Abstract
Aims: Obstructive pelvic arterial lesions are highly prevalent in patients with erectile dysfunction and commonly located in penile artery segments. In this first-in-man study, we intended to assess the safety and feasibility of balloon angioplasty for isolated penile artery stenoses in patients with erectile dysfunction.
Methods and results: Twenty-five patients with erectile dysfunction and isolated penile artery stenoses (unilateral stenosis ≥70% or bilateral stenoses ≥50%) identified by pelvic computed tomographic angiography were enrolled. A total of 20 patients (mean age 61 years [range, 48-79 years]) underwent balloon angioplasty. Three patients had bilateral penile artery stenoses. Procedural success was achieved in all 23 penile arteries, with an average balloon size of 1.6 mm (range, 1.00-2.25 mm). The average International Index for Erectile Function-5 (IIEF-5) score improved from 10.0±5.2 at baseline to 15.2±6.7 (p<0.001) at one month and 15.2±6.3 (p<0.001) at six months. Clinical success (change in the IIEF-5 score ≥4 or normalisation of erectile function [IIEF-5 ≥22]) was achieved in 15 (75%), 13 (65%), and 12 (60%) patients at one, three, and six months, respectively. There were no adverse events through follow-up.
Conclusions: For the first time we demonstrated that penile artery angioplasty is safe and can achieve clinically significant improvement in erectile function in 60% of patients with erectile dysfunction and isolated penile artery stenoses.
Introduction
Erectile dysfunction is a common disorder that mainly affects men older than 40 years of age1. It has been assumed that erectile dysfunction is generally of a mixed psychogenic and organic nature. Among the organic causes of erectile dysfunction, at least five sectors have been identified: neurogenic, hormonal, arteriogenic, cavernosal/venogenic, and drug-induced1,2. Based on collective results from previous invasive angiographic studies, the majority of patients with erectile dysfunction (~75%) had stenotic lesions in the ilio-pudendal-penile arterial system3,4, which provides the arterial inflow to the penis. This finding, together with the fact that erectile dysfunction shares common risk factors with cardiovascular disease, often co-exists with cardiovascular disease, and is an independent risk factor for future cardiovascular events1,2,5, suggests that the arteriogenic cause plays a dominant role in the pathogenesis of erectile dysfunction.
Theoretically, stenotic lesions could be anywhere in the ilio-pudendal-penile arterial system in patients with arteriogenic erectile dysfunction. However, previous angiographic studies have shown that most arterial stenoses are present in the common penile and internal pudendal arteries4,6,7. By using non-invasive multi-detector computed tomographic (CT) angiography, we confirmed this finding by showing that approximately 90% of stenotic lesions were located in the common penile and internal pudendal arteries in 80 patients with erectile dysfunction8. Moreover, the obstructive lesions were limited to the penile artery segments in ~30% of patients with arteriogenic erectile dysfunction, whereas ~15% of them had their obstructive lesions limited to the internal pudendal arteries. The recently published Zotarolimus-Eluting Peripheral Stent System for the Treatment of Erectile Dysfunction in Males with Suboptimal Response to PDE5 Inhibitors (ZEN) trial demonstrated the safety and feasibility of endovascular stenting for stenotic lesions in the internal pudendal artery9. The ZEN trial also revealed the limitation of isolated internal pudendal artery intervention because only 8% of subjects screened were qualified to undergo interventional therapy. This number is consistent with the frequency of isolated internal pudendal artery stenoses among patients with erectile dysfunction across different imaging studies6-8. In fact, penile artery stenoses are more prevalent in patients with arteriogenic erectile dysfunction6-8 and, if left untreated, can obviously compromise the therapeutic effects of endovascular treatment restricted to stenotic lesions proximal to the common penile artery. The average diameters of the penile and internal pudendal arteries are 1-2 mm and 2-3 mm, respectively1,2. With the advent of interventional technology, even the smaller penile artery is now amenable to endovascular angioplasty.
In this first-in-man PElvic Revascularisation For arteriogenic EreCTile dysfunction (PERFECT-1) study, we intended to assess the safety and feasibility of catheter-based therapy for isolated penile artery stenoses in patients with erectile dysfunction. To improve the efficacy of patient selection, non-invasive CT angiography was used as the screening tool to identify potential candidates.
