Abstract
Aims: Assessment of health related quality-of-life (HRQL) has become increasingly important as not only the clinician’s view of the technical success, but also the patient’s perception is being measured. We evaluated the HRQL following sirolimus-eluting coronary stent (SES) (CYPHER®; Cordis, Johnson & Johnson, Warren, NJ, USA) implantation in patients with multivessel disease, comparing the outcomes with the historical surgical and bare metal stent (BMS) arms of the ARTS-I study.
Methods and results: The HRQL outcomes were compared to the outcome of the historical cohorts of the randomised ARTS-I trial using the same inclusion and exclusion criteria. HRQL was evaluated at baseline, at one month and at 6, 12 and 36 months after revascularisation using the SF-36 in patients treated with SES (n=585), BMS (n=483) or coronary artery bypass graft (CABG) (n=492). The HRQL compliance rates varied from 100% at baseline to 92% at 36 months. Both stenting and CABG resulted in significant improvement of HRQL and anginal status. There was a trend towards better HRQL after CABG than BMS beyond six months. Already from the first month up to three years, SES patients had, on average, 10% significantly better HRQL than BMS patients on the HRQL subscales physical functioning, role physical functioning, role emotional functioning and mental health (p<0.01) and a trend towards better HRQL in the other subscales. Up to 12 months, the HRQL was better after SES than CABG and was identical thereafter. At all time points, angina was more prevalent in the BMS group than in both the SES and CABG groups, in which the incidence of angina was similar. At three years, 10% of the SES patients suffered from angina, 13% of the CABG patients and 20% of the BMS patients.
Conclusions: Both stenting and CABG resulted in a significant improvement in HRQL and angina. Along with a substantial reduction of restenosis, HRQL after SES was significantly improved as compared with BMS, and was similar to CABG.
Abbreviations
ARTS: Arterial Revascularisation Therapy study
BMS: Bare metal stent
CABG: Coronary artery bypass graft
DES: Drug-eluting stent
HRQL: Health related quality-of-life
PCI: Percutaneous coronary intervention
PTCA: Percutaneous transluminal coronary angioplasty
SES: Sirolimus-eluting stent
SF-36: Short form health survey
Introduction
Randomised studies comparing percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) among patients with multivessel coronary artery disease showed similar rates of death, myocardial infarction and stroke between both treatment modalities1. Additionally, another important outcome measure is the patient’s subjective appraisal of the intervention and since elimination of ischaemia is more complete with surgery, patients may derive a greater health related quality-of-life (HRQL) benefit with CABG as compared with PCI2-9. Recently, we reported the HRQL, assessed by the Short form health survey (SF-36), of the Arterial Revascularisation Therapy Study-I (ARTS-I)10. This randomised controlled trial compared CABG with PCI using bare metal stents (BMS) in patients with multivessel disease. There was a trend towards a better HRQL after CABG, but this difference was mainly attributed to a higher repeat revascularisation rate in the PCI arm. With the introduction of the first drug-eluting stent (sirolimus-eluting stent [SES]) repeat revascularisation rates after stenting decreased significantly11 and there was a need for a randomised comparison between bypass surgery and stenting with SES for multivessel disease, using a similar study design as in ARTS-I12,13. The ARTS-II registry was designed applying the same inclusion and exclusion criteria, the same protocol definitions and the same primary endpoint, in order to make the registry as comparable as possible to the randomised ARTS-I14,15. The present study evaluated the SF-36 and anginal status at baseline, at one month and at 6, 12 and 36 months of the SES in patients with multivessel disease compared to the outcomes of the historical results of the two arms of ARTS-I.
Methods
Study design
ARTS-II is a multicentre, non-randomised, open label, trial designed to compare the safety and efficacy of the SES (CYPHER®; Cordis, Johnson & Johnson, Warren, NJ, USA) in patients with de novo multivessel coronary artery disease with the surgical group of ARTS-I acting as a historical control14. In order to obtain a population comparable to ARTS-I, patients were stratified by clinical site in order to ensure the inclusion of at least 1/3 of patients with three-vessel disease. ARTS-II included between February 2003 and November 2003, 607 patients at 45 participating centres.
