in women1. However, women are usually under-represented in randomised coronary clinical trials, accounting for ~25% of patients, with contributing factors being comorbidities, child-bearing potential and older age. This makes the generalisation of such studies problematic in decision making for individual females undergoing percutaneous coronary intervention (PCI). Registry data show that, despite having smaller vessels than men, women are less likely to receive drug-eluting stents (DES)2. The prevalence of risk factors for stent thrombosis and restenosis, including older age, diabetes mellitus, and small vessel size, is also different between sexes undergoing PCI, which raises the important question concerning whether patient sex modifies significantly the relationship between stent type and PCI outcomes during long-term follow-up3,4. Table 1 shows the current knowledge gaps in this area. As opposed to studies of CAD, women represent half of the population included in clinical trials evaluating transcatheter aortic valve implantation (TAVI) for the treatment of symptomatic aortic stenosis. Figure 1 shows a diagrammatic representation of the impact of both CAD and structural heart disease upon women and the comparable results of subsequent intervention with men.
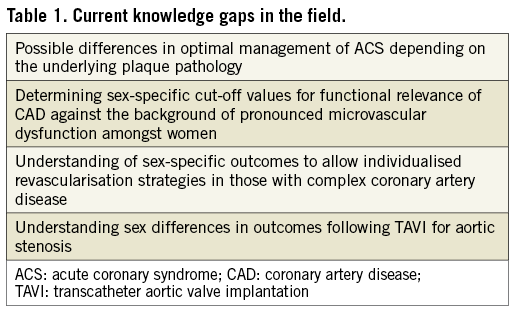
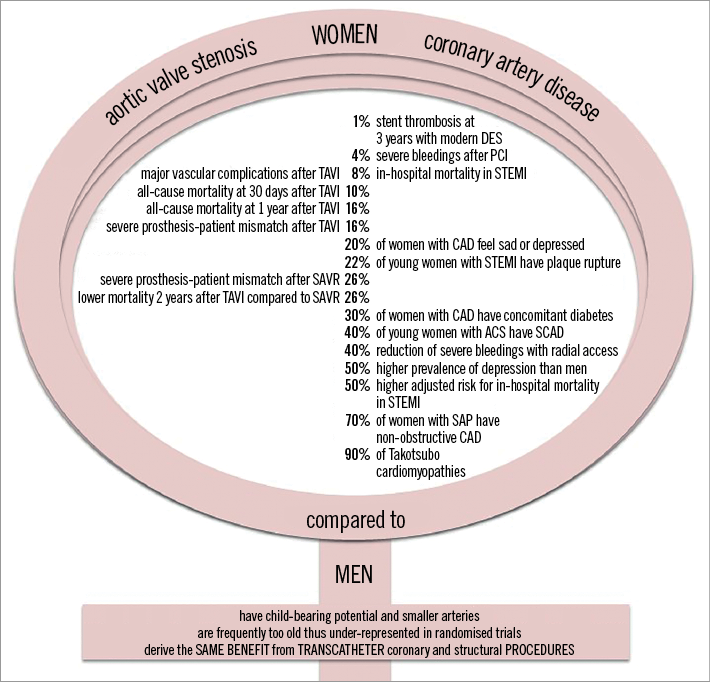
Figure 1. A diagrammatic representation of the impact of both CAD and structural heart disease on women and the comparable results of subsequent intervention with men.
Against this background, the EAPCI Women Committee met during the European Society of Cardiology Congress on 26 August 2017 in Barcelona, Spain, with the aim of developing a position paper regarding the potential influence of sex in the percutaneous treatment of both CAD and structural heart disease. This expands on prior published expert documents on sex-based differences in interventional outcomes.
PATHOPHYSIOLOGY OF CORONARY ARTERY AND STRUCTURAL HEART DISEASE IN WOMEN
CORONARY ARTERY DISEASE
Almost 70% of women presenting with stable angina have been reported to have non-obstructive CAD (NOCAD)5. Microvascular coronary dysfunction (MCD) has been demonstrated to be the main mechanism of angina in women ≤65 years of age. A definitive diagnosis can be made with the use of invasive coronary vasomotor testing or consideration of positron emission tomography scanning and should not be underestimated due to the worse prognosis of MCD6. Intravascular imaging and functional assessment can be used for further assessment, as will be discussed later. Another mechanism to be considered is that women more often have hypertrophy of the left ventricle and, in the setting of relative anaemia, there may be a mismatch in the oxygen supply and demand.
