Abstract
Aims: The aim of this study was to assess clinical and prognosis differences in patients with COVID-19 and STEMI.
Methods and results: Using a nationwide registry of consecutive patients managed within 42 specific STEMI care networks, we compared patient and procedure characteristics and in-hospital outcomes in two different cohorts, according to whether or not they had COVID-19. Among 1,010 consecutive STEMI patients, 91 were identified as having COVID-19 (9.0%). With the exception of smoking status (more frequent in non-COVID-19 patients) and previous coronary artery disease (more frequent in COVID-19 patients), clinical characteristics were similar between the groups, but COVID-19 patients had more heart failure on arrival (31.9% vs 18.4%, p=0.002). Mechanical thrombectomy (44% vs 33.5%, p=0.046) and GP IIb/IIIa inhibitor administration (20.9% vs 11.2%, p=0.007) were more frequent in COVID-19 patients, who had an increased in-hospital mortality (23.1% vs 5.7%, p<0.0001), that remained consistent after adjustment for age, sex, Killip class and ischaemic time (OR 4.85, 95% CI: 2.04-11.51; p<0.001). COVID-19 patients had an increase of stent thrombosis (3.3% vs 0.8%, p=0.020) and cardiogenic shock development after PCI (9.9% vs 3.8%, p=0.007).
Conclusions: Our study revealed a significant increase in in-hospital mortality, stent thrombosis and cardiogenic shock development after PCI in patients with STEMI and COVID-19 in comparison with contemporaneous non-COVID-19 STEMI patients.
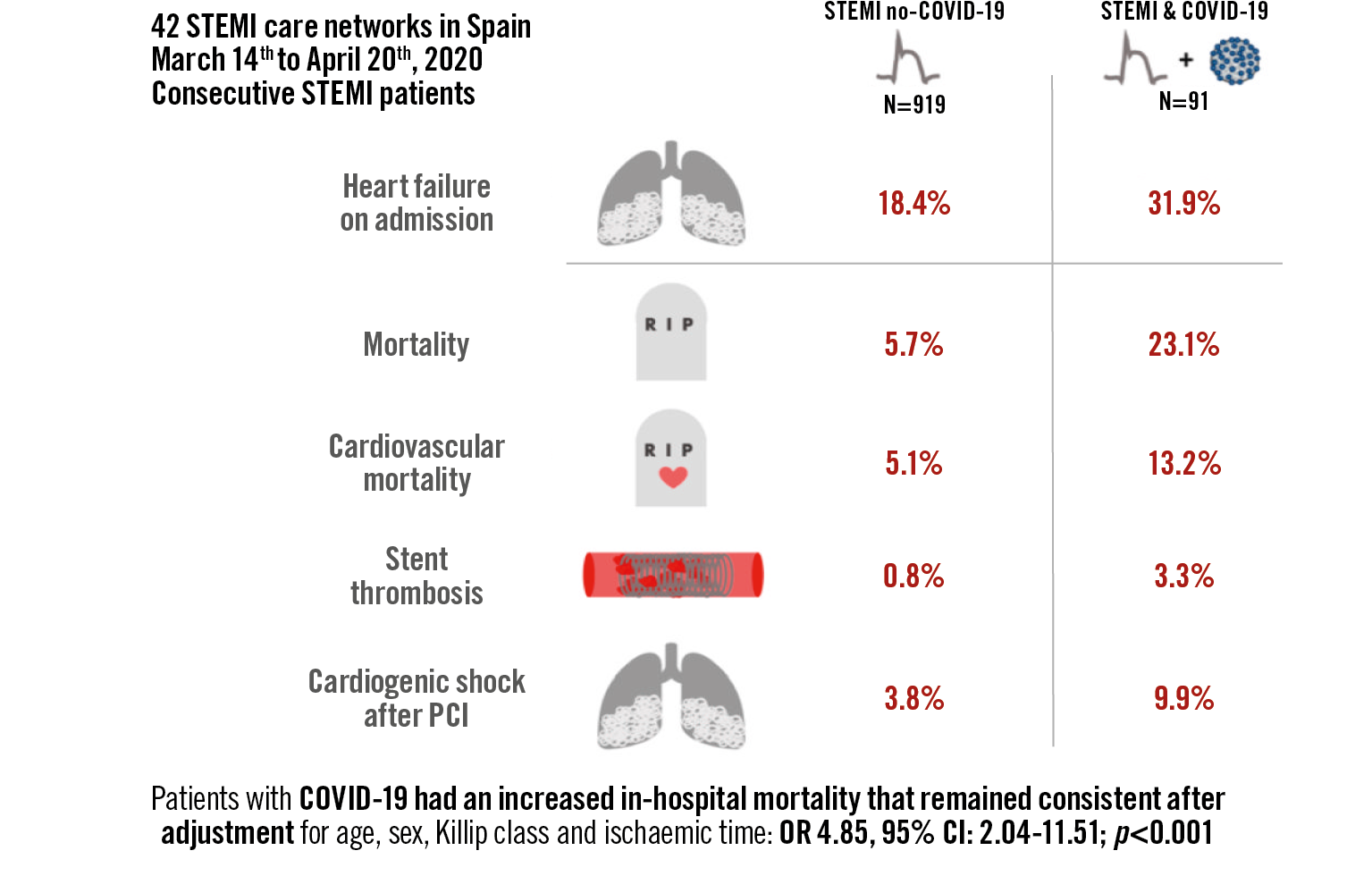
Visual summary. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients.