A total of 1,205 patients who had multivessel disease and were considered equally treatable with the two modalities were randomised to either stent implantation (n=600) or CABG (n=605) at 67 participating centres worldwide between April 1997 and June 1998 in ARTS-I. Details of this study have been described previously12. The indications for revascularisation included silent ischaemia, stable or unstable angina pectoris, and the presence of at least two de novo lesions located in different major epicardial coronary arteries, potentially amenable to stent implantation.
As the translation of the SF-36 questionnaire was not available in Portuguese, Greek and Danish (Portugal, Brazil, Greece and Denmark), 170 of the 1,812 patients were not included in this substudy. Of the eligible patients, 1,535 (93%) agreed to participate in this study. At respectively 1, 6, 12 and 36 months follow-up 6, 20, 24 and 43 patients had died respectively (equally divided among both treatment groups). The corresponding participating rates were 100% at baseline and 92% at all other time points.
Health related quality-of-life and anginal status
The Short form health survey (SF-36) is a generic measure of HRQL that assesses eight domains, i.e., physical functioning, role physical functioning, role emotional functioning, mental health, vitality, social functioning, bodily pain, and general health16. The SF-36 is a standardised and validated instrument validated by the American Association of Cardiovascular and Pulmonary Rehabilitation and is used for evaluating health related quality-of-life in patients with cardiovascular disorders. It enables the assessment of any limitation of patient’s physical, psychological and social functioning16. Scale scores are obtained by summing the items together within a domain, dividing this outcome by the range of scores and then transforming the raw scores to a scale from zero to 100. A higher score on the SF-36 sub domains represents a better HRQL with a high score on the bodily pain scale indicating freedom from pain. The scale has good reliability with Cronbach’s alpha ranging from .65 to .96 for all subscales17. The SF-36 was administered at baseline, and at 1, 6, 12 and 36 months’ post-index procedure.
Anginal status was assessed by the Canadian Cardiovascular Society (CCS) classification18.
Statistical analysis
Discrete variables are given as percentages and SES and CABG, and SES and BMS were compared using the chi-square test. Continuous variables were compared using student’s t-test and were presented as means ±SD. Unadjusted SF-36 scores at each of the time points were compared by independent t-tests. To compare SF-36 changes over time between the treatment groups were performed using ANCOVA with adjustments for baseline SF-36 scores and all baseline characteristics from Table 1.
To control for the differences in baseline characteristics between SES and CABG, and SES and BMS, HRQL was compared using generalised mixed models for continuous repeated longitudinal data. To adjust for baseline HRQL differences, HRQL baseline was included as a covariate in the multivariable regression models. All analyses were performed according to the ”intention-to-treat” principle. All statistical tests were two-tailed. P < 0.05 was used for all tests to indicate statistical significance. All data were analysed with SPSS software (SPSS 15.0, SPSS Inc., Chicago, IL, USA).
Results
Patients treated in ARTS-II were significantly older than those in ARTS-I (Table 1). ARTS-II had a significantly higher incidence of diabetes mellitus, hypertension, hypercholesterolaemia and silent ischaemia, and a lower percentage of current smokers or patients with a history of prior myocardial infarction as compared to the ARTS-I CABG groups. Seven BMS patients did not receive any stents during the index procedure (four underwent elective CABG, one required emergent CABG, one underwent percutaneous treatment 35 days later and one remained on medical therapy). The percentage of percutaneous 3-vessel treatment was 54% in ARTS-II versus 31% in ARTS I. The 3-year survival rate in ARTS-II was similar with the historical surgical and angioplasty cohorts of ARTS-I (SES: 3%; BMS: 4%; CABG: 4%). Cumulative freedom from major adverse cardiac and cerebrovascular events after SES was 81% which did not differ significantly with CABG (84%; p=0.2), but higher than after BMS (66%; p<0.0001).