ACUTE CORONARY SYNDROMES
Another important difference in acute coronary syndrome (ACS) pathophysiology between men and women is that, similar to stable angina, women are more likely to have NOCAD on angiography. There are many potential explanations for this, such as angiographic underestimation of the true CAD burden, higher-risk plaque characteristics, MCD, spontaneous coronary artery dissection (SCAD), coronary spasm or Takotsubo cardiomyopathy. Women presenting with ACS, more frequently non-STEMI than men, with NOCAD have an elevated risk of cardiac events7, suggesting that appropriate diagnosis and optimal secondary prevention with antiplatelet agents and statins are essential.
SPONTANEOUS CORONARY ARTERY DISSECTION
The spontaneous separation of the layers of the coronary artery wall, termed SCAD, notably being neither iatrogenic nor traumatic, is gaining recognition as an important cause of ACS especially in young women. Indeed, in contemporary series, women accounted for 92-95% of the population with SCAD (mean age 44-55 years) with a prevalence of 22-43% in young women, higher among those with pregnancy-related myocardial infarction (MI)8. Coronary angiography is the first-line imaging modality for these patients; however, it has significant limitations as only the lumen and not the arterial wall is visualised, with only one third obvious by angiography alone. Therefore, dedicated intracoronary imaging techniques may improve diagnosis.
TAKOTSUBO CARDIOMYOPATHY
Another presentation of ACS, more common in women (9:1), is Takotsubo cardiomyopathy, which is associated with an early mortality of 3-5% and is the cause of MI in 1-8% of women9. This syndrome is typically, but not always, caused by emotional stress, with catecholamine release leading to stunning of the myocardium with hypokinesia/akinesia in the mid segments and apex of the left ventricle. To date, there is no specific therapy, but recommended strategies aim to prevent cardiogenic shock/arrhythmias, avoiding catecholamine release.
STRUCTURAL HEART DISEASE
At the time of treatment, women with aortic stenosis are approximately two years older compared to their male counterparts, typically with higher transvalvular pressure gradients and smaller valve areas10.
Furthermore, the left ventricular response to increased afterload in aortic stenosis shows sex-specific differences with concentric hypertrophy, smaller left ventricular volumes and preserved left ventricular ejection fraction (LVEF) in women, whereas men more often develop left ventricular dilatation, fibrosis and systolic dysfunction11. The typical left ventricular geometry in women also contributes to the higher prevalence of paradoxical low-flow low-gradient AS.
Several sex differences have been observed in mitral valve pathology and mitral regurgitation characteristics in patients undergoing mitral valve surgery. Posterior leaflet prolapse, flail and annular dilatation are more frequent in men, who are more likely to require surgery. In contrast, mitral annular calcification, leaflet thickening and myxomatous mitral valves and the presence of some degree of mitral stenosis are more common in women12.
INTRACORONARY IMAGING MODALITIES AND FUNCTIONAL ASSESSMENT IN WOMEN
CORONARY PLAQUE MORPHOLOGY
Several studies using intravascular ultrasound (IVUS) have demonstrated that women have a lower atherosclerotic plaque burden13. Regarding plaque composition, studies have shown some differences in calcium and necrotic core components that tend to be attenuated in older and stable patients14.
Intracoronary imaging has confirmed in vivo the sex differences in the substrate for ACS, especially in young women. A recent IVUS study demonstrated that, in ST-elevation myocardial infarction (STEMI) patients <65 years old, 59% of men versus 22% of women had plaque rupture. In those ≥65 years, no differences in culprit plaque morphology were found15. High-resolution intracoronary imaging with OCT has been able to demonstrate in vivo the presence of plaque erosion16. Furthermore, IVUS and especially OCT have also contributed significantly to increasing the recognition of SCAD. Supplementary Figure 1 illustrates the case of a 51-year-old lady presenting with anterolateral STEMI with SCAD.
