bstract
Aims: The relationship between the predictive performance of the TIMI risk score for STEMI and gender has not been evaluated in the setting of primary PCI (pPCI). Here, we compared in-hospital mortality and predictive performance of the TIMI risk score between Belgian women and men undergoing pPCI.
Methods and results: In-hospital mortality was analysed in 8,073 (1,920 [23.8%] female and 6,153 [76.2%] male patients) consecutive pPCI-treated STEMI patients, included in the prospective, observational Belgian STEMI registry (January 2007 to February 2011). A multivariable logistic regression model, including TIMI risk score variables and gender, evaluated differences in in-hospital mortality between men and women. The predictive performance of the TIMI risk score according to gender was evaluated in terms of discrimination and calibration. Mortality rates for TIMI scores in women and men were compared. Female patients were older, had more comorbidities and longer ischaemic times. Crude in-hospital mortality was 10.1% in women vs. 4.9% in men (OR 2.2; 95% CI: 1.82-2.66, p<0.001). When adjusting for TIMI risk score variables, mortality remained higher in women (OR 1.47, 95% CI: 1.15-1.87, p=0.002). The TIMI risk score provided a good predictive discrimination and calibration in women as well as in men (c-statistic=0.84 [95% CI: 0.809-0.866], goodness-of-fit p=0.53 and c-statistic=0.89 [95% CI: 0.873-0.907], goodness-of-fit p=0.13, respectively), but mortality prediction for TIMI scores was better in men (p=0.02 for TIMI score x gender interaction).
Conclusions: In the Belgian STEMI registry, pPCI-treated women had a higher in-hospital mortality rate even after correcting for TIMI risk score variables. The TIMI risk score was effective in predicting in-hospital mortality but performed slightly better in men. The database was registered with clinicaltrials.gov (NCT00727623).
Introduction
Cardiovascular disease is the major cause of death in women over the age of 65. Since the early nineties, higher mortality rates have been reported for women with ST-segment elevation myocardial infarction (STEMI) as compared to men1-7. The poorer outcome in women has been attributed to a higher age, more advanced disease, more comorbidities, longer ischaemic times, worse clinical condition on presentation and the underuse of evidence-based therapy and invasive reperfusion strategies1,8. Several authors have demonstrated that sex-related mortality differences are confined to younger patients, typically those younger than 50 years of age5,9,10. Despite the fact that primary PCI (pPCI) improves outcome in STEMI in both men and women11, as confirmed by the current guidelines12, there is conflicting evidence regarding gender-based differences in the short-term outcome of women treated with pPCI. In 2001, Vakili et al demonstrated that women treated with primary PCI for a first STEMI still had a higher risk of death as compared to men13. This finding was confirmed in some studies14,15, while others found no significant sex-related differences in early mortality3,16-21.
The Thrombolysis In Myocardial Infarction (TIMI) risk score for STEMI is a simple arithmetic score that predicts short-term mortality based on age and clinical data on admission22. This score was initially developed and validated in a randomised controlled trial of patients treated with fibrinolysis, but proved to be useful in patients treated with primary PCI in an observational registry (c-statistic=0.80 for patients treated with primary PCI in the NRMI III registry [n=15,348])23. Ten baseline variables accounted for 97% of the predictive capacity and were constituted in the TIMI risk score. Female gender was not included in the TIMI risk score, as it was one of the five variables accounting for the remaining 3% of the predictive capacity for 30-day mortality (OR 1.2; 95% CI: 1 to 1.2). There are no data on the predictive performance of the TIMI risk score when applied to a community-based cohort of men and women in the current era of pPCI, stenting and contemporary adjunctive antiplatelet therapy.
Accordingly, we compared the in-hospital mortality rate and predictive performance of the TIMI risk score between male and female Belgian STEMI patients undergoing pPCI.
