Abstract
Aims: There is no consensus definition for minor and major stroke in trials comparing CAS vs. CEA. In this study the patients of our large single-centre CAS registry suffering a procedure-related stroke were categorised as minor or major stroke according to study-specific definitions.
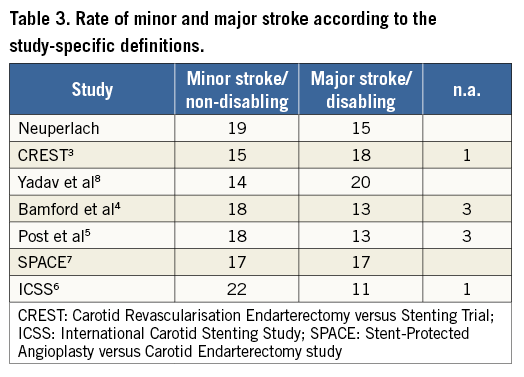
Methods and results: A board-certified neurologist examined nearly all patients (99%) pre- and post-procedurally, and once again in case of a subsequent neurological deficit. To objectify the deficits the NIHS Scale and modified Rankin Scale (mRS) were used. To compare the difference of the rates of minor and major strokes according to each definition, Fleiss’ Kappa and Cohen’s Kappa Test were used, as appropriate. Up to 30 days, 34 (3.6%) neurological events in 947 procedures lasting >24 hours (=stroke) occurred. According to our definition (major stroke: symptoms lasting >30 days, NIHSS ≥4 and/or mRS ≥3), 15 (1.6%) sustained a major and 19 (2%) a minor stroke. The comparison of all definitions of stroke resulted in a substantial agreement (Fleiss’ Kappa=0.73). The stroke rates depending on available definitions were as follows: our centre 19 minor/15 major strokes, CREST 15/18 (1 n.a.), Yadav et al 14/20, Bamford et al 18/13 (3 n.a.), Post et al 18/13 (3 n.a.), SPACE 17/17, ICSS 22/11 (1 n.a.).
Conclusions: Study-specific definitions for minor and major strokes lead to significantly different rates of stroke. Therefore, study-specific definitions should be respected comparing the results of each trial. A standard definition for minor and major stroke should be used in future trials.
Abbreviations
CAS: carotid artery stenting
CEA: carotid endarterectomy
CREST: Carotid Revascularization Endarterectomy versus Stenting Trial
ICSS: International Carotid Stenting Study
mRS: modified Rankin Scale
NIHSS: National Institutes of Health Stroke Scale
RCT: randomised controlled trial
SPACE: Stent-Protected Angioplasty versus Carotid Endarterectomy study
Introduction
The treatment of a significant carotid artery stenosis is performed to avoid neurological events, primarily strokes with restriction in daily routine. One of the most important issues during carotid revascularisation is to avoid procedure-related strokes.
In general, stroke is defined as a neurological deficit due to a cerebrovascular cause that persists beyond 24 hours. An updated definition of stroke was published in 2013, which includes objective evidence of ischaemic injury by imaging and clinical evidence based on symptoms persisting ≥24 hours or until death1.
The 24-hour limit divides stroke from transient ischaemic attack (TIA), which is a related syndrome of stroke symptoms but resolves completely within 24 hours after onset of first symptoms. In several large registries and randomised trials comparing carotid endarterectomy (CEA) and carotid artery stenting (CAS), stroke is categorised as minor and major stroke or disabling and non-disabling stroke. This categorisation is usually done by means of duration of the neurological symptoms or point value of different score systems. In most cases the National Institutes of Health Stroke Scale (NIHSS) and/or the modified Rankin Scale (mRS) is used. The allocation to the different subtype of stroke is important in view of the fact that patients with major symptoms (i.e., major or disabling stroke) are usually unable to manage their everyday life; moreover, a stroke with obvious disability leads to higher healthcare costs. Furthermore, it is known that a severe stroke has prognostic significance and the severity of the stroke is an important predictor of long-term survival2. However, to date, there is no unique classification for minor and major stroke3-8, which obscures direct comparisons of study results.
In this study we aimed to assess the impact of different stroke definitions, used in various trials, on the complication rate in our relatively large patient population treated and monitored in a standardised fashion.