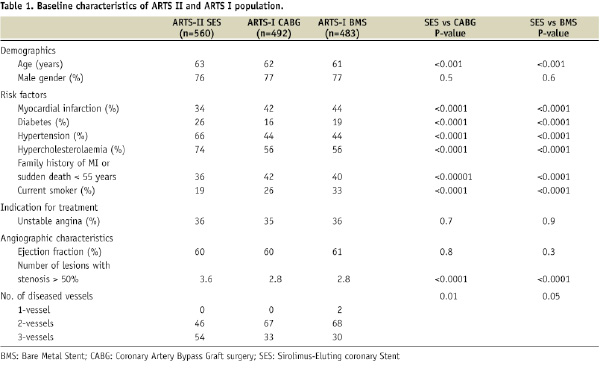
The time course of recovery from revascularisation was similar among the three treatment groups (Figure 1).
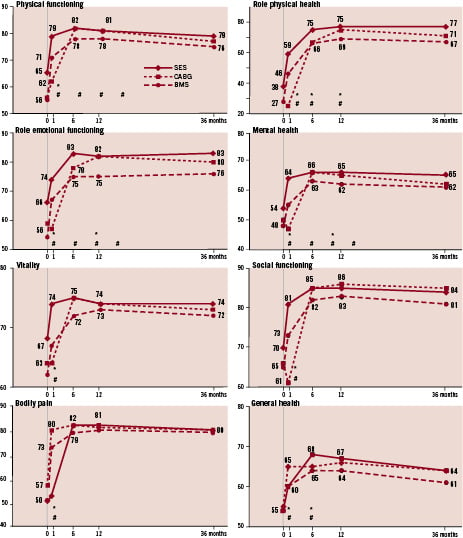
Figure 1. The eight SF-36 quality-of-life subdomain measures (vertical axis) at baseline and at 1, 6, 12 and 36 months (horizontal axis) according to SES (solid line), CABG (dotted line) and BMS (dash line). Higher scores indicates better quality-of-life. * P-value<0.05 comparing DES and CABG. # P-value<0.05 comparing DES and BMS
All three types of revascularisation showed substantial improvement over the first year in all HRQL aspects. In the first post-operative month, patients undergoing CABG experienced a decrease in all HRQL sub-domains, whereas HRQL significantly increased immediately after SES and BMS. However, from baseline to one month this increase was twice as high after SES than after BMS in three sub-domains (emotional well-being, energy and social functioning) (p<0.01) and in the other five subscales this increase was 25% to 50% higher after SES than after BMS (p<0.05). Between one and six months, most HRQL subscales further improved substantially, but by far the strongest after CABG. After adjustment for baseline SF-36 scores and median differences of all eight sub-domains between SES and CABG from baseline to six months was 2 points (range 0 to 6 points) and between SES and BMS the unadjusted median difference was 3 points (range 0-11 points) in favour of SES. After adjustment for baseline SF-36 scores the differences were 1 point (range -2 to 4 points) for SES vs CABG and 2 points (range 0-9 points) in favour of SES.
Ultimately, at six months, the CABG patients attained the same HRQL level as the SES patients but, due to restenosis, the BMS patients remained behind and reached lower HRQL (p<0.05). After six months and up to 36 months, the HRQL scores remained in general unchanged with higher HRQL in the SES and CABG population compared with the BMS population.
Anginal status
The incidence of anginal status is shown in Figure 2.
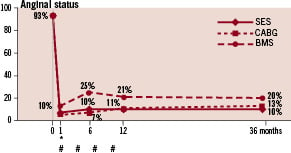
Figure 2. Anginal status (vertical axis) at baseline and at 1, 6, 12 and 36 months (horizontal axis) according to SES (solid line), CABG (dotted line) and BMS (dash line). Lower scores indicates less angina. * P-value<0.05 comparing DES and CABG. # P-value<0.05 comparing DES and BMS
All patients experienced an early significant relief of angina after revascularisation. At one month, 90% of all patients were free from angina. After SES and CABG this incidence remained low up to 36 months. However, due to restenosis, the incidence of angina increased after BMS in the first year up to 25%. At three years only 10% of the SES patients suffered from angina vs. 13% of the CABG patients (p=NS), while after BMS, this number doubles (21%; p<0.05).