Methods
BELGIAN STEMI REGISTRY
The Belgian STEMI registry is a prospective observational registry of unselected Belgian STEMI patients from 72 Belgian hospitals. STEMI was defined as follows: symptoms suspicious of acute coronary syndrome, combined with ST-elevation (>1 mm in two contiguous leads), or new left bundle branch block on ECG. The registry contains demographics (post code, PCI vs. non-PCI centre), previous history (diabetes, hypertension, peripheral artery disease, coronary artery disease), clinical characteristics at admission (weight < or ≥67 kg, admission blood pressure < or ≥100 mmHg , admission heart rate > or ≤100 bpm), infarct localisation (anterior, LBBB, non-anterior), practice patterns (treatment, transfer, ischaemic and intervention times) and in-hospital outcomes. Ischaemic time is defined as the time between onset of symptoms and revascularisation therapy. The registry is an initiative from the Belgian Working Group on Acute Cardiology (BIWAC) and supported by the Belgian government and the Belgian College of Cardiologists. All Belgian cardiologists working in hospitals with acute care facilities were required to prospectively collect data on all admitted STEMI patients starting from January 2007. Since a patient file can only be finalised when all required data are provided, there are no missing covariates in the registry. The database was registered with clinicaltrials.gov (NCT00727623). This study was approved by the central ethical committee of the Ghent University Hospital (2011/455). Informed consent was obtained from all patients or their legal representatives.
During the period between January 2007 and February 2011, a total of 9,535 STEMI patients from 72 hospitals (25 with PCI facilities and 47 without PCI facilities) were prospectively included. Of these, 8,073 (84.67%) patients were treated with primary PCI <24 hours after hospital admission and included in the analysis. Patients receiving rescue PCI after failed thrombolysis (N=272, 2.85%) were not included in the PCI group, while patients who underwent facilitated PCI (N=231, 2.42%) were included in the PCI group. A yearly audit, conducted by an external commission, of 10% of all patient files was performed to verify the validity of the data. Data were electronically collected via a protected eCRF. The database is managed by an independent electronic data capture provider (Lambda Plus, SA, Gembloux, Belgium).
CLINICAL ENDPOINTS
The primary endpoint of the study was in-hospital mortality.
TIMI RISK SCORE
The TIMI risk score was automatically calculated from eight differentially weighted clinical indicators ascertained upon admission. The TIMI score ranges from 0 to 14 and is calculated as follows: age (2 points: 65-74, 3 points: 75 and older); history of angina, diabetes or hypertension (1 point); admission systolic blood pressure (BP) <100 mmHg (3 points); admission heart rate (HR) >100 beats/min (bpm) (2 points); admission Killip class >I (2 points); admission weight <67 kg (1 point); anterior infarction or left bundle branch block LBBB (1 point); and time to reperfusion therapy >4 hours (1 point)22.
STATISTICAL ANALYSIS
We compared the baseline characteristics and in-hospital outcomes of women with those of men. Categorical variables were compared with the Fisher’s exact test. Continuous variables were evaluated for normality. The Student’s t-test was used for continuous variables with a normal distribution (presented as the mean±SD), and Mann-Whitney U test was used for continuous variables (presented as the median and interquartile range [IQR]) without a normal distribution.
We created a multivariable logistic regression model to evaluate the relationship between gender and in-hospital mortality, including all TIMI risk score variables: age group (< and ≥65 years of age), history of hypertension, history of diabetes, previous coronary artery disease [CAD], Killip class >I, ischaemic time >4 hours, admission BP <100 mmHg, admission HR >100 bpm, weight <67 kg, anterior myocardial infarction or LBBB). Female gender was added to this multivariable model. Odds ratios (OR) with 95% confidence intervals (CI) are reported. Statistical significance was defined as p<0.05 or CI for OR that did not include 1.0.
The predictive discriminatory capacity of the TIMI risk score was expressed as the c-statistic, which represents the area under the ROC (receiver operating characteristic: 0.50 indicating chance discrimination and 1.00 perfect discrimination) curve for predicting in-hospital mortality in both men and women. Calibration was assessed by using the Hosmer-Lemeshow goodness-of-fit test; a p-value >0.05 was prespecified as good calibration. We established a logistic model for in-hospital mortality, including the TIMI risk score, gender and an interaction term between both.
All statistical analyses were performed using the PASW 18 statistical software (SPSS Inc., Chicago, IL, USA).