Introduction
The impact of COVID-19 on outcomes of ST-elevation myocardial infarction (STEMI) patients undergoing reperfusion has barely been explored. Two small series of 18 and 28 COVID-19 STEMI patients have been reported showing extremely high in-hospital mortality rates of 70% and 50%, respectively1,2. The lack of contemporaneous non-COVID-19 STEMI patients precludes a definite conclusion on the contribution of STEMI to the poor prognosis.
Here we present a nationwide cohort of consecutive STEMI patients admitted in 42 high-volume percutaneous coronary intervention (PCI) centres across Spain during the seven weeks that followed the country lockdown in March 2020. We aimed to study clinical and prognosis differences in patients with COVID-19.
Methods
SPANISH STEMI REGISTRY
In Spain there are 17 regional public service STEMI care networks which comprise 83 hospitals capable of performing primary percutaneous coronary interventions (PPCI) in 24/7/365 programmes. In 2018, 21,261 interventions in STEMI (91.6% PPCI, 3.2% rescue PCI and 5.1% routine early PCI strategy after fibrinolysis) were performed, representing 417 PPCI per million inhabitants3.
During the current COVID-19 outbreak, the Spanish Interventional Cardiology Association called for a registry to collect information on all consecutive STEMI patients retrospectively. Since March 2020, just after the activation of the “State of Alarm” and the country lockdown in Spain4, information on incidence, clinical characteristics, clinical management and outcomes has been recorded retrospectively.
The research protocol was approved by the Working Group on the Infarct Code of the Spanish Interventional Cardiology Association and by one central ethics committee.
STUDY DESIGN
The present report is a multicentre, retrospective, observational cohort study which evaluates procedures included in the Spanish Infarct Code Registry database. Supplementary Appendix 2 provides a checklist of items that should be included in reports of cohort studies. Between 14 March and 30 April 2020, a total of 42 hospitals with at least one patient with confirmed STEMI and a positive SARS-CoV-2 polymerase chain reaction (PCR) assay were identified and included in the analysis.
In these centres, all consecutive STEMI patients admitted were divided into COVID-19 and non-COVID-19 STEMI groups to compare clinical characteristics, in-hospital management and in-hospital clinical outcomes. Patients with a final diagnosis different from STEMI were not included in the final analysis. COVID-19 was defined when a PCR assay for SARS-CoV-2 was positive. Delay times were defined according to the European guidelines5. Data were collected reviewing clinical records. Cardiogenic shock diagnosis was based on clinical examination on admission and was defined as systolic blood pressure less than 90 mmHg or the need for vasopressors to maintain blood pressure above 90 mmHg combined with signs of peripheral hypoperfusion (coldness and/or pallor in the extremities, oliguria, or a decrease in level of consciousness)6.
We did not include patient and public involvement in this study.
INCIDENCE OF COVID-19 IN SPAIN
At the time the “State of Alarm” was declared in Spain, on 14 March 2020, 5,753 cases of COVID-19 had been diagnosed and there were 136 deaths. On 3 May 2020, when this analysis ended, there were 217,466 cases diagnosed (positive PCR assay), with 25,264 deaths and 118,902 recovered patients. At that moment, Spain was the leading European country in terms of the number of cases and mortality adjusted for population, ahead of the United Kingdom and Italy7.
STATISTICAL ANALYSIS
Frequencies (percentages) and means (±SD) were used to describe the population. Comparisons were performed using a t-test or non-parametric tests for continuous variables and a chi-square test or Fisher’s exact test for categorical variables. The association between COVID-19 and in-hospital mortality was assessed using both unadjusted and adjusted logistic regression models, estimating odds ratios (OR) and their 95% confidence interval (95% CI). In the latter, estimations were adjusted for age, gender, Killip class and time from symptom onset to reperfusion. All tests were two-sided. A p-value of 0.05 was considered to set statistical significance. All analyses were performed using Stata 15.0 (StataCorp, College Station, TX, USA).
Results
PATIENTS
A total of 1,130 patients with suspected STEMI were cared for at 42 high PCI-volume hospitals that were hubs of regional networks for STEMI treatment, with 109 patients having a positive PCR assay (9.6%). The final study sample is made up of 1,010 patients with confirmed STEMI, with 91 patients who had a positive PCR assay (9.0%). Figure 1 shows the flow chart of patients. Baseline clinical characteristics are provided in Table 1.