Methods
For this retrospective analysis, we included all symptomatic and asymptomatic patients with a relevant carotid artery stenosis undergoing carotid artery stenting in a single centre. The stenosis quantification was carried out according to established criteria9,10. Since 1999, all procedures have been performed by one interventionalist or one further proctored by that interventionalist. In each patient a pre- and post-procedural neurological examination was done by a board-certified neurologist, usually the day before and the day after the intervention, and once again in case of a subsequent neurological deficit. The NIHSS11 and mRS12,13 were used to objectify potential neurological deficits occurring during or after the procedure. Further information about the registry is given in previous publications14,15. Table 1 shows the study-specific definitions for minor and major stroke. In our series a stroke was defined as minor if symptoms persisted less than 30 days, an NIHSS score of 1-3 and/or an mRS score <3. A major stroke included symptoms persisting ≥30 days, an NIHSS score of ≥4 and/or an mRS score ≥3.
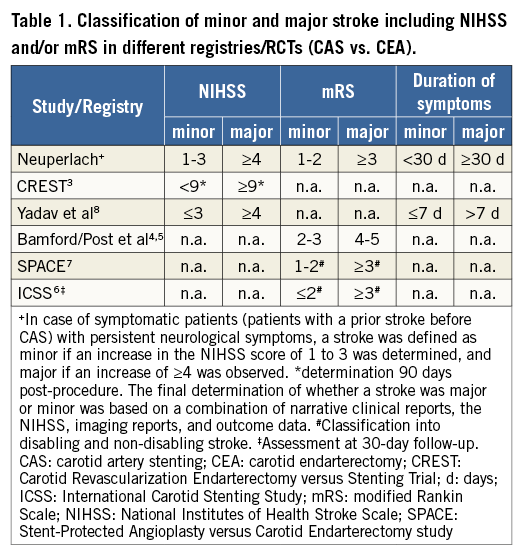
In case of symptomatic patients (patients with a prior stroke before CAS) with already existing neurological symptoms at baseline, a stroke was defined as minor if an increase in the NIHSS score of 1 to 3 was determined, and major if an increase of ≥4 was observed.
Statistical analysis
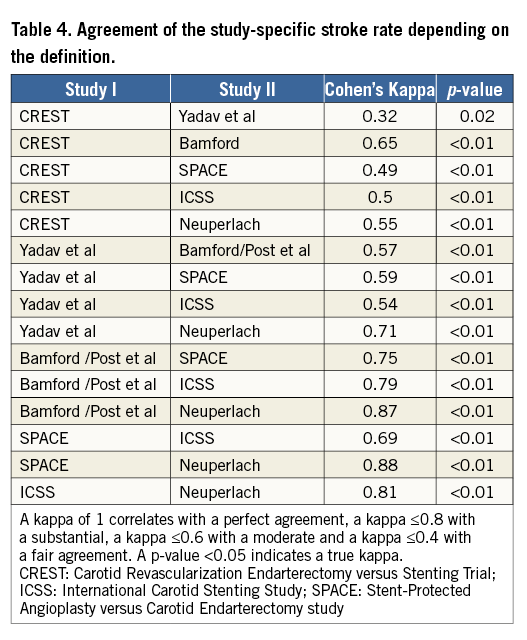
To compare the statistical difference of the rates of stroke according to each definition, Fleiss’ Kappa and Cohen’s Kappa Test were used. Kappa was used as a measurement of agreement (between two raters). In Cohen’s Kappa, it measures agreements between two raters, respectively; in Fleiss’ Kappa, it measures the overall agreements among all the raters, in this case the different definitions of the registries/studies. Conventionally, a Kappa of ≤0.2 is considered as slight agreement, 0.21-0.4 fair, 0.41-0.6 moderate, 0.61-0.8 substantial or strong, and more than 0.8 almost perfect agreement. The 95% confidence interval is Kappa±96 standard error.
Results
From 1999 to 2014, we performed 947 percutaneous carotid interventions in symptomatic and asymptomatic patients with a relevant carotid artery stenosis. The patient characteristics are listed in Table 2.