Discussion
Assessment of health related quality-of-life has become increasingly important as not only the clinician’s view of the technical success, but also the patient’s perception is being measured. Both stenting and CABG resulted in a significant improvement in HRQL and anginal status. With the introduction of drug-eluting stents with subsequent reduction of restenosis HRQL after SES was significantly improved as compared with BMS, and was similar with CABG, despite the higher clinical risk profile of the SES cohort. During the 3-year follow-up of the present study, SES patients experienced significant greater improvement in HRQL and anginal status than BMS patients and was, from six months on, at the same level as the CABG patients. Most of the differences can be attributed to the lower need of repeat revascularisation after SES.
Because all randomised controlled trials have demonstrated equivalent mortality after CABG and PCI, it is important to examine other patient outcomes, particularly patient-reported health status, because differences in these outcomes may help us while considering a specific treatment option for a patient with multivessel disease. Care of patients with severe ischaemia should focus on management of chronic illness, including alleviation of symptoms, improvement of functional capability and retardation of disease progression19. As a result, evidence of a meaningful benefit from the patient’s perspective becomes more and more important to compare the treatment strategies.
Multiple randomised controlled trials have demonstrated improvement of HRQL for both CABG and PCI2-5. In EAST angina was most prevalent in the PTCA group than in the CABG group, and thus more need for anti-ischaemic medication. There was also a strong tendency that CABG patients believed to have recovered more completely than the PTCA population2. RITA reported a marked but similar improved outcome in HRQL after both intervention procedures3. CABRI reported in a small subanalysis no difference in HRQL at 12 months evaluated with the Nottingham Health profile4. In BARI, amongst patients undergoing CABG, improvement in functional class was significantly greater than among those undergoing angioplasty at one year, but this difference was diminished after four years5. Furthermore, no emotional health difference was found throughout the follow-up period. However, in contrast with BARI, where the HRQL and anginal status declined over time, the HRQL in ARTS remained unchanged between six months and three years. However, all these studies dated from the pre-stent era. Since then, only AWESOME, SOS and MASS-II have reported HRQL after stenting and CABG6,7,20. The AWESOME investigators found similar HRQL outcomes at 6-months, and the SOS study reported better HRQL up to one year after CABG6,7. MASS-II compared CABG, stenting and medical treatment19. They concluded that there was a better HRQL in both CABG and PCI as compared with medical treatment at 12 months. However, the CABG group had the most improved HRQL.
The availability of drug-eluting stents today is an important consideration in the choice of treatment. Earlier, we have presumed that the differences in outcome were due to restenosis, as we did in our HRQL ARTS-I report10. In the present study we were indeed able to confirm this. Especially, among those patients at high restenosis risk substantial benefit is obtained with the use of drug-eluting stents.
A major limitation could be that a comparison with a historical cohort is inappropriate and potentially misleading considering the advances in procedural techniques and post-operative treatment over the past decade. Only a true randomised controlled clinical trial can definitively compare CABG with SES. Only the recently completed Syntax trial comparing surgery with paclitaxel-eluting stents in patients with three vessel or left main disease patients may resolve this matter.
Conclusion
HRQL was improved in both stenting and CABG. There was a trend in better HRQL after CABG as compared with BMS, but up to six months, HRQL after SES was better than CABG and identical with CABG during longer follow-up. Based purely on HRQL outcomes, there seems no reason to prefer CABG to PCI using SES in order to gain a greater HRQL. Ultimately, the selection of either treatment modality should be made on an individual, patient-by-patient, basis.

