The question of increased mortality in women sustaining an acute myocardial infarction (AMI) as compared with men is a recurrent matter of debate. Observational cohorts have repeatedly reported higher mortality rates in women, but how to interpret this increased risk is rendered difficult by the large differences in age (from five to 10 years on average) between men and women hospitalised for AMI1-5; a difference which may be technically difficult to adjust for, despite the use of conventional multivariable analysis techniques. Also, several studies have reported an increased risk in younger women compared with younger men, but not in older individuals1,2.
The current study by Jakobsen et al6 analysed early and long-term outcomes in 7,385 patients getting primary percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI) in Denmark from 2002 to 2008. Overall, women were five years older than men and they had poorer early and long-term outcomes. After adjustment for age and comorbidity, however, the difference in outcomes was no longer significant: adjusted hazard ratios (95% confidence intervals) for death, recurrent MI or stroke 1.16 (0.95-1.41) at 30 days, 1.18 (1.02-1.37) at one year, and 1.14 (0.99-1.30) at two years. Of note, no excess risk was observed in the younger patients. Past the first months following the acute episode, mortality was the same as that of the general Danish population, for women as well as for men. Interestingly, women received the same medications as men during follow-up.
The authors should be commended for an excellent analysis, which indeed has many strengths. Firstly, the study was population-based and used data from a mandatory and audited continuous registry of interventional procedures in Western Denmark. Also, the data were linked with the Danish civil registration system, the Danish transfusion database and the medications reimbursement database; the use of all of these methods ensured complete representativeness of the data reported. Beyond the question raised by the current article, cross-linking of national databases represents a major research tool for assessing the real-world impact of any therapy, and one cannot but regret that this procedure is not allowed in many countries, including France.
The question of how to interpret the present results, however, deserves consideration. At first sight, the conclusions appear extremely encouraging: gender bias seems to have disappeared from the world of cardiology and women with a myocardial infarction have similar outcomes to men. This view, however, is probably overly optimistic and may hide other important, unresolved, issues.
– In their analysis, Jakobsen et al have not analysed temporal trends in compared outcomes in men and women. One does not know whether mortality was similar in both genders from the very beginning of the observation period (2002) or whether the situation progressively improved over the years. In the early 2000s, higher mortality in women was still commonly reported in many countries1,3,4. Whether the Danish situation is country-specific (i.e., there never was a gender bias in the management of STEMI patients in Denmark) or can be extrapolated to other countries therefore remains an open question.
– More importantly, the current analysis is limited to patients undergoing primary PCI within 12 hours of symptom onset. Unfortunately, this reflects a skewed view of the true situation of STEMI patients. In recent observational data in France, as many as 25% of STEMI patients had no reperfusion therapy, mainly because of delayed diagnosis, with only 61% getting primary PCI. Notably, analysing outcomes only for patients undergoing primary PCI does not take into account two key factors: when confronted with chest pain suggestive of myocardial infarction, do women react as quickly as men? Once STEMI is diagnosed, do women get timely primary PCI as often as men? And there is reason there for doubt. In the most recent French registry of myocardial infarction, FAST-MI 2010, the median time from symptom onset to first call was only slightly longer in women (70 minutes versus 65 minutes), but the time from symptom onset to primary PCI was 43 minutes longer in women (298 minutes versus 255 minutes in men). In addition, even after taking into account age, the time from symptom onset to first call, and other potential confounders, primary PCI was performed less often in women (crude rates: 59.5% vs. 67%, p=0.007, adjusted odds ratio: 0.75; 95% confidence interval: 0.57-0.98, p=0.04) (Figure 1). Therefore, the results observed in patients treated with primary PCI do not necessarily reflect the actual way women and men suffering from AMI are treated, and women may still have higher mortality rates if they get less reperfusion therapy. This question may be particularly important for younger patients: previous studies have documented that the excess mortality risk in women was limited to the younger age groups1,2; it has been proposed that myocardial salvage with primary PCI may be greater in women than in men7, and performing primary PCI in a timely fashion in these young patients might therefore be the best way to even the risk between men and women.
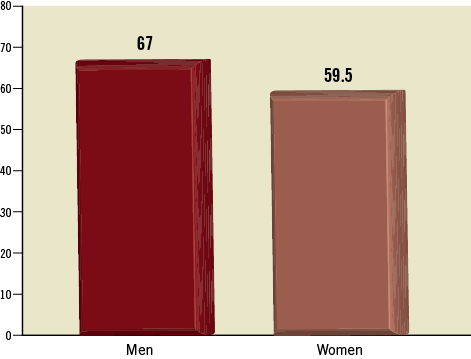
Figure 1. The use of primary PCI according to gender in STEMI patients of the FAST-MI 2010 registry. After extensive adjustment concerning potential confounders, women have 25% less chance of being treated with primary percutaneous coronary interventions. Adjusted OR=0.75; 95% confidence interval: 0.57-0.98; p=0.04
Overall, it is reassuring to observe that Danish women suffering a STEMI have similar outcomes to their male counterparts when treated with primary PCI. It would be more reassuring to know that all women with STEMI are also managed in a similar way and that the situation in Denmark is replicated in other countries as well, as suggested by other registry data8-10.
Conflict of interest statement
N. Danchin received research grants from Astra-Zeneca, Daiichi-Sankyo, Eli-Lilly, GSK, Merck, Novartis, Pfizer, Sanofi-aventis, Servier, and The Medicines Company, and fees as a speaker or consultant for AstraZeneca, Bayer, Bristol-Myers Squibb, Boehringer-Ingelheim, Daiichi-Sankyo, Eli-Lilly, GlaxoSmithKline, MSD-Schering, Novartis, Novo-Nordisk, Pfizer, Roche, Sanofi-aventis, Servier and The Medicines Company. T. Simon received research grants from Astra-Zeneca, Daiichi-Sankyo, Eli-Lilly, Glaxo-Smith-Kline, MSD, Novartis, Pfizer, Sanofi-aventis, Servier, and speaker and consulting fees from AstraZeneca, Bayer-Schering, Eli-Lilly, Sanofi-aventis.