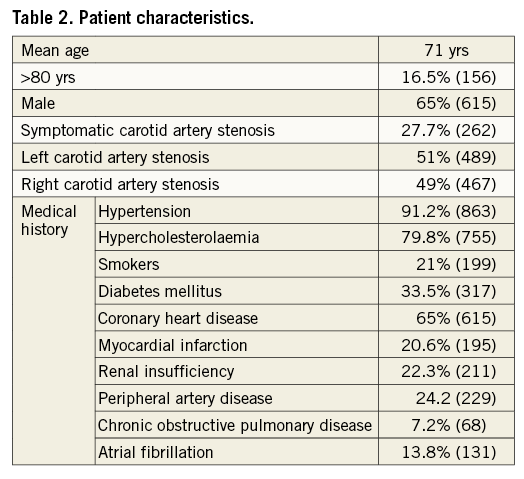
Up to 30 days after the procedure, 34 patients (3.6%) suffered a stroke (typical neurological symptoms lasting >24 hours, procedural neurological events included). In half of the patients (n=17) it occurred during the procedure, in the other half (n=17) post-procedurally during follow-up. According to our stroke definitions, 15 patients (1.6%) sustained a major and 19 patients (2%) a minor stroke. Table 3 shows the particular incidence of minor and major stroke according to the definition used in several large CAS registries or RCTs comparing CAS vs. CEA. Using these different definitions, our major stroke rate varies from 1.2%-2.1%, the minor stroke rate from 1.5%-2.3%. Some patients could not be allocated to either minor or major stroke due to missing clinical data, depending on the requirements of the study (in CREST, Bamford et al, Post et al, Yadav et al and ICSS). Table 4 illustrates the comparison of the different stroke rates of each study. All pairwise comparisons showed a statistically significant difference in the rates of minor and major stroke. Cohen’s Kappa resulted in fair to infrequently substantial agreement of the stroke rates. Fleiss’ Kappa yielded a value of 0.73 (95% CI: 0.6362 to 0.8210), testifying that the overall agreements among all raters (=study-specific definition of minor and major stroke) are not perfect, but substantial.
In patients with a symptomatic carotid artery stenosis (a neurological event ≤6 months before CAS) the change of NIHSS (before and after the recurrent event) was crucial for the stroke classification. In our registry, 14 of the 34 (41.2%) patients with a procedure-related stroke had a prior symptomatic carotid stenosis.
Discussion
On the basis of the 30-day stroke rate of our single-centre CAS registry, including almost 1,000 carotid procedures in symptomatic and asymptomatic patients, we found that the minor and major stroke rate varies significantly depending on the selected definition (Figure 1).
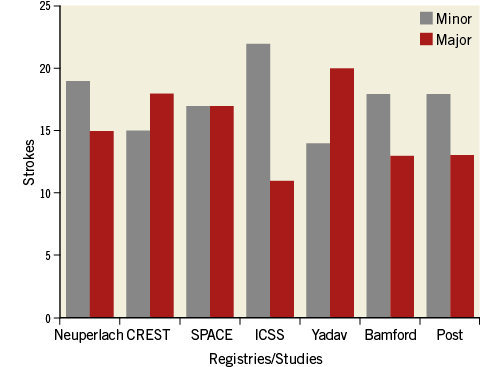
Figure 1. Procedure-related stroke rates after CAS in the same patient population according to the study-specific definition used in published trials.
In general, a minor stroke is defined as an ischaemic stroke irrespective of the origin (e.g., atrial fibrillation, carotid artery stenosis, arterio-arterial), usually associated with a short period of symptoms and good functional outcome. In contrast, patients suffering a major or disabling stroke are not able to carry out all usual activities and therefore require intensive rehabilitation and constant care later on.
In most of the CAS registries or RCTs comparing CAS vs. CEA, the NIHSS and/or mRS are used to classify the stroke symptoms in minor or major stroke. NIHSS includes a 15-item scale of neurological impairments (score from 0 to 42, from no symptoms up to coma/quadriplegia). The mRS ranges from 0, which means no symptoms, up to 6 (death) and specifies the degree of disability. However, there is no definite and uniform threshold to categorise stroke into minor or major. Moreover, using the NIHSS, the severity of symptoms may be underestimated particularly in terms of visual and language disorders16,17.
In a retrospective Italian analysis, Crespi et al evaluated a threshold to categorise patients as minor stroke according to the mRS in 2,389 stroke patients (any cause of stroke) of the SIRIO study database18. The threshold for minor stroke was determined as mRS ≤2 (slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance) due to a better outcome which resulted in a lower one-year mortality and a higher rate of discharge in comparison to all stroke patients, optimally evaluated at hospital discharge.
In addition, there is no general agreement on the timing of the assessment of stroke severity (immediately after the first contact with the symptomatic patient vs. at discharge or during follow-up). This is important because some patients improve during the hospital stay due to early therapy or intensive rehabilitation; however, a smaller proportion shows clinical impairment18. Hence, minor stroke may be different depending on the moment of the clinical examination of the patients.
In a further study, 760 consecutive patients with an acute ischaemic stroke were classified by means of six different minor stroke definitions, primarily based on the NIHSS16. The endpoint included the rate of discharge from hospital and neurological status assessed with mRS (favourable outcome at three months mRS of ≤2). The following definitions were considered most suitable for the term minor stroke due to most favourable outcome: all patients with an NIHSS score 0 or 1 on every baseline NIHSS score item, except level of consciousness items (definition A) and all patients with baseline NIHSS ≤3 (definition F). On the other hand, all patients with only motor deficits with or without sensory deficits and all patients with baseline NIHSS in the lowest (least severe) quartile of severity (NIHSS ≤9) had the worst outcome (definitions C and E). The advantage of definition F (NIHSS ≤3) is the objectiveness and simple assessment. Defining minor stroke by means of NIHSS ≤3 was used, in accordance with other important groups of stroke research8,19,20, and our single-centre registry. Notably, about 70% of the patients with an NIHSS 3 were discharged home compared to around 60% of those with an NIHSS 4. In patients with an NIHSS ≥5, the discharge rate was 35% or even less16. This result shows how challenging a determination of a threshold for minor stroke is.
In addition, the authors proposed to include not only the clinical symptoms of the patients, but also diffusion-weighted imaging to define those patients with a minor stroke more accurately16. However, data about the combination of clinical signs and imaging do not exist as yet.
In several randomised trials comparing CAS vs. CEA, the classification of stroke differs greatly (Table 1). In the Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis (CREST) trial a stroke was defined as major stroke on the basis of clinical data or if the NIHSS was 9 or higher 90 days after the procedure. Neurological assessment was carried out at baseline and 18 to 54 hours after the procedure and one month later3. However, in the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study, stroke was subclassified as disabling or non-disabling based on the mRS. Patients with an mRS ≥3 had a severe stroke, termed as disabling stroke7. Other neurological assessment was not mandatory to define the type of stroke. In a further international randomised trial comparing CEA vs. CAS in symptomatic patients (ICSS), a stroke was defined as a disabling stroke if there was an increase in the mRS to 3 or more at 30-day follow-up6.
In a CAS series with 107 consecutive patients, a minor stroke was defined as a neurological deficit lasting <7 days or an NIHSS of ≤3. A major stroke included symptoms lasting >7 days and an NIHSS >38.
With respect to the definitions mentioned above, we think that our definition for minor and major stroke best reflects the currently used classification: it is consistent with other trials and registries and uses the most frequently applied neurological assessment scales.
Limitations
Undoubtedly, the results of our registry include some limitations. A few of our patients suffering a procedure-related stroke could not be allocated appropriately according to the definitions of other trials because clinical reports were different. Furthermore, the exact moment of the neurological assessment after the procedure was not standardised. Neurological symptoms in particular are known to fluctuate. However, clinical assessment was performed in almost all of the patients pre- and post-procedurally by a board-certified neurologist before hospital discharge.
Conclusions
In summary, there is no consensus definition for minor and major stroke irrespective of the origin of the emboli. Using established definitions of large registries or RCTs led to significantly different minor and major stroke rates in our study cohort. Therefore, one should take notice of the definition of each study when comparing the results after carotid intervention. A standard definition for minor and major stroke should be used in each future trial to make results comparable.
| Impact on daily practice On the basis of the 30-day stroke rate of our single-centre CAS registry, we found that the minor and major stroke rates vary significantly depending on the definition used in several studies or registries. A standard definition for minor and major stroke should be used in each future trial to make study results comparable. Therefore, we think that our article contributes significantly to the field of CAS and CEA studies. |
Conflict of interest statement
The authors have no conflicts of interest to declare.