While it is generally accepted that patients with COVID-19 who have cardiac comorbidities suffer from a substantially increased risk of adverse outcomes, establishing a cohesive understanding of this relationship has proven elusive. Moreover, as healthcare systems continue to grapple with the relentless and often unforeseen challenges that accompany this global pandemic, progress in unravelling the virus’ pathobiology and seemingly pleiotropic effects has been additionally complicated by the disrupted delivery of even routine care. A blunted recognition of comorbid cardiovascular conditions coupled with uncertainty regarding how concomitant infection with a novel, highly contagious pathogen should influence treatment has likely contributed to these poor outcomes, especially in the setting of those who are critically ill. Unsurprisingly, this is particularly apparent to patients presenting with COVID-19 and ST-segment elevation myocardial infarction (STEMI).
While researchers were quick to identify a reduction in overall cardiac catheterisation laboratory (CCL) activations for STEMI during the early phases of the pandemic1, a worrisome association has been noted between COVID-19 and enhanced thrombogenicity that suggests, if anything, that STEMI incidence may have paradoxically increased during this time and may thus have been underreported. Moreover, in an attempt to preserve personal protective equipment, protect hospital staff from excess exposure, and achieve timely reperfusion, there has been renewed interest in fibrinolytic therapy as an initial management strategy for patients with COVID-19 and STEMI2. Despite a joint position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) strongly advocating the use of primary percutaneous coronary intervention (PPCI) when available3 (Figure 1), there have been few data describing how patients fare when managed with either approach. Existing case series of COVID-19 STEMIs have included limited numbers of patients and have demonstrated extraordinarily high in-hospital mortality rates of up to 50-70%4.
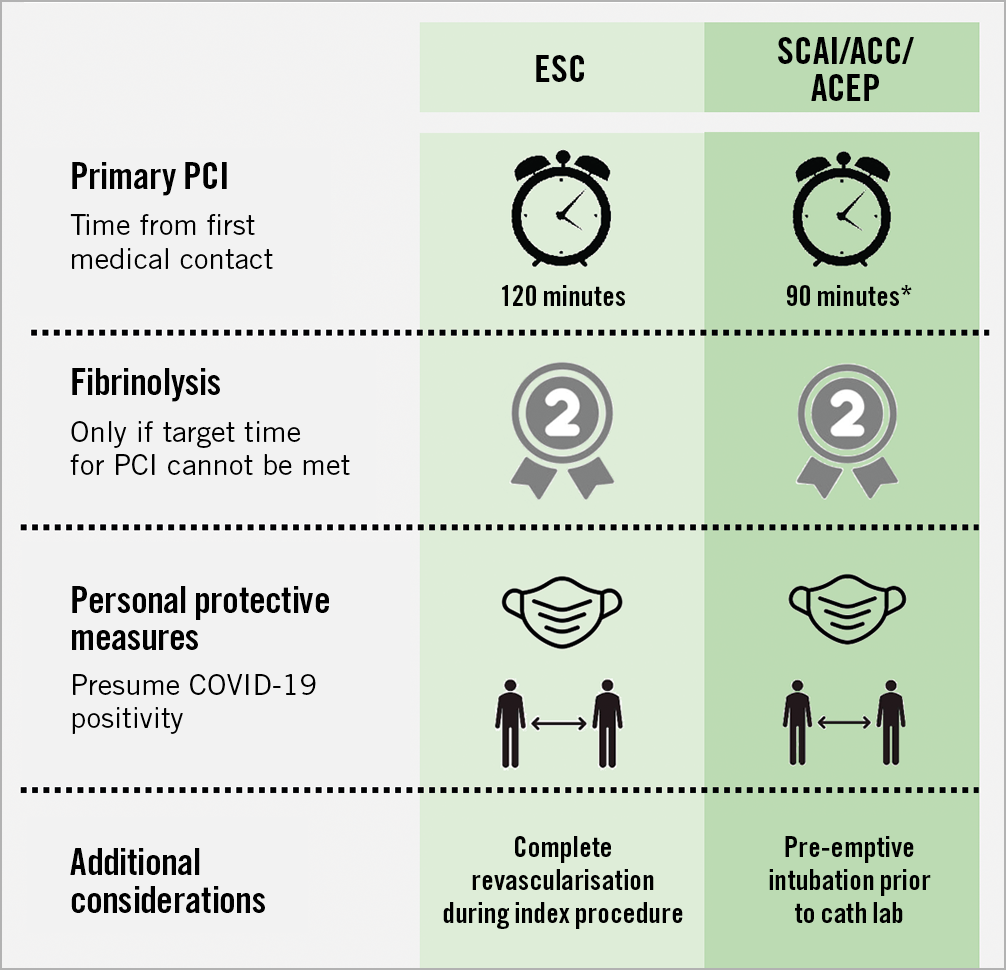
Figure 1. Consensus recommendations for managing ST-segment elevation myocardial infarctions during the COVID-19 pandemic from the European Society of Cardiology (ESC) and the Society for Cardiovascular Angiography and Interventions (SCAI), American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP). *120 minutes if transfer to a PCI-capable facility necessary
In this issue of EuroIntervention, Rodriguez-Leor et al report the outcomes of 91 patients with COVID-19 compared with 919 patients without COVID-19 treated with PPCI for STEMI from a Spanish multicentre registry5.