Methods
STUDY DESIGN
From December 2012 through August 2013, consecutive patients with symptoms of erectile dysfunction were screened for enrolment in this prospective, unblinded, single-arm, single-centre first-in-man PERFECT-1 study. All patients were invited to complete a five-item brief form of the International Index for Erectile Function (IIEF-5) questionnaire, which has been extensively validated as a useful instrument for erectile function assessment10,11. Responses to the five questions range from 1 (worst) to 5 (best). Questions 2 to 5 may be graded 0 if there is no sexual activity or no sexual intercourse attempt. The final score ranges from 1 to 25 points, with values ≤21 being diagnostic of erectile dysfunction. Erectile dysfunction could be further categorised as mild (IIEF-5 score 17 to 21), mild to moderate (12 to 16), moderate (8 to 11), and severe (7 or less). Patients with an IIEF-5 score of 5 to 21 and having at least two intercourse attempts each month with the same single partner in the previous three months were diagnosed as “having an active sex life despite the presence of erectile dysfunction” and then evaluated by comprehensive medical and sexual history and physical examination, hormonal testing, and pelvic CT angiography by a multidisciplinary team consisting of interventional cardiologists, a radiologist, and urologists with expertise in sexual medicine. All eligible patients were asked to take phosphodiesterase-5 inhibitors for at least two intercourse attempts to ensure their erectile function could not achieve an IIEF-5 score ≥22 by pharmacological therapy alone. After completion of all these diagnostic investigations, patients were invited to take a second IIEF-5 assessment. All patients provided written informed consent approved by the ethics committee of the National Taiwan University Hospital.
Pelvic CT angiography was performed by using a 64-detector row CT scanner (LightSpeed VCT; GE Healthcare, Milwaukee, WI, USA) with premedication of 0.6 mg sublingual nitroglycerine8 (details are reported in the Online Appendix). The whole pelvic arterial system supplying the penis (from the pelvic aorta to the dorsal penile and cavernosal arteries) was identified and systemically assessed (Figure 1A, Figure 