FUNCTIONAL CORONARY STENOSIS SEVERITY ASSESSMENT
A number of studies have demonstrated that, for similar degrees of coronary luminal obstruction, the fractional flow reserve (FFR) result is significantly higher in women compared with men. A substudy of the landmark “Fractional flow reserve versus Angiography for Multi-vessel Evaluation” (FAME) trial reported such results with angiographically equivalent lesions less likely to cause ischaemia in women, with the proportion of FFR values ≤0.80 in 50-70% lesions lower in women than in men (21.1% vs. 39.5%; p<0.001); however, there was a similar relative risk reduction in death, MI and repeat revascularisation with the use of FFR17. Indeed, when considering predicting FFR ≤0.80, IVUS had a lower positive predictive value in women, probably as a consequence of the smaller body surface area and subsequent left ventricular mass and hence smaller myocardial territory at jeopardy18. The postulated reason for this finding is higher MCD in women and hence impaired response to vasodilators. If there remains doubt with regard to the significance of a lesion, then both FFR and IVUS should be utilised, assuming that there are no issues with IVUS due to small vessel size.
TRANSCATHETER CORONARY AND STRUCTURAL INTERVENTIONS IN WOMEN
PRIMARY PCI
The significant benefits of early reperfusion in STEMI in both sexes are now unquestionable. This is reflected in current guidelines19. Nevertheless, women have a higher risk of in-hospital mortality and adverse outcomes including those in contemporary primary PCI studies3,20. There are a number of reasons postulated which may contribute to inferior outcomes. Firstly, women delay longer in seeking medical treatment for symptoms of STEMI21. There is also a demonstrable delay in door-to-balloon time22. In addition, women commonly have atypical symptoms including back or neck pain, pleuritic chest pain, indigestion and dyspnoea23. STEMI may not be suspected initially, due to the unclear history and a general underestimation of the risk in women. One of the most important factors is the older age of women at presentation and comorbidities. Women experience more bleeding complications, and it is recognised that significant bleeding is associated with a higher mortality24 (Supplementary Appendix 1). Use of radial access, particularly in STEMI, has reduced this complication.
COMPLEX PERCUTANEOUS CORONARY INTERVENTIONS
Women presenting with stable CAD and obstructive CAD frequently undergo complex PCI. Usually such patients are then excluded from randomised clinical trials. In the SYNTAX trial, women accounted for only 22.3% overall. Specifically, women with unprotected left main coronary artery (ULMCA) disease represented only 10.3%. When women from the ULMCA substudy were evaluated (CABG n=85; PCI n=100), there was no difference in the primary endpoint of major adverse cardiac and cerebrovascular events (MACCE) (CABG 21.3% vs. PCI 26.3%; p=0.47) at three years. Furthermore, the SYNTAX II score revealed that females required lower anatomic SYNTAX scores to achieve similar mortality in both the PCI and CABG arms, as female sex is a clinical predictor in the model.
The limited data available also come from retrospective data analysis, such as the Milan and New-Tokyo (MITO) registry. In this challenging subset of patients with ULMCA disease, women had a greater number of comorbidities and more complex lesions, resulting in a higher incidence of cardiac death. After propensity matching, there was no difference in the occurrence of MACE but cardiac death showed only a trend to be higher in women25. As there were small numbers, this difference in cardiac events could be explained by the consideration that ULMCA disease in women may be influenced by those risk factors not analysed and considered in the propensity model.
The “Interventional Cardiology Research In-cooperation Society-left MAIN revascularization” registry was recently published comparing 2,328 patients (23.4% women) undergoing ULMCA PCI with DES. At a median follow-up of 2.9 years (IQR 1.0-4.1), the incidence of all-cause death, MI or stroke was comparable between sexes (10.8% vs. 10.8%, log-rank p=0.587)26. A further sub-analysis from patient-level data from women enrolled in randomised DES trials focused on complex PCI showed an increased risk of MACE at three years in the complex PCI group, but use of new-generation DES did reduce MACE and stent thrombosis compared with first-generation devices27. With regard to chronic total occlusions (CTO), data from registries suggest that such complex PCI in women is safe and feasible. However, women were less likely to undergo percutaneous revascularisation for a CTO and had a lower success rate following a CTO procedure28.
An example of complex PCI and concurrent TAVI in an elderly lady presenting with pulmonary oedema and cardiogenic shock is illustrated in Supplementary Figure 2.