Interestingly, patients with COVID-19 and STEMI more frequently presented directly to the hospital rather than to auxiliary emergency medical services, in contrast to our experience in New York where delays in seeking care due to fear of contracting COVID-19 from the hospital were more common. COVID-19 patients were less likely to be pre-treated with aspirin or with a P2Y12 inhibitor and presented more frequently with heart failure. COVID-19 patients were more likely to undergo mechanical thrombectomy and receive GP IIb/IIIa inhibitors, suggesting perhaps a greater thrombotic burden. These patients had a 2.6-fold higher incidence of post-procedural cardiogenic shock, and a fourfold increase in acute stent thrombosis with a consequent fourfold higher rate of in-hospital mortality.
Although this article describes consistently worse outcomes for COVID-19 patients with STEMI, the in-hospital mortality rates are not as profound as previously described. Regrettably, understanding why patients in this study had relatively better survival when compared to prior observations4 is almost impossible given the substantial dissimilarities among patient populations, healthcare systems, and study design (including exclusion of patients who did not go to the CCL. However, some critical takeaways from this study include higher thrombotic burden, greater risk of acute stent thrombosis, cardiogenic shock and increased in-hospital death.
How can we therefore mitigate the risk in these patients? While not shown in this series, experience from other parts of the world indicates significant delays in seeking care. Therefore, increasing awareness about the warning signs of a myocardial infarction (MI) and the need for timely care is of paramount importance, even more so in the COVID era. Once patients present to the hospital, rapid triage including focused chest pain history, an electrocardiogram (ECG) and point-of-care ultrasound (POCUS) is critically important to identify rapidly those patients who may benefit from PPCI. Multiple randomised trials have shown that novel P2Y12 inhibitors such as ticagrelor and prasugrel have greater antiplatelet activity and have superior outcomes, including lower stent thrombosis, when compared with clopidogrel and should be preferred in the COVID era regardless of the COVID-19 status of the patients. In the CCL, similar to the observation in Spain, we observed increased thrombus burden in patients with COVID-196. Adjunct pharmacotherapy such as intracoronary IIb/IIIa and intracoronary thrombolytics may be useful in select patients6. In addition, the use of a fluoropolymer stent, which has been shown to have intrinsic thromboresistance properties7, can potentially provide added protection against stent thrombosis, although this has not been tested in clinical studies in COVID-19 patients. Additionally, in patients with severe COVID-19 and advanced comorbidities (including age) and cardiogenic shock, the futility of a PPCI approach should be considered. Further, given the early results of trials such as ACTIV-4a, REMAP-CAP, and ATTACC, preventative therapeutic anticoagulation should be considered to prevent thromboembolic events for hospitalised patients, although whether this strategy will prevent MIs is not known.
Overall, the work by Rodriguez-Leor et al lends credence to the theory that infected patients fare considerably worse when afflicted with cardiovascular illness even when treatment strategies are similar. There is therefore a growing recognition of the need for quick identification and risk assessment of patients with cardiovascular disease and COVID-19 so that we can continue working to avoid such a tragic disparity in outcomes.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.