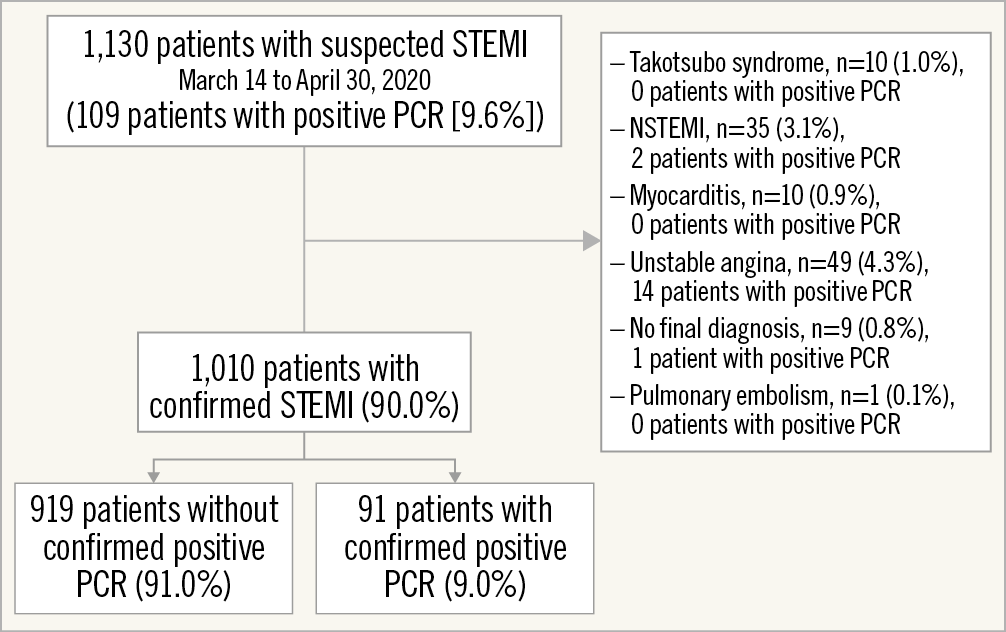
Figure 1. Flow chart of patients. STEMI. NSTEMI: non-ST-elevation myocardial infarction; PCR: polymerase chain reaction; STEMI: ST-elevation myocardial infarction
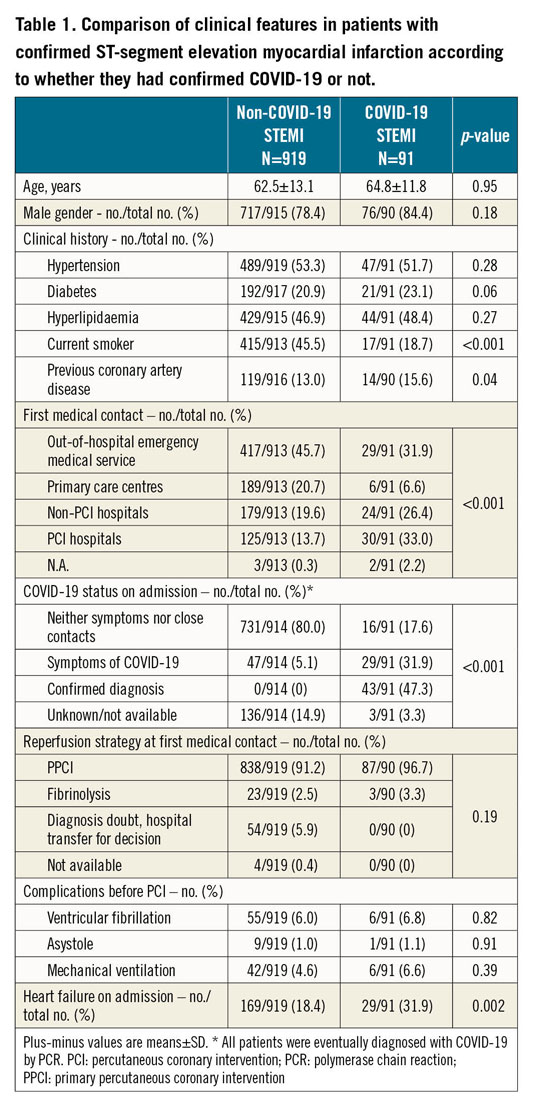
With the exception of smoking status (higher in non-COVID-19 patients) and previous coronary artery disease (higher in COVID-19 patients), the clinical characteristics were not different between the groups. The mode of presentation differed significantly between the groups, COVID-19 patients presenting more frequently at the hospital and less frequently via extra-hospital emergency medical services. Patients with COVID-19 more frequently had heart failure on arrival at the catheterisation laboratory. On admission, only 43 patients (4.3%) had a confirmed COVID-19 diagnosis; during admission, COVID-19 was diagnosed in 48 additional patients (4.8%), with a final sample of 91 patients (9.0%). Up to 96% of patients with clinical suspicion of COVID-19 during admission had a PCR assay. Figure 2 shows the COVID-19 status diagnosis path.
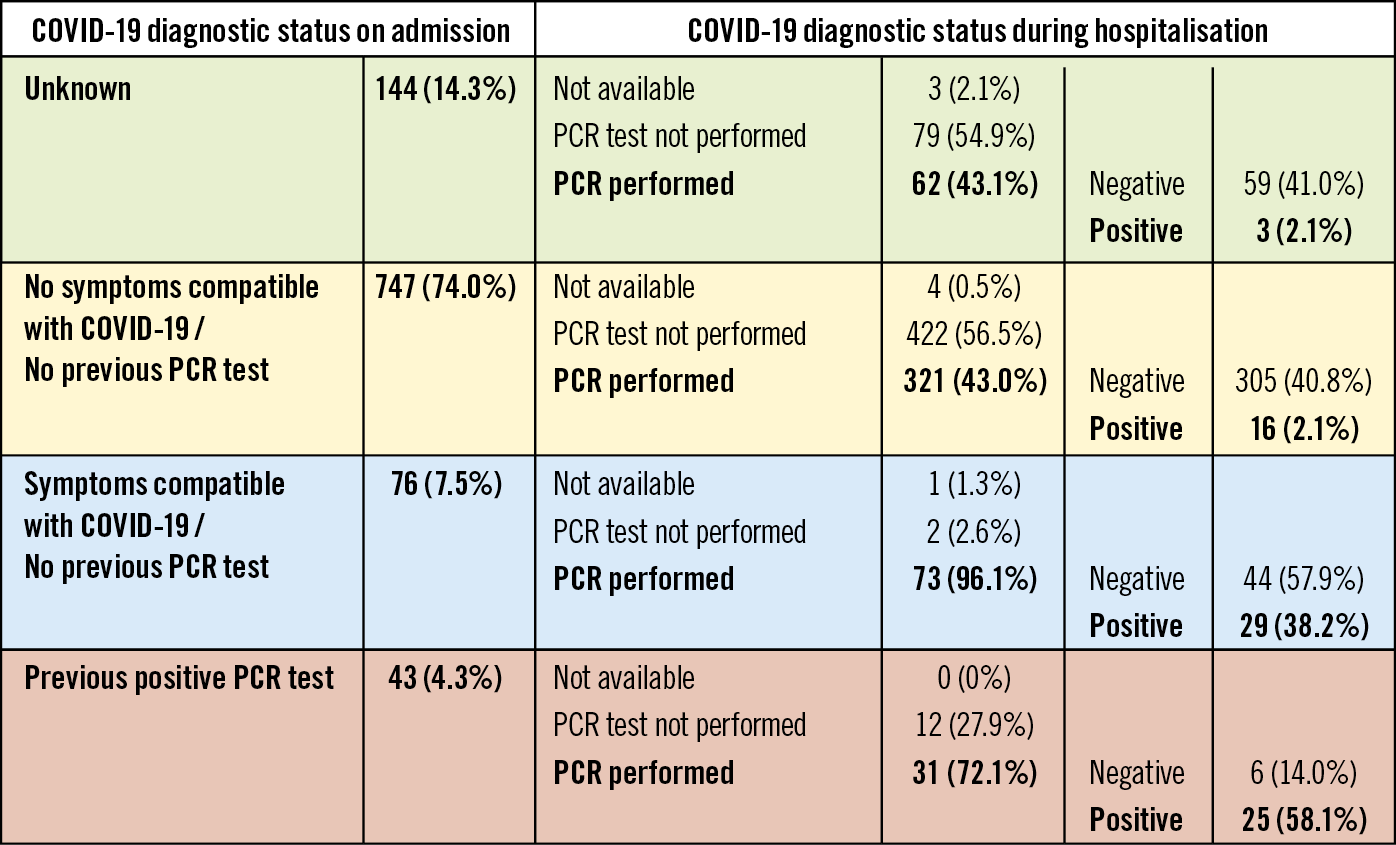
Figure 2. COVID-19 diagnostic status path. Patients were categorised on admission according to their COVID-19 status into four groups: unknown, no symptoms compatible with COVID-19 or previous PCR test, symptoms compatible with COVID-19 but no previous PCR test or previous positive PCR test. Although it is essential to perform a PCR assay at admission in all patients, it should be noted that at the beginning of the pandemic, when this study was carried out, PCR was not available in many facilities. PCR: polymerase chain reaction
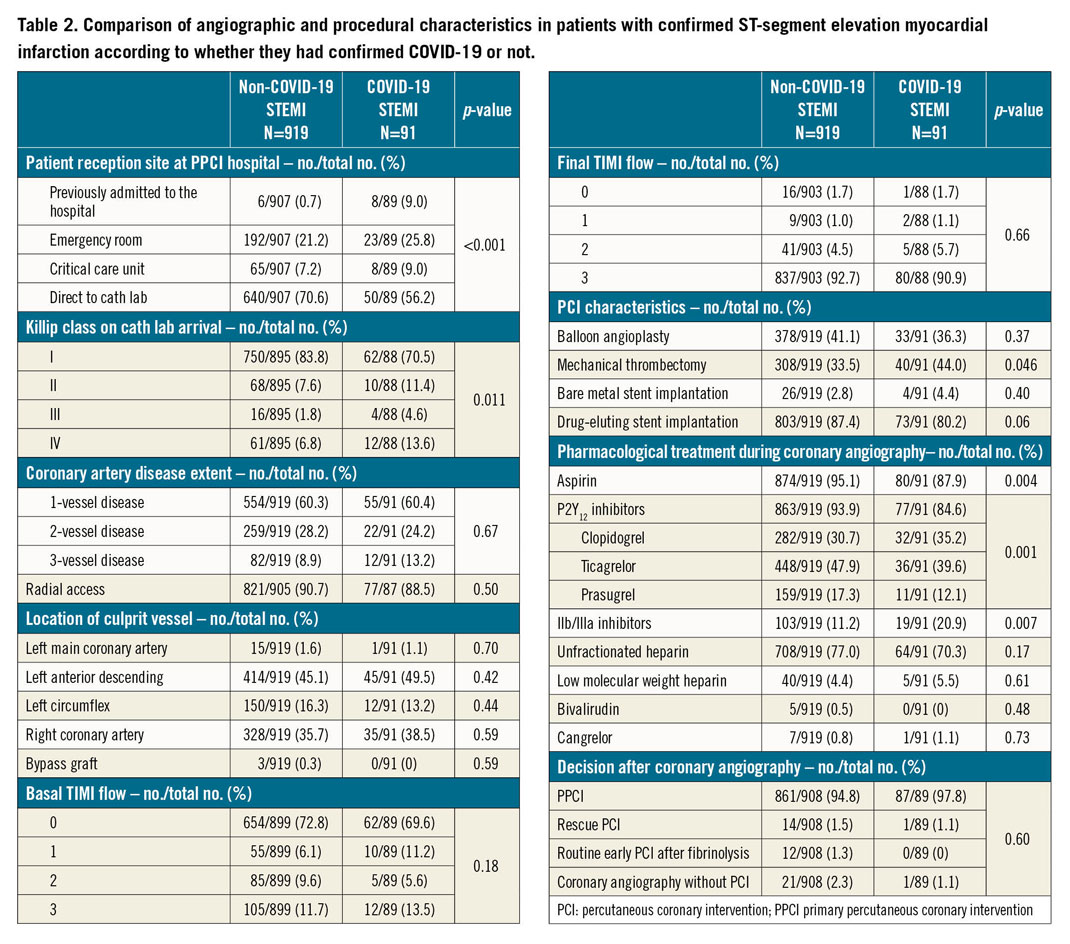
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Table 2 shows angiographic and procedural characteristics. Absence of significant stenosis on coronary angiography was present in 2.6% in patients with STEMI as the final diagnosis and 59.2% in patients with other diagnoses. In the whole cohort, 8.6% of patients did not have significant coronary stenosis (8.2% in patients without COVID-19 and 11.9% in COVID-19 patients). Patients with confirmed COVID-19 less frequently received pre-treatment with acetylsalicylic acid (ASA) and P2Y12 inhibitors (87.9% vs 95.1%, p=0.004, for ASA, and 84.6% vs 93.8%, p=0.001, for P2Y12 inhibitors). Conversely, mechanical thrombectomy (44% vs 33.5%, p=0.046) and glycoprotein (GP) IIb/IIIa inhibitors during the procedure (20.9% vs 11.2%, p=0.007) were more frequently used in COVID-19 patients.
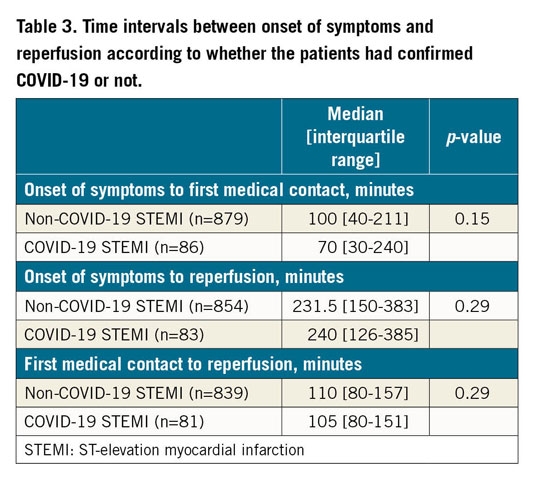
DELAYS TO REPERFUSION
Table 3 shows the main delays to reperfusion intervals. Time between symptom onset and first medical contact trended to be shorter in COVID-19 patients (70 [30-240] vs 100 [40-211] minutes, p=0.15); there were no differences in time between symptom onset and reperfusion (231.5 [150-383] vs 240 [126-385] minutes, p=0.29). The time between first medical contact and reperfusion was similar in both groups (110 [80-157] vs 105 [80-151] minutes, p=0.29).
IN-HOSPITAL OUTCOMES
Figure 3 summarises in-hospital outcomes. Patients with COVID-19 had an increased in-hospital mortality (23.1% vs 5.7%, p<0.0001), driven by both non-cardiovascular (9.9% vs 0.5%, p<0.001) and cardiovascular causes (13.2% vs 5.1%, p=0.002). This association remained consistent after adjustment for age, sex, Killip class and time from symptom onset to reperfusion (OR 4.85, 95% CI: 2.04-11.51; p<0.001).
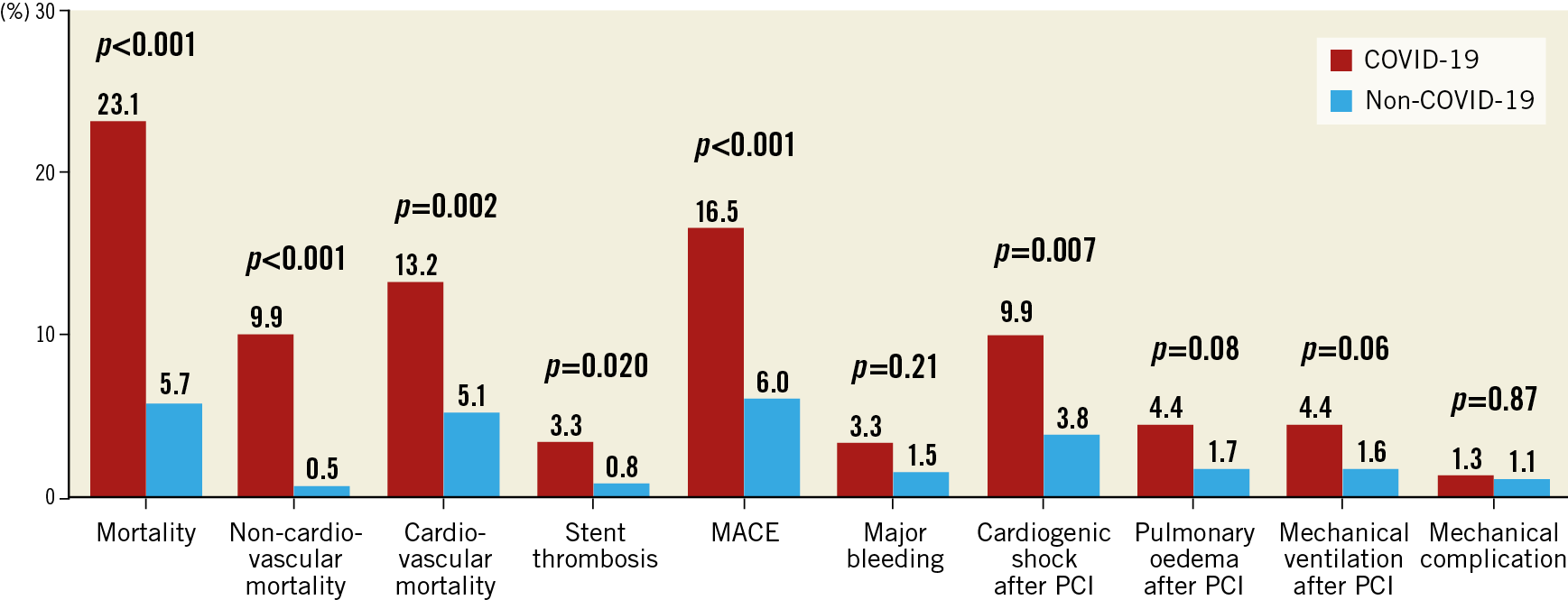
Figure 3. In-hospital outcomes. MACE: major adverse cardiovascular events (defined as cardiovascular mortality, non-fatal myocardial infarction or stent thrombosis)
Interestingly, an increase of in-hospital stent thrombosis was observed (4.1% vs 0.8%, p=0.015) as well as an increase in cardiogenic shock after PCI (9.9% vs 3.8%, p=0.007). Stent thrombosis in patients with COVID-19 was acute and over drug-eluting stents in all cases; all patients were on aspirin and clopidogrel. Major cardiovascular events, defined as cardiovascular mortality, non-fatal acute myocardial infarction or acute stent thrombosis, were also more frequent in patients with COVID-19 (16.5% vs 6.0%, p<0.001).
Discussion
To our knowledge, this is the first study to have evaluated the influence of COVID-19 on early outcomes in patients with STEMI cared for in specific care networks in comparison with contemporaneous non-COVID-19 STEMI patients, as well as the largest series of COVID-19 STEMI patients thus far. It has the advantages of being multicentre and multi-region, providing a more balanced approach than the previously published manuscripts. Compared to non-COVID-19 patients, there was a higher percentage of heart failure on arrival and increased in-hospital mortality in COVID-19 patients with a hazard risk of 4.85 after controlling for age, sex, class and time from symptom onset to reperfusion. In addition, patients had evidence of more thrombotic lesions with higher use of mechanical thrombectomy and GP IIb/IIIa inhibitors and an increase in in-hospital stent thrombosis and cardiogenic shock development after PCI.
PREVALENCE OF COVID-19 IN STEMI
On 3 May 2020, confirmed COVID-19 cases in Spain were 217,416, implying a prevalence of confirmed cases (positive PCR assay) of 0.5%7. The reported prevalence of COVID-19 in STEMI patients at the beginning of the pandemic all over the country was 6.3%8, but these data included many hospitals without any case diagnosed. In our series we found a prevalence of 9.0%; 43 patients (4.3%) were already COVID-19 confirmed cases at the time of STEMI. PCR was performed during admission in 456 out of the remaining 967 patients. Thus, 511 STEMI patients never had PCR and therefore it is plausible that the prevalence of COVID-19 in our cohort is underestimated. In fact, it is estimated that more than half of SARS-CoV-2 infected patients are asymptomatic9. Nevertheless, up to 96% of patients with clinical suspicion of COVID-19 during admission had a PCR assay. Of the 823 patients with clinical information on the presence or absence of symptoms related to COVID-19 on admission and without previous diagnosis, only 45 (5.5%) had a positive PCR assay (2.1% asymptomatic and 38.2% with any symptom suggestive of the disease). Although in the current situation it is essential to perform a PCR assay on admission in every patient, it should be noted that, at the beginning of the pandemic, when this study was carried out, PCR was not readily available in many facilities.
ANGIOGRAPHIC CHARACTERISTICS
A recent case series of STEMI patients with PCR-confirmed COVID-19 from several hospitals in Lombardy, Italy, reported up to 39.3% of patients without obstructive coronary artery disease. In fact, PCI was performed in only 60.7% of STEMI cases2. It is not clear if those were consecutive patients or selected cases. Our data show a very different scenario, with an incidence of non-obstructive coronary artery disease in COVID-19 STEMI patients of only 2.2%, not different to COVID-19 negative patients. In our case, all patients were cared for in STEMI code networks. The criteria for STEMI code activation were chest pain and an ECG with ST-segment elevation. There were 120 patients with a final diagnosis different from STEMI (10.7%), which is very similar to what we found when compared with STEMI activity during 2019 in Spain; among patients with a final diagnosis different from STEMI, non-obstructive coronary artery disease was also similar to what was found during 2019, when there was no COVID-198. Between 1-14% of STEMI occur in the absence of obstructive coronary artery disease. We analysed only patients with a confirmed STEMI diagnosis and so we excluded other causes of myocardial infarction with non-obstructed coronary arteries such as myocarditis, Takotsubo syndrome, non-ST-elevation myocardial infarction or pulmonary embolism which, in our series, represented 10.6% of patients.
Choudry et al recently reported a single-centre experience in patients with confirmed STEMI and COVID-1910. Their findings are in line with our findings and suggest a strong signal towards a higher thrombus burden and poorer outcomes in patients with COVID-19 and STEMI. Interestingly, they performed an angiographical analysis and found that COVID-19 patients presented higher multivessel thrombosis, higher thrombus grade and poorer myocardial blush grade after PCI. Levels of D-dimer were found to correlate with thrombus grade, myocardial blush grade, and levels of heparin requirement during the primary PCI procedure, with a suggestion of higher heparin doses required to achieve therapeutic activated clotting times (ACT) in this cohort.
REPERFUSION STRATEGY
Different scientific societies have developed recommendations on reperfusion strategy during the COVID-19 outbreak, with advice that differs, depending on the conditions in each country. In China, the Pekin Union Medical College Hospital recommended thrombolysis as the first choice of treatment, and only recommended coronary intervention after ruling out COVID-19, even in case of contraindications to fibrinolysis11. The American College of Cardiology Interventional Council and the Society for Cardiovascular Angiography and Interventions stated that fibrinolysis could be considered an option for relatively stable STEMI patients with active COVID-19 to prevent staff exposure12. The recommendation of the Spanish Society of Cardiology was to maintain PPCI as the reperfusion strategy of choice in all patients during the COVID-19 crisis13. In agreement with this recommendation, >90% of patients in both groups underwent mechanical reperfusion. Delays to reperfusion were similar in both groups, but the time between symptom onset and first medical contact tended to be shorter in patients with COVID-19. This is probably due to the fact that 9% of COVID-19 patients who presented a STEMI were already admitted to a hospital, compared to 0.7% of the non-COVID-19 patients. Furthermore, up to 5.9% of non-COVID-19 patients were transferred to another centre to decide whether or not they had a STEMI, while this did not occur in any patient with COVID-19.