1B).The clinical inclusion criterion was men 20 years of age or older with “consistent” erectile dysfunction defined as both IIEF-5 scores, taken at least four weeks apart, being in the range of 5 to 21 points and with a difference of ≤2 points. The anatomical inclusion criteria, based on pelvic CT angiography, were unilateral luminal diameter stenosis ≥70% or bilateral diameter stenoses ≥50% in the common penile artery, cavernosal artery, or dorsal penile artery proximal to the first cavernosal artery, a target lesion reference vessel diameter ≥1.0 mm, and a target lesion length ≤30 mm (Figure 2A-Figure 2F). The exclusion criteria are detailed in the Online Appendix.
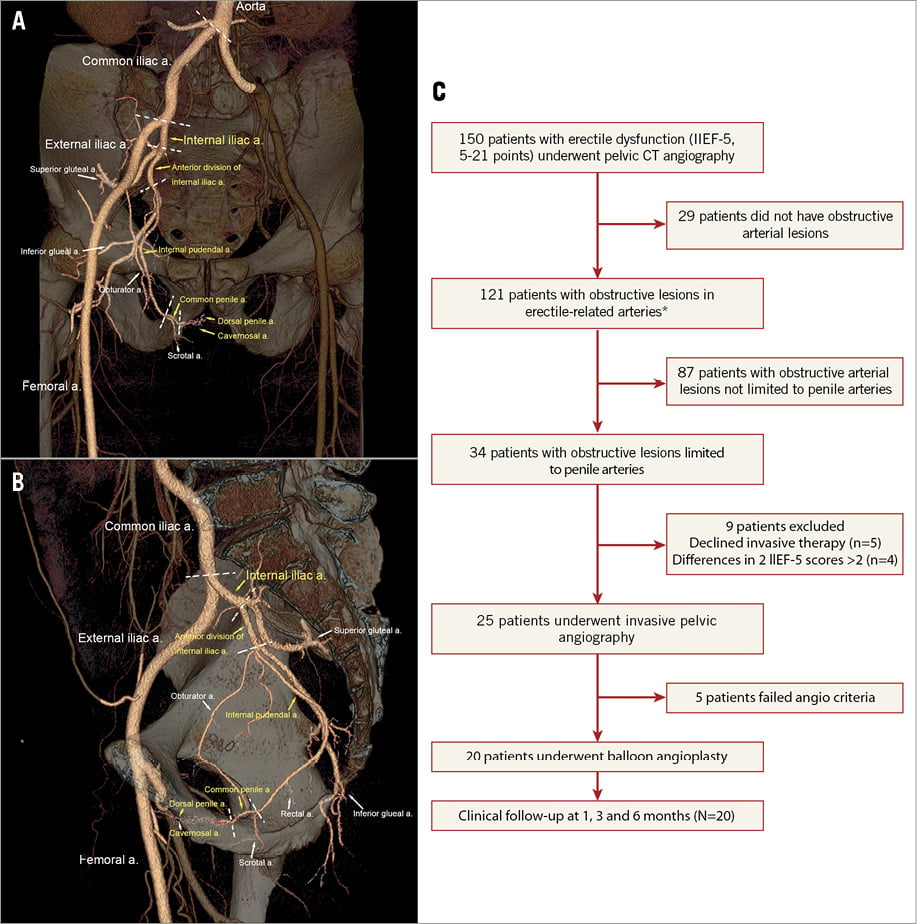
Figure 1. Pelvic CT angiography showing the anatomy and nomenclature of the whole pelvic arterial system and study flow chart. A) Three-dimensional volume-rendered (VR) reconstruction of the right-sided pelvic arteries (anterior view). Erectile-related arteries are labelled by yellow-coloured characters, non-erectile-related arteries are labelled by white-coloured characters. There are three major branches of internal iliac artery (superior gluteal artery, inferior gluteal artery, and internal pudendal artery). The terminal branches of the internal pudendal artery are the perineal-scrotal artery and the common penile artery. The common penile artery gives rise to the dorsal penile and cavernosal arteries. B) Oblique lateral VR reconstruction of the right-sided pelvic arteries. C) Study flow chart. *Erectile-related arteries are those labelled by yellow-coloured characters shown in A) and B).
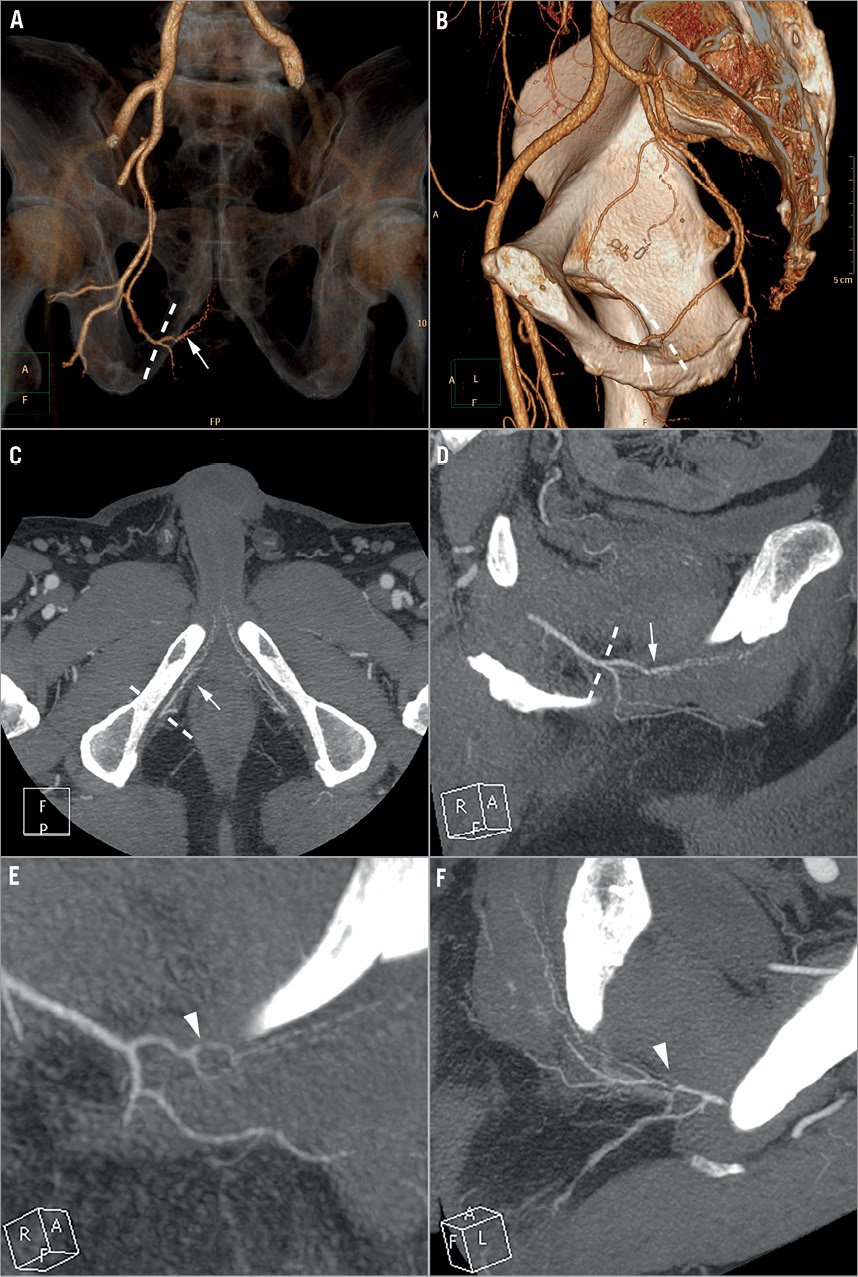
Figure 2. Pelvic CT angiography showing the penile arteries. A) Three-dimensional volume-rendered (VR) reconstruction of the right-sided arteries supplying the penis (anterior view with caudal 30 degree angulation). B) Oblique lateral VR reconstruction of the right-sided pelvic arteries. C) Axial thin-slab maximal intensity projection (MIP) of the penile arteries. D) Oblique MIP view of the penile arteries. E) Oblique MIP view of a case with focal stenosis (arrowhead) in the right common penile artery. F) Oblique MIP view of a case with focal stenosis (arrowhead) in the left common penile artery.