Results
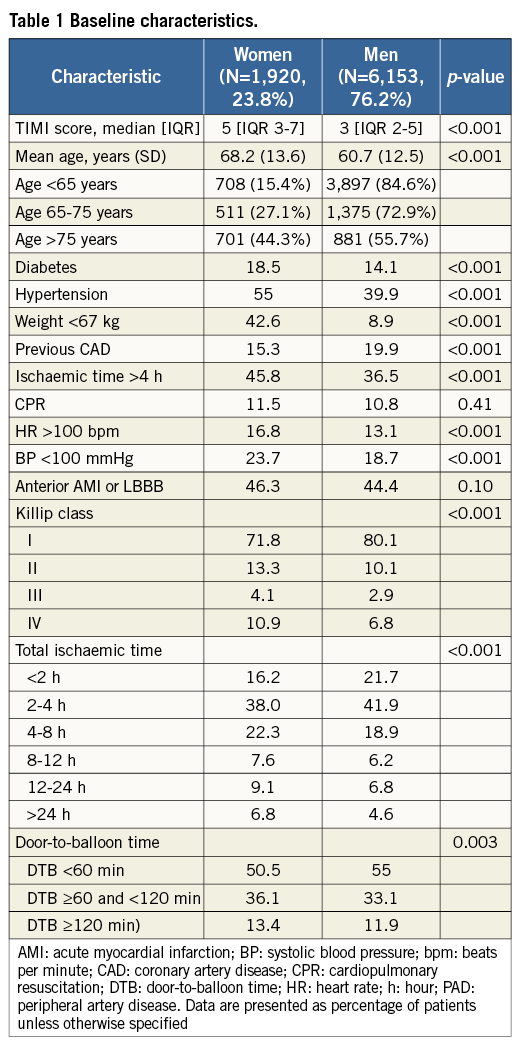
BASELINE CHARACTERISTICS
Baseline patient characteristics are shown in Table 1. During the period between January 2007 and February 2011, 8,073 patients were treated with primary PCI: 1,920 (23.8%) were female and 6,153 (76.2%) were male. TIMI risk scores at admission were higher in women vs. men (TIMI: median 5 [IQR 3-7] vs. 3 [IQR 2-5], p<0.001). As compared to men, the women were older (mean age 68.2 vs. 60.7 years, p<0.001) and more had diabetes (18.5% vs. 14.1%, p<0.001), hypertension (55% vs. 39.9%, p<0.001) and body weights <67 kg (42.6% vs. 8.9%, p<0.001). Furthermore, fewer of these women had previous CAD as compared to men (15.3% vs. 19.9%, p<0.001). Women had longer total ischaemic times (ischaemic time >4 hours in 45.8% of the female patients vs. 36.5% of the male patients, p<0.001). The need for CPR was not different between women and men (11.5% vs. 10.8%, p=0.41). The Killip class at admission was higher in women vs. men (Killip >I: 28.3% vs. 19.9%, p<0.001). Women also experienced longer door-to-balloon times (DTB) as compared to men: DTB <60 min: 50.5% vs. 55%, DTB ≥120 min: 13.4% vs. 11.9% (p=0.003).
GENDER AND IN-HOSPITAL MORTALITY
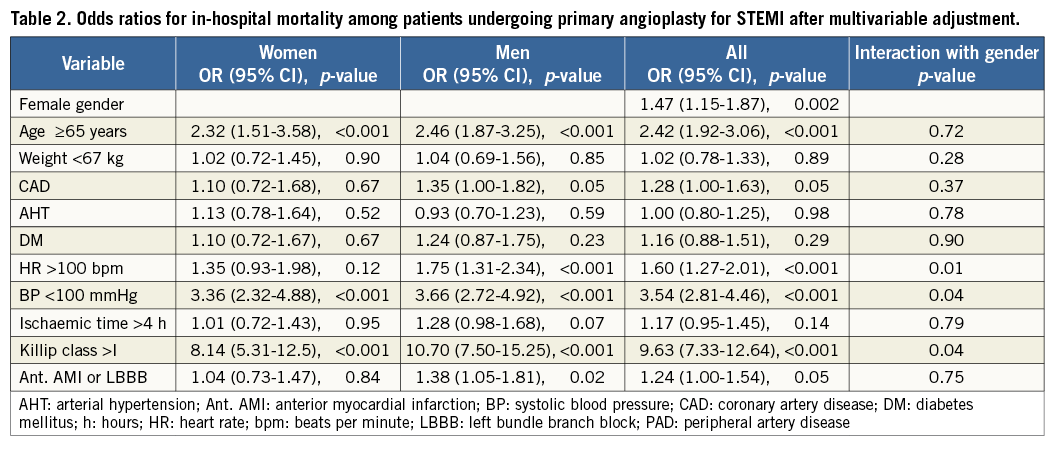
The in-hospital mortality rate for the entire cohort of pPCI-treated patients was 6.1%. Crude mortality data show that mortality was double in invasively-managed Belgian women with STEMI as compared to men (10.1% vs. 4.9%; OR 2.2; 95% CI: 1.82 to 2.66, p<0.001). In a multivariable regression model, adjusting for TIMI risk score variables and gender, the disparity in the risk of death between men and women persisted (OR 1.47; 95% CI: 1.15 to 1.87, p=0.002). Age ≥65 (OR 2.42; 95% CI: 1.92 to 3.06, p<0.001), HR >100 bpm at admission (OR 1.60; 95% CI: 1.27 to 2.01, p<0.001), BP at admission <100 mmHg (OR 3.54; 95% CI: 2.81 to 4.46, p<0.001), known CAD (OR 1.28; 95% CI: 1.00-1.63, p=0.05) and a Killip class >I (OR 9.63; 95% CI: 7.33 to 12.64, p<0.001) were other independent predictors of in-hospital mortality, while hypertension (OR 1.00; 95% CI: 0.80 to 1.25, p=0.98), diabetes (OR 1.16; 95% CI: 0.88 to 1.51, p=0.29) and an ischaemic time >4 hours (OR 1.17; 95% CI: 0.95 to 1.45, p=0.14) were not. Interaction tests for the individual TIMI risk score variables and gender demonstrated that an admission heart rate >100 bpm, an admission systolic blood pressure <100 mmHg and a Killip class >I had more effect on mortality in male than in female patients (Table 2).