Pre-treatment with platelet inhibitors was also less frequent in patients with COVID-19, probably due to a worse clinical scenario (higher incidence of heart failure on admission) but use of thrombectomy devices and administration of GP IIb/IIIa inhibitors during PCI was more frequent. Of note, the incidence of acute and subacute stent thrombosis was significantly higher in the COVID-19 group (4.1% vs 0.8%, p=0.015). Although the lower rate of pre-treatment with antiplatelet therapies in these patients could have played a role, the heightened inflammatory and prothrombotic state reported in COVID-19 patients14 could also explain this alarmingly high rate of stent thrombosis. Anyway, we believe that, among STEMI patients, antithrombotic treatment should be more aggressive in those with concomitant COVID-19 infection.
IN-HOSPITAL OUTCOMES
We found a high in-hospital mortality (23.1%) in patients with COVID-19 and STEMI. They presented a higher incidence of heart failure on admission. Mortality remained higher for patients with COVID-19 after adjusting for confounding factors. Undoubtedly, COVID-19 infection is a serious disease with a high mortality rate, that could explain the higher non-cardiovascular mortality in COVID-19 positive STEMI patients. However, additionally, these patients had a higher incidence of cardiac events (cardiovascular death, reinfarction, or stent thrombosis). In fact, recent reports also suggest a higher thrombus burden and stent thrombosis risk in patients with COVID-19 and STEMI10. Although this is speculative, COVID-19 disease could reduce haemodynamic tolerance to complications related to the infarction, and additionally some drugs that have been used against COVID-19 infection could have a deleterious effect on cardiovascular function and could have interacted with antithrombotic and cardiovascular drugs prescribed in STEMI patients.
A recent trial evaluating antiviral medication in patients with confirmed SARS-CoV-2 infection and severe respiratory involvement showed a 19.2% to 25% 30-day mortality15. Data from the north of Italy suggested an even higher in-hospital mortality in STEMI patients with COVID-19 - up to 35.3% in patients treated with PCI and 45.4% in patients who did not have a culprit lesion on coronary angiography. In this series of cases, the high incidence of advanced heart failure or cardiogenic shock (75%) suggests a highly selected population that could explain this elevated mortality2. Another case series from the New York area also reported a very high mortality in patients with COVID-19 who presented ST-segment elevation on electrocardiography, with 50% in-hospital mortality in eight patients with STEMI and 90% in-hospital mortality in patients with non-coronary myocardial injury. In this series, 83% of STEMI patients were treated with PPCI, 12% suffered previous cardiac arrest and 25% presented cardiogenic shock1. We think that, although with a limited number of patients, our non-selected data probably best reflect the reality of patients with COVID-19 and STEMI, in line with the recent results of a series of 39 patients that found a 17.9% in-hospital mortality10.
Limitations
The limitations of this study are those of any multicentre registry. It is impossible to presume that every operator interpreted variables in the same way. Also, there is no way to determine inter-observer and inter-centre differences in denoting any particular variable. However, these definitions are a standard used in interventional practice and were originally designed to be intuitively applied by the clinician. PCR assays were not systematically performed in all patients, but it should be noted that, at the beginning of the pandemic, when this study was carried out, PCR was not available in many facilities, and it was performed in the vast majority of patients who had clinical symptoms of COVID-19 upon admission (96.1%). The data collected are not specific for patients with COVID-19 but for patients with STEMI and, unfortunately, we do not have available data on analytical parameters or on other clinical variables that could affect the evolution of patients with COVID-19. In any case, what is clear is that these patients have a higher risk of adverse cardiovascular events during hospital admission for STEMI.
Conclusions
Our study revealed a significant increase in in-hospital mortality in patients with STEMI and COVID-19, in comparison with contemporaneous non-COVID-19 STEMI patients. We did not find differences in the extent of coronary artery disease, and PPCI was the reperfusion strategy in the vast majority of patients. COVID-19 patients presented a higher rate of stent thrombosis and cardiogenic shock development after PCI.
|
Impact on daily practice Despite a similar risk profile and similar total ischaemic time, COVID-19 patients presented more frequently with heart failure and had significantly higher in-hospital mortality (driven both by cardiovascular and by non-cardiovascular causes) than non-COVID-19 patients. The incidence of acute stent thrombosis and cardiogenic shock development after PCI was significantly higher in COVID-19 patients. Antithrombotic treatment should probably be more aggressive in those with concomitant COVID-19 infection to prevent stent thrombosis. |
Conflict of interest statement
A. Perez de Prado has received personal fees from iVascular, Boston Scientific, Terumo, B. Braun, and Abbott, outside the submitted work. A. Cequier has received grants and personal fees from Abbott Vascular, Medtronic and Biosensors; grants from Boston Scientific, Biomenco, Cordis, OrbusNeich and Spanish Society of Cardiology; personal fees from Ferrer International, Terumo and AstraZeneca, all outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.