A 79-year-old woman with severe aortic stenosis and progressive dyspnoea was referred to our centre for transcatheter aortic valve implantation (TAVI). An echocardiogram revealed normal left ventricular function with concentric left ventricular hypertrophy and severe, heavily calcified, aortic stenosis (mean gradient 82 mmHg; valve area 0.85 cm2). On cardiac catheterisation a “peak-to-peak” aortic valve gradient of 97 mmHg was demonstrated (Figure 1A), and a 26 mm CoreValve® (Medtronic, Minneapolis, MN, USA) was successfully implanted. However, immediately after the intervention, a severe intraventricular gradient was found (Figure 1B). As this gradient completely disappeared at the valvular level (Figure 1C), it was interpreted as catheter entrapment in the setting of hypovolaemia and transient haemodynamic instability. A transoesophageal echocardiogram confirmed a normal function of the CoreValve (Figure 1D [arrows], Moving Image 1) but, unexpectedly, disclosed complete systolic obliteration of the left ventricular cavity (Moving image 2, Moving image 3) causing major obstruction (turbulent flow) at the mid ventricular level and outflow tract (Figure 1E, Moving image 4). The characteristic morphology of a “dynamic” intraventricular gradient (120 mmHg), with a “late peaking” pattern (curved arrows) identical to that previously elicited in the haemodynamic suite, was readily depicted (Figure 1F). No significant systolic anterior motion of the mitral valve was found. The patient remained asymptomatic and eventually she was discharged seven days later with a persisting dynamic intraventricular gradient (90 mmHg) despite increasing doses of beta-blockers.
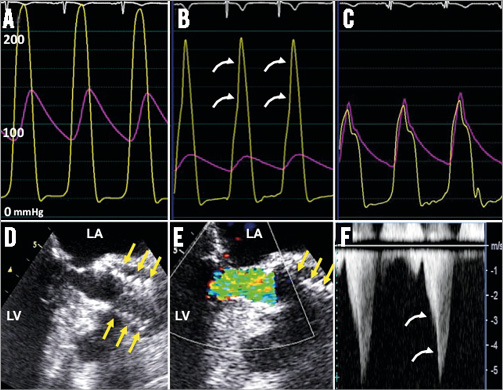
Figure 1. Top: Pressure tracings. Bottom: Echocardiographic and Doppler findings. A) Aortic and left ventricular pressures before TAVI. B) Aortic and left ventricular pressures immediately after TAVI. Notice the late-peaking intraventricular gradient. C) Absence of gradient at the aortic valve level. D) Transoesophageal echocardiogram showing the implanted valve (yellow arrows). E) Turbulent flow in the left ventricular outflow tract. F) Dynamic intraventricular gradient on continuous wave Doppler. LA: left atrium; LV: left ventricle
Our findings demonstrate that severe intraventricular dynamic gradients may emerge after TAVI. The pathophysiology of this phenomenon appears to be similar to that typically described in the postoperative period of rare patients following surgical aortic valve replacement.
Conflict of interest statement
R. Trillo is proctor for the Medtronic CoreValve. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Transoesophageal echocardiography revealing a normal function of the aortic valve after TAVI.
Moving image 2. Transgastric longitudinal view of the left ventricle disclosing the left ventricular hypertrophy and systolic cavity obliteration after TAVI.
Moving image 3. Transgastric short-axis view of the left ventricle showing similar findings.
Moving image 4. Colour Doppler depicting the intraventricular turbulent flow after TAVI.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Transoesophageal echocardiography revealing a normal function of the aortic valve after TAVI.
Moving image 2. Transgastric longitudinal view of the left ventricle disclosing the left ventricular hypertrophy and systolic cavity obliteration after TAVI.
Moving image 3. Transgastric short-axis view of the left ventricle showing similar findings.
Moving image 4. Colour Doppler depicting the intraventricular turbulent flow after TAVI.