IMPACT OF CORONARY STENT TECHNOLOGIES EVOLUTION
Under the auspices of the Society for Cardiovascular Angiography and Interventions’ Women in Innovation Initiative (WIN), a patient-level meta-analysis has been undertaken to investigate the efficacy and safety profiles of DES in women29. A total of 11,557 women in 26 DES trials from 2000-2013 were included. At three years, the estimated cumulative incidences of death or MI were 12.8%, 10.9% and 9.2% in female patients treated with BMS, first-generation DES and newer-generation DES, respectively (p=0.001). Corresponding rates of definite or probable stent thrombosis were 1.3%, 2.1% and 1.1%, respectively (p=0.01). The three-year rate of target lesion revascularisation decreased significantly from 18.6% with BMS to 7.8% with first-generation DES and 6.3% with newer-generation DES (p<0.0001). These results were consistent after multivariable adjustment for potential confounding factors and in subgroup analyses. Overall, the results of this meta-analysis suggest that in women the use of DES compared with BMS is safe and effective and that newer-generation DES have further improved the safety and efficacy profile compared to early-generation DES30. This information provides reassurance regarding the performance of DES in women; however, the benefits must be weighed against the increased safety risk with dual antiplatelet therapy in subjects at risk of bleeding.
TRANSCATHETER AORTIC VALVE IMPLANTATION
Multiple studies have shown that female sex is an independent predictor of worse outcomes after surgical aortic valve replacement (SAVR)31 but conversely is potentially favourable in TAVI. The PARTNER trial demonstrated that, amongst women, there was a trend for procedural mortality to be lower with TAVI versus SAVR (6.8% vs. 13.1%; p=0.07). This finding was maintained throughout follow-up (HR 0.55, 95% CI: 0.32-0.93; p=0.02)32. A recent meta-analysis of randomised clinical trials comparing TAVI versus SAVR, comprising 1,706 women, showed that TAVI patients had a substantial reduction in mortality (31% at one year and 26% at two years)33. The same meta-analysis also suggested that females undergoing TAVI have lower periprocedural mortality and lower rates of bleeding and acute kidney injury. Furthermore, there were lower procedural bleeding rates in women following TAVI than SAVR. Female sex is independently associated with better recovery of left ventricular systolic function following TAVI34. A possible reason for this is that TAVI does not require the sewing ring to be present and hence there is a lower rate of severe prosthesis-patient mismatch (16%) compared with SAVR patients (29%)35. A large meta-analysis of 47,188 patients (49.4% women) undergoing TAVI confirmed a benefit favouring women in all-cause mortality at one year (relative risk [RR] 0.85, 95% CI: 0.79-0.91; p<0.001), with the survival advantage remaining consistent across multiple secondary analyses36. This is probably a consequence of fewer baseline comorbidities, including less CAD prior to undergoing TAVI.
The WIN-TAVI (Women’s INternational Transcatheter Aortic Valve Implantation) registry is the first all-female multinational, prospective, observational registry of women undergoing TAVI for aortic stenosis. The purpose was to investigate the safety and performance of contemporary TAVI and to explore further the influence of female sex-specific factors which have never previously been investigated but may be relevant in the management. Women enrolled were intermediate- to high-risk and experienced a 30-day Valve Academic Research Consortium (VARC)-2 composite safety endpoint of 14.0%. Age, prior stroke, LVEF <30%, TAVI device generation, and history of pregnancy were independent predictors of the 30-day composite safety endpoint37. The primary VARC-2 efficacy composite endpoint occurred in 111 (10.9%) patients beyond 30 days and in 167 (16.5%) patients at one year. The incidence of one-year death or stroke was 13.9%. Prior coronary revascularisation (HR 1.72, 95% CI: 1.17-2.52; p=0.006) indicating established CAD and EuroSCORE I (HR 1.02, 95% CI: 1.00-1.04; p=0.027) were independent predictors of the VARC-2 efficacy endpoint. Of note, after adjustment, no significant association was observed between history of pregnancy or any sex-specific factors and one-year TAVR outcomes38. Finally, lower-risk patients are now a matter of debate and several trials are ongoing. To date, TAVI in intermediate- and high-risk patients has been proven to be more successful in the female sex. Nevertheless, women at low risk may demonstrate the same trend.
TRANSCATHETER ATRIOVENTRICULAR PROCEDURES– MITRACLIP
Sex-related differences in valve pathology, operative strategy, and long-term surgical outcome exist in mitral regurgitation (MR), but not in tricuspid regurgitation (TR)39,40. In MR repair with the MitraClip® device (Abbott Vascular, Santa Clara, CA, USA), implantation is safe and efficacious in both sexes41, irrespective of baseline clinical and echocardiographic differences, despite a trend towards poorer functional improvement among women. Women less frequently receive ≥2 clips, and their mean post-intervention gradient is higher, probably due to lower body surface areas. For tricuspid clipping, the largest series (55% women) showed a 97% success rate, and good clinical results, without assessing sex differences42. No sex-specific guidelines exist for MitraClip implantation; however, current ESC guidelines recommend edge-to-edge repair if the surgical risk is not low with, for primary MR, a ventricular dysfunction and a low likelihood of surgical repair and, for secondary MR, an absence of need for surgical revascularisation, with persisting symptoms despite optimal medical treatment43.