GENDER AND TIMI RISK SCORE PERFORMANCE
The median TIMI risk score for all patients treated with primary PCI was 4; women had a higher median TIMI risk score than men (TIMI score 5 [IQR 3-7] vs. 3 [IQR 2-5]). More than half of the men, versus only a quarter of the women, had a TIMI risk score below 4 (54.1% vs. 27.6% of the women). Almost 17% of the women had a very high TIMI risk score (>8) as compared to only 7.5% of the men (Figure 1).

Figure 1. TIMI risk score distribution in men and women. TIMI: the Thrombolysis In Myocardial Infarction (TIMI) risk score for STEMI. Calculation of TIMI score (0-14): age (2 points: 65-74, 3 points: 75 and older); history of angina, diabetes or hypertension (1 point); admission systolic blood pressure (BP) <100 mmHg (3 points); admission heart rate (HR) >100 beats/min (bpm) (2 points); admission Killip class >I (2 points); admission weight <67 kg (1 point); anterior infarction or left bundle branch block (LBBB) (1 point); time to reperfusion therapy >4 hours (1 point). Red bars: men; pink bars: women.
The in-hospital mortality rate increased with increasing TIMI risk scores in both women and men (Figure 2). The mortality rate difference between men and women was the highest for low TIMI risk scores (TIMI score ≤4) and in patients with TIMI scores >8. The mortality rate in women was higher for almost all TIMI risk scores.
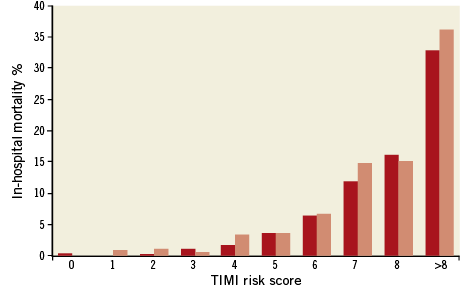
Figure 2. In-hospital mortality by TIMI risk score in male and female patients. TIMI: the Thrombolysis In Myocardial Infarction (TIMI) risk score for STEMI. Calculation of TIMI score (0-14): age (2 points: 65-74, 3 points: 75 and older); history of angina, diabetes or hypertension (1 point); admission systolic blood pressure (BP) <100 mmHg (3 points); admission heart rate (HR) >100 beats/min (bpm) (2 points); admission Killip class >I (2 points); admission weight <67 kg (1 point); anterior infarction or left bundle branch block (LBBB) (1 point); time to reperfusion therapy >4 hours (1 point). Red bars: men; pink bars: women
The TIMI risk score provided a good prognostic discrimination of mortality among both women (c=0.84 [95% CI: 0.809-0.866]) and men (c=0.89 [95% CI: 0.873-0.907]). The TIMI risk score calibration was good in both genders with a Hosmer-Lemeshow goodness-of-fit of 0.53 in women and 0.13 in men. When comparing mortality rates for TIMI risk scores between women and men, with an interaction term for TIMI score and gender, we found that mortality prediction for TIMI scores was better in men compared to women (p=0.02 for TIMI score x gender interaction).
GENDER AND AGE
The <65 years of age group (n=4,605) comprised 708 (18.3%) female patients, as compared to 1,212 (34.9%) female patients in the ≥65 years of age group (n=3,468). Adjusting for TIMI risk score variables (except age ≥65 years) and gender demonstrated a sustained association between female gender and mortality in both age groups (<65 years of age: 1.71 [1.05-2.77, p=0.03]; ≥65 years of age: 1.39 [1.05-1.83, p=0.02]). After further adjustment for age in these age groups female gender remained a predictor for mortality in the <65 years of age group (<65 years: 1.73 [1.07-2.82, p=0.03]) but not in the ≥65 years of age group (≤65 years: 1.27 [0.96-1.68, p=0.09]).
GENDER AND BODY WEIGHT
Overall, 60% of the patients with body weights <67 kg and 16.4% of the patients with body weights ≥67 kg were women. The adjusted mortality difference between women and men remained significant in the subgroup with body weights ≥67 kg (OR 1.55; 95% CI: 1.16 to 2.06, p=0.003) but not in the subgroup with body weights <67 kg (OR 1.29; 95% CI: 0.82 to 2.01, p=0.27).
Discussion
There is ongoing debate as to whether gender itself is an independent predictor of in-hospital mortality in STEMI patients undergoing primary PCI, and the relationship between the predictive performance of the TIMI risk score for STEMI and gender has not been evaluated in this setting.
We demonstrated that female patients, from a nationally representative (Belgium) community-based registry of 8,073 consecutive STEMI patients reperfused by pPCI, had a higher in-hospital mortality rate than men. Even after adjusting for the baseline risk variables of the TIMI risk score for STEMI, the risk of dying remained almost 50% higher in women. We showed that the TIMI risk score for STEMI, which weights these different risk factors, demonstrated a good prognostic discrimination and calibration in both men and women, but the mortality prediction for TIMI risk score was better in men.
Several factors may contribute to the worse outcome of women experiencing a STEMI. First, women are older and have more comorbidities, including diabetes and hypertension, and this has been observed consistently in different trials and registries7. Women seek treatment with later-stage STEMI24 and suffer longer door-to-balloon/-needle times25, resulting in longer ischaemic times and more myocardium at risk26. Women generally have a lower body weight and hence a lower BSA, which is not only a risk factor for bleeding complications after PCI27, but is also associated with a higher mortality. This is also known as the “obesity paradox”28. Less frequent use of evidence-based management therapies, including invasive management, more extensive coronary artery disease and smaller coronary arteries, or a higher risk of periprocedural complications may also contribute to their poorer outcome8,25. In general, the question remains whether gender-related differences in outcome would persist if both men and women presenting with STEMI received the same evidence-based management, including primary PCI, as the current standard. This question has been addressed by several investigators during the last two decades. However, sample sizes were often small, and these studies do not always reflect the current standards of stenting and adjunctive antiplatelet therapy.
We demonstrated that an age >65 years is an important predictor of mortality. A significant gender-related mortality rate difference was observed in the <65 years of age group as well as in the ≥65 years of age group. After further adjustment for age in these age groups, the mortality gap persisted in the <65 years of age group, suggesting that age alone does not fully explain the difference in outcomes between women and men, especially not in the patient group <65 years of age. Moreover, the mortality gap in this group warrants close monitoring of these women in the acute phase.
Although diabetes and hypertension are two of the main risk factors for developing an acute coronary syndrome, these conditions were not independent predictors of in-hospital mortality, either for the entire cohort or separately between women and men. The fact that diabetes was not associated with increased in-hospital mortality might be explained by a greater risk reduction with primary PCI in diabetic patients as compared to non-diabetic patients29, and this is consistent with the findings of Meisinger et al who showed only an association with long-term mortality, particularly in women30. There appeared to be no clear association between a history of hypertension and in-hospital mortality among STEMI patients. We presume that many patients with known hypertension already receive adequate treatment, including cardio-protective medication (ACE-inhibitors, statins, aspirin), while patients with unknown hypertension were classified in the registry as having no history of hypertension31,32. Although more prevalent among women, diabetes and hypertension also did not account for the higher in-hospital mortality among women in our population.
We confirmed that women sought treatment with later-stage STEMI as compared to men and experienced longer door-to-balloon times, which resulted in longer total ischaemic times. One of the reasons behind this later presentation is the lack of typical chest pain, especially in younger women suffering a myocardial infarction, as was recently demonstrated in the National Registry of Myocardial Infarction33. Another problem is the lack of awareness at the physician level: doctors can be misled by this atypical presentation and/or underestimate the possibility of an acute coronary syndrome, especially in young women. This may lead to delays in diagnosis and treatment as well as suboptimal treatment. Other reasons for the later-stage presentation and longer door-to-balloon time remain unclear but are one of the reasons behind awareness campaigns addressing females around the world. After multivariable analysis, an ischaemic time >4 hours was not an independent predictor of in-hospital mortality; however, an ischaemic time >4 hours may influence other TIMI variables, such as Killip class and haemodynamic compromise.
Finally, female Belgian STEMI patients more frequently had a body weight <67 kg and were sicker on admission, as reflected by their higher Killip class and prevalence of admission hypotension and tachycardia. Correction for all of these differences, all included in the TIMI risk score, also failed to explain the differences in in-hospital mortality rates between men and women. However, interaction tests for each predictor with gender demonstrated that a HR >100 bpm, a BP <100 mmHg and a Killip class >I had more effect on mortality in men than in women.
After correction for all of the TIMI risk score variables, the mortality rate remained significantly higher in women as compared to men. On the other hand, our analysis showed that the TIMI risk score provides good predictive discrimination in both genders in a community-based population treated with primary angioplasty. The mortality prediction for TIMI risk score was slightly better in men. However, as pointed out by Vergouwe et al34, comparing c-statistics between groups may be biased by the variation in risk profiles in these groups; the tighter interquartile range in the TIMI risk score distribution in men compared to women seems rather inconsistent with this explanation. There seemed to be a stronger impact of admission hypotension, admission tachycardia and a Killip Class >I on mortality in men (Table 2).
Despite the fact that the TIMI risk score was developed and validated in a randomised controlled trial of fibrinolysis, it is still a valuable tool to predict early mortality in currently treated male and female STEMI patients. It remains unclear whether the worse baseline haemodynamic profile in women (HR >100 bpm, BP <100 mmHg and Killip >I), good for seven points in the TIMI risk score, could be improved by reducing ischaemic times, and what impact this would have on gender differences in outcome after STEMI.
Strengths and limitations
This relatively large registry offers a “real-life” view of the men and women treated with primary PCI. Several limitations need to be considered when interpreting the results. First, the data were examined using risk adjustment models; however, we cannot exclude other confounding factors that were not registered, such as renal function, lipid status, smoking habits, coronary anatomy, TIMI flow rates, success of PCI, periprocedural complications, treatment (anticoagulation, antiplatelet agents, β-blockers, ACE inhibitors, statins), or other unrecognised differences. Second, the characterisation of some continuous important characteristics (body weight < or ≥67 kg, ischaemic time, blood pressure and heart rate) into dichotomies was inherent to the registry and may have introduced residual confounding and hence biased our results to some extent. Third, we only collected data on in-hospital mortality rates; hence, it remains unclear whether our results can or cannot be extrapolated to long-term outcomes. Furthermore, a referral bias for invasive evaluation is not excluded: secondary care centres that do not routinely apply pPCI for STEMI may refer only the most severely ill patients for urgent PCI. We found no significant differences in the baseline characteristics in female patients admitted in PCI vs. non-PCI hospitals to support this possibility. Finally, underreporting cannot be excluded despite the fact that the registry design called for consecutive enrolment of all STEMI patients.
Conclusions
Analysis of the Belgian STEMI registry demonstrates that almost a quarter of all patients treated with primary PCI for ST-segment elevation myocardial infarction comprised women. In-hospital mortality rates of PCI-treated female STEMI patients were higher as compared to their male counterparts, even after adjustment for TIMI risk score variables. The TIMI score for STEMI proved to have a good predictive performance in both women and men in predicting in-hospital mortality rates in currently pPCI-treated patients; however, this predictive performance was slightly better in men than in women. The TIMI risk score remains a reliable and simple bedside score suitable for early risk stratification, in women as well as in men. Reducing the time delays remains one of the most important modifiable factors that could improve TIMI risk scores and outcomes in women. This stresses the need for continuous awareness campaigns, especially in younger women, but also in the physicians confronted with these patients.
Acknowledgements
The authors thank Mrs Lisa Hobbs, former secretary of the Belgian Society of Cardiology, for her administrative support.
Funding
The National STEMI Database is financially supported by a grant from the Ministry of Public Health of the Belgian government.
Conflict of interest statement
The authors have no conflicts of interest to declare.