INTERVENTIONS
Selective angiography and penile artery interventions were performed percutaneously by an over-the-bifurcation (for the contralateral lesions) or a retrograde (for the ipsilateral lesions) approach via a single femoral vascular access with the use of a 6 Fr sheath. Details of angiographic projections are reported in the Online Appendix. We routinely engaged the proximal internal pudendal artery by using a 5 Fr diagnostic catheter and obtained the selective angiograms following intra-arterial administration of 150-200 µg of nitroglycerine to achieve maximal dilatation of the common penile artery and its branches. Use of any phosphodiesterase-5 inhibitor within 72 hours of the procedure was prohibited.
Patients could proceed with investigational angioplasty if their quantitative angiographic results fulfilled the following angiographic inclusion criteria: 1) unilateral diameter stenosis ≥70% or bilateral diameter stenoses ≥50% in the common penile artery, cavernosal artery, or dorsal penile artery proximal to the first cavernosal artery, 2) a target lesion reference vessel diameter ≥1.0 mm, and 3) a target lesion length ≤30 mm. Patients were excluded if there was ≥50% stenosis in the ilio-pudendal-penile arterial system proximal to the common penile artery.
After confirmation of angiographic eligibility, patients received 8,000 U of heparin to maintain an activated clotting time ≥250 s. All patients received aspirin (100 mg daily) and clopidogrel (75 mg daily and 300 mg loading one day before intervention) prior to the procedure. Selective engagement of the internal pudendal artery was performed with an appropriately shaped 5 Fr guiding catheter. A 0.014-inch steerable guidewire was advanced across the stenosis and standard interventional techniques were applied to treat the lesion. In order to prevent inadvertent dissection, we routinely started with a balloon catheter with a diameter of 1.0 mm and ended with a balloon catheter with the size approximately equal to the reference vessel diameter. Each balloon was inflated at 10 to 12 atm for a total of at least two minutes. After dilatation of the entire target lesion, biplane angiograms were obtained. Once flow-limiting dissection was noted, prolonged (more than two minutes) balloon dilatation was performed. Technical success was defined as residual diameter stenosis ≤30% and adequate distal run-off.
After intervention, two doses of subcutaneous enoxaparin (1 mg/kg) were administered. Post-procedural antiplatelet therapy included aspirin (100 mg daily) indefinitely and clopidogrel (75 mg daily) for three months.
STUDY ENDPOINTS
The primary endpoints were determined with regard to safety and clinical efficacy. The primary safety endpoint was the rate of major adverse events within one month after intervention, defined as procedure-related death, occurrence of perineal haematoma, gangrene or necrosis (glans penis, penile shaft, scrotal, or anal), or the need for subsequent perineal, penile, or anal surgery (including target lesion or vessel revascularisation or arterial embolisation procedures). The primary feasibility endpoint was the change of IIEF-5 score from baseline to six months following intervention. All patients were asked to maintain at least the same levels of sexual activity and phosphodiesterase-5 inhibitor use (if any) after the procedure to ensure the comparability of erectile function assessments (IIEF-5 scores).
The secondary endpoints included: the rates of major adverse events at three and six months; the rates of clinical success defