During the last 20 years, primary PCI has evolved from being an almost experimental intervention to becoming a routine job performed around the clock, as commonplace as a general surgeon operating on an acute appendicitis, or a traumatologist reducing an exposed fracture.
At this point in time, the primary PCI technique has evolved from a simple, prudent inflation of balloons, to the administration of complex drug cocktails, routine implantation of stents, aggressive manipulation of thrombus, amazing intravascular imaging, and to concepts such as preconditioning and even recovering of dead myocardial tissue with cardiopoietic regenerative therapy.
Nevertheless, reviewing a primary PCI performed in March 1993 (Figure 1A-Figure 1C), and one performed 20 years later, by the same operator, in April 2013 (Figure 1D-Figure 1F), there seems to be very little if any difference in the global concept of the procedure.
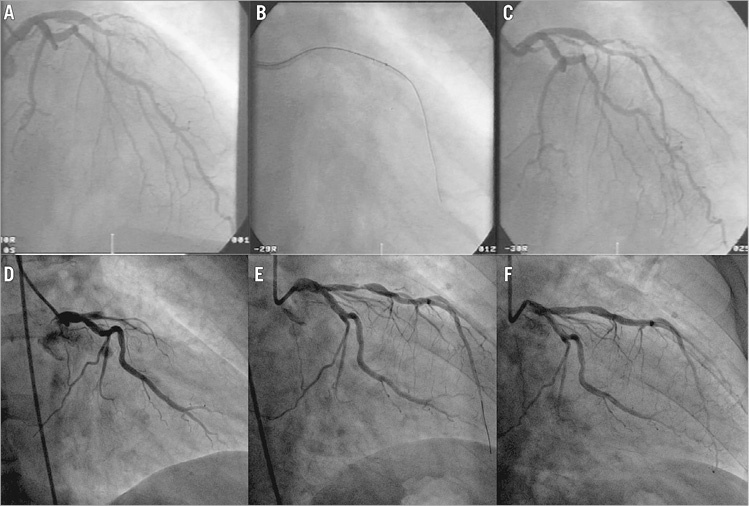
Figure 1. Primary PCI procedures performed 20 years apart. A) Right anterior oblique angiographic image showing a thrombotic, acute, total occlusion of the left anterior descending coronary artery causing a large anterior STEMI on March 31st 1993. B) Balloon dilatation at the site of the occlusion. C) Recanalised vessel after balloon angioplasty. D) Right anterior oblique angiographic image showing a thrombotic, acute, total occlusion of the left anterior descending coronary artery causing a large anterior STEMI on April 18th 2013. E) Vessel recanalisation after manual thrombus aspiration. D) Final result after direct implantation of a 3.5×18 mm Absorb scaffold and post-dilation with a 3.5 mm non-compliant balloon.
Indeed, apart from the significant shifts from the femoral to the radial vascular access, a strategy potentially reducing mortality in STEMI patients, and the use of manual thrombus aspiration catheters in selected cases, another simple act that might reduce one-year mortality, everything else looks more or less the same as it did 20 years ago –a guiding catheter, a guidewire, a balloon, and a stent…
This supplement provides the reader with a “state-of-the-art” vision of reperfusion therapy as it stands in 2014. It develops important topics such as the role of thrombus aspiration1 and new dedicated stents2, PCI in the patient presenting with multivessel disease3, the role of FFR in acute coronary syndromes4, the management of patients with cardiogenic shock5, the role of new antithrombotic drugs6, and an update of the guidelines accompanied by thoughtful comments by experts7. In addition, it also tries to envisage what is, or could be, the next step, the next frontier.
The future of reperfusion treatment poses two different challenges: one is massive and concrete and is that of extending the population actually treated in a timely manner in a world where deep socio-economic discrepancies have started to change, as analysed in the section dedicated to the STEMI systems in emerging countries prepared by the leaders of the SFL Initiative8.
The other challenge, implicit in the spirit of science itself, is the willingness of daring against limits, aiming at what today seems impossible: this is, on the one hand, restoring the vessel wall and “leaving nothing behind…” and, on the other hand, disclaiming cell death itself, by seeding progenitor cells to regain living muscular tissue.
Experience, technology and scientific advances in this field have offered new alternatives to doing the same thing in many different ways, although the mission clearly remains the same: leaving anything else and rushing to open the occluded artery, to save muscle, to save life. In a world that changes so rapidly and that offers so many options to change, it becomes essential for the future to understand the difference between real advances and non-determinant variations that we like to call “exercises in style”.
Exercises in style is the English translation of a masterpiece of French literature written by Raymond Queneau in 1947 which tells the simple story of a man seeing the same stranger twice in one day9. It tells that same short story in 99 different ways, demonstrating the variety of styles in which storytelling can take place. In each, the narrator gets on the “S” bus, witnesses an altercation between a man with a long neck and funny hat and another passenger, and then sees the same person two hours later at the Gare Saint-Lazare getting advice on adding a button to his overcoat. The story itself is as simple as it is absurd, and this simplicity is intentional so as not to confuse the reader with the story itself, but to concentrate on the different iteration of the same tale as the real message.
Among the 99 different manners of telling the same story, the author includes some styles that bring to mind our common thinking and daily “interventional speak”. Some examples of Queneau’s proposed styles are: “retrograde”, “double entry”, “futile”, “surprise”, “precision”, “hesitation”, “more or less”, “animism”, “feminine”, “telegraphic”, “unexpected”, “insistent”, “awkward”, “gallicisms, italianisms, anglicisms”, “dreams” and so forth, up to providing us with 99 different forms of the same act.
By analogy, over more than 20 years technical progress has enriched the re-telling of the primary PCI story without changing its content much. The real story remains the same, i.e., opening the vessel as soon as and “as opened” as possible. Most of the additional iterations have proved to be more “exercises in style”.
Primary PCI has to enlarge the treated population as much as possible, by educating people to provide first-aid care and recognise the early symptoms of a heart attack, and by reaching more patients with a reperfusion treatment even in places where primary angioplasty is not available. This is not simply a matter of style, this is doing more, for more people, and this is about saving millions of human beings.
The other projection into the future has to do with cardiac regenerative therapy, both at a vascular and at a muscular level. Repairing the irreparable, reversing the irreversible, and recovering the unrecoverable. Isn’t perhaps inventing the future the best manner to predict it…?
If so… what about using a BVS instead of a metallic stent that opens the artery as well, but then induces healing and disappears, allowing the regeneration of functioning vascular cells able to reconstitute a living artery, and leaving no traces of the PCI intervention...?
If so… what if cell therapy can transform necrotic tissue into functioning muscle...?
So far, these remain simply, objectively, just “open issues”, but the cardiovascular community is extremely active, creative and courageous, and we have seen a reduction of early mortality in STEMI patients from more than 25% in the pre-reperfusion era, to 12-15% in the eighties with aspirin and lytics, to 5-8% in the nineties with PCI, to less than 3% nowadays with new drugs and devices. However, there is still a future ahead, and the next frontiers are there to be challenged and pushed back. Give us a little more time and we will understand if the “vanishing” scaffold and the “resurrecting” cells are just another two new “exercises in style” or rather the prediction of an incredible future that is about to become real.
Conflict of interest statement
The authors have no conflicts of interest to declare.