LEFT ATRIAL APPENDAGE OCCLUSION
As in coronary trials, women were under-represented in LAA occlusion trials (33%). Fewer haemorrhagic strokes and cardiovascular/unexplained deaths were observed with LAA occlusion compared to warfarin, with similar rates of stroke or systemic thromboembolism. Subgroup analyses did not show sex-related difference in efficacy and complication rates44.
Indications for catheter-based LAA occlusion do not differ according to sex. Current ESC guidelines recommend LAA occlusion for CHA2DS2-VASc score >2 while the EHRA/EAPCI expert consensus suggests extension to CHA2DS2-VASc score ≥145. Since female sex increases the CHA2DS2-VASc score by one point, women are more likely to fulfil the criteria for LAA occlusion.
ATRIAL SEPTAL DEFECT CLOSURE
Device closure has replaced surgery for secundum defect closure when morphologically feasible (80%) due to lower morbidity and shorter hospital stay, with similar success and mortality rates. Patients benefit from closure at any age in terms of exercise capacity, dyspnoea, and right heart failure, despite lower rhythmic benefit ≥40 years46. No data exist regarding the effect of patient sex. Device closure is preferred for secundum defect closure when applicable. It is particularly indicated in patients with significant shunt and pulmonary vascular resistance <5 WU regardless of symptoms, and in patients with paradoxical embolism47.
Conclusions
This paper from the EAPCI Women Committee (Supplementary Appendix 2) highlights the ongoing issues with the diagnosis and treatment of CAD in women. Differences in the pathophysiology between sexes are summarised, highlighting the need for a greater awareness amongst healthcare professionals to enable the best evidence-based therapies for women and men. Table 2 reports what could be done to improve outcomes in women.
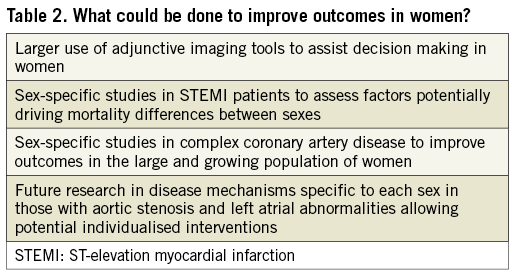
Reassuringly, women are well represented in data concerning TAVI and may actually benefit more than men. Growing evidence is also emerging for other interventional atrial procedures which may well be advantageous to women. Awareness of sex disparities is increasing, and we must all work collaboratively within our profession to ensure that we provide timely and effective care for all patients with both CAD and structural heart disease in the future.
Guest Editors
This paper was guest edited by Roxana Mehran, MD; Mount Sinai School of Medicine, New York, NY, USA, and Alec Vahanian, MD, PhD; Hôpital Bichat-Claude-Bernard and University Paris VII, Paris, France.
Conflict of interest statement
A. Chieffo reports lecture fees from Abbott Vascular, Abiomed, Alvimedica, Biosensors and Cardinal Health. J. Mehilli reports lecture fees from Abbott Vascular, Biotronik, Boston Scientific, BMS, Edwards Lifesciences and Terumo, and institutional grants from Abbott Vascular and Edwards Lifesciences. N. Gonzalo has been a speaker at educational events for Abbott and Boston Scientific. N. Karam is a medical proctor for Abbott. M. Radu reports lecture fees from St. Jude and Abbott Vascular. The other authors have no conflicts of interest to declare. The Guest Editor Roxana Mehran has no conflicts of interest to declare. The Guest Editor Alec Vahanian is a consultant for Edwards Lifesciences.
Supplementary data
Supplementary Appendix 1. Bleeding complications in women undergoing intervention.
Supplementary Appendix 2. EAPCI Women Committee members 2016-2018.
Supplementary Figure 1. Case of an elderly lady undergoing concurrent PCI and TAVI in the setting of cardiogenic shock and pulmonary oedema.
Supplementary Figure 2. Case of a 51-year-old lady presenting with anterolateral STEMI and CAD.
To read the full content of this article, please download the PDF.