Do you show the angiographic result to your patient at the end of the procedure? Why not? It takes two minutes and the images are so easy to interpret that the patient quickly understands what the problem was and how it was “fixed”. We often use that word, “fixing”, but is it right? Certainly not. It gives the idea of a pipe replaced restoring normal functionality in an appliance. Unfortunately the human body is somewhat more complicated than a dishwasher and the ruptured plaque leading to an acute coronary syndrome is only the last step of a process of wall encroachment starting soon after birth. The message we convey to our patients can, therefore, be misleading. “You had a serious problem, Sir, but now it is solved, you are a new man, forget it and go back enjoying life”.
One of the big advantages of angioplasty (PCI) in acute coronary syndromes is the ability to offer a treatment requiring one day of hospitalisation for an unstable syndrome and 2-3 days in most cases with ST-segment elevation myocardial infarction, patients who used to stay in bed one month till 30-40 years ago and still spend 7-10 days in hospital where primary PCI and routine early PCI after thrombolytics is not commonplace. When timely applied in acute coronary syndromes, PCI is one of the few new medical interventions which is both life-saving and cost-saving.1 A structured secondary prevention programme, aimed at risk stratification and modification, is scarcely applied. Most patients simply go home with the advice to take it easy for one to two days if they had a femoral puncture, regularly assume standard doses of beta blockers, ACE-inhibitors, aspirin, clopidogrel and statins, often without discussing their importance and side effects. If they are lucky, a member of the junior medical staff or a nurse in the ward will mumble a few words before discharge about smoking, healthy diet, control of pressure, body weight, diabetes and cholesterol. All the rest is left to their GP or their local attending cardiologists, often doctors the patients have never seen before because their heart attack was the first medical event of note for many years.
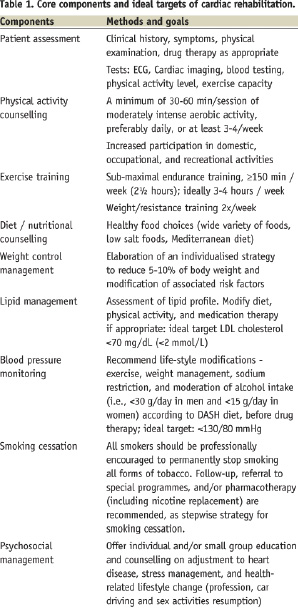
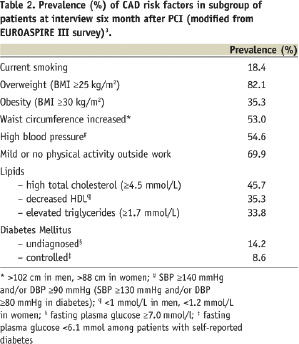
Table 1 is a simplified presentation of the present recommendation of the European Association of Prevention and Rehabilitation (EACPR) for secondary prevention in patients with known coronary artery disease (CAD).2 Achieving these goals can dramatically reduce the incidence of death and new coronary events for these high risk patients. But, how many of our patients treated with PCI are going to achieve these goals when all our support is three lines in a discharge summary? Some information can be derived from the EUROASPIRE III study3. The data from 13,935 patients with CAD (5,494 PCI patients) in 76 centres all around Europe were surveyed to determine whether the Joint European Societies’ guidelines on cardiovascular prevention4 have been applied in clinical practice. Table 2 documents the persistence of uncontrolled risk factors in the subgroup undergoing PCI. The results are truly disappointing: most patients do not hit one or more targets that have been demonstrated to prolong life. Only a minority of the population achieve effective control of blood pressure and/or adequate reduction of serum cholesterol, and only 8.6% of the diabetic patients control their glycaemic levels. It is not just a matter of doses of drugs. The real problem is our incapacity to convince patients to change their lifestyle: in the EUROASPIRE survey, only 68% of the smokers admitted to have effectively quit, and only 62% reported to have significantly increased their physical activity and 60% to have lost some weight after the PCI. These data are based on self-reported questionnaires and thus we have to trust their honesty.
Exercise based cardiac rehabilitation and the institution of a secondary prevention individualised program are a generally accepted component of long-term therapy after surgical revascularisation and has achieved Class of Recommendation 1, Level of Evidence B showing in multiple studies that they reduce future morbidity and mortality associated with the atherosclerotic process5. Unlike surgical coronary revascularisation, based on the use of arterial or venous conduits bypassing the proximal segments of the main epicardial vessels, PCI is critically dependent on the achievement of an effective interruption or the induction of a significant delay of the otherwise natural process of disease progression. The PROSPECT trial (Providing Regional Observations to Study Predictors of Events in the Coronary Tree), recently presented at TCT in San Francisco6, offers an updated confirmation that more than half (11.6%) of the three year MACEs (20.3% cumulative incidence of death, cardiac arrest, myocardial infarction, unstable or recurrent angina) is caused by lesions originally not treated during PCI. This trial, along with others soon to follow, take advantage of the improved resolution of new imaging modalities such as OCT7. These imaging modalities are aimed at the identification of plaques at so high a risk that the common preventive measures are insufficient to stabilise them before new events develop. In our main congresses we spend considerable time and resources and dedicate long sessions to the search for the holy grail of still unproven local mechanical interventions of plaque stabilisation. We dedicate no time and plan no research studies to improve efficacy of an intervention proven to offer a big long-term advantage to all patients with CAD and in particular to patients post-PCI, the humble prevention. When a patient has a new myocardial infarction, two years after PCI due to a new lesion, he/she doesn’t care that the previously implanted DES is perfectly patent because their cardiologist is fully aware of the recent trial results and has picked up a second generation DES able to reduce by 2% the risk of target lesion failure; an artificial, purely device-oriented endpoint, of some new trials8. They and their GPs will consider the event a complication of the initial treatment strategy and will advise their neighbour, relative or patients to undergo surgery in similar circumstances.
Sometimes, interventionalists spend too much time in the ivory towers of their catheterisation laboratories and not enough in the ward or in the outpatients’ clinic. Attention to technical details, achieving optimal stent deployment and expansion, especially in complex lesions, is of critical importance. We should not forget, however, that in CAD management, myocardial revascularisation is only a palliative treatment. To offer lasting results to our patient we must look back from the heights of our sophisticated technologies to the ABC of secondary prevention (or in fact to the “ABCDE”, where “A” stands for antiplatelet therapy, anticoagulation, angiotensin converting enzyme inhibition, and angiotensin receptor blockade; “B” for beta-blockade and blood pressure control; “C” for cholesterol treatment and cigarette smoking cessation; “D” for diabetes management and diet; and “E” for exercise)9. I have seen hospitals where cholesterol is not routinely measured upon admission for PCI with the excuse that “it is anyway modified by the acute coronary syndrome” or “lipid lowering treatment is somebody else’s responsibility”. Weight is measured to adjust the heparin or the bivalirudin doses, but the importance of a hypocaloric diet and regular exercise is never stressed. How much attention will the patient pay later to the advice of his GP or clinical cardiologist when his “saviour”, the skilled physician who suddenly made his acute chest pain disappear, did not even mention the critical importance of the control of these factors?
New cardiac patients following an acute event deserve special attention. They all, businessmen and builders alike, are afraid that this sudden event can impair for ever their quality of life, work capacity, sexual activity, long-term life plan. They are confused, standing between depression and denial and they often misinterpret our words: “the doctor said that my problem is fixed”. Many of them may not need a traditional cardiac rehabilitation program as outpatients or in a rehabilitation centre. All of them require counselling to prevent event recurrence, by adhesion to a medication plan and adoption of a healthy lifestyle. Education should be interactive with full participation of patient care-givers, providing explanation for each pharmacological and life-style intervention while mobilisation and physical conditioning programme should vary according to individual clinical status. Comprehensive risk factor modification programmes with regular follow-up are essential to bring patients to target goals, and have been showed to be cost-effective in terms of costs per year life saved, comparing favourably with other well-established preventive and therapeutic intervention tools in the treatment of CAD such as thrombolysis, mechanical revascularisation with PCI or surgery or ICD implantation.10 No wonder that indications for secondary prevention in post-PCI and surgical myocardial revascularisation have been further emphasised in recent guidelines.11-14
In many European countries interventional cardiologists successfully led the recent revolution of the widespread adoption of primary PCI. They convinced other key medical players such as acute care cardiologists and physicians and the emergency ambulance service to drastically change previous practices.15 We need a similar revolution in prevention after PCI, joining forces with cardiac rehabilitation specialists, other clinical cardiologists and GPs.
Our associations, part of the European Society of Cardiology (ESC) family, are optimally positioned to lead this cooperative effort, with common education initiatives planned during the respective association congresses and the ESC congress. It is a necessary cultural revolution to recognise the interdependency of our specialities, while always keeping in mind the priority of optimal care of our patients. A first step has been the recognition in the Core Curriculum of the European Cardiologists, all of them, interventionalists included, of the knowledge of secondary prevention and rehabilitation. Specific registries are required to monitor outcome measures such as global cardiovascular risk control, clinical stability and symptoms control, level of independency, adherence to therapeutic prescription and to beneficial life style changes. Strategies to ensure a smooth transition and immediate interactive communication between the interventional cardiologist in the acute care hospital, the local clinical cardiologist and GP must be developed and tested. It will certainly benefit all our patients, and benefit interventional cardiology as well, breaking through our present unnatural isolation from the other active components of the cardiological and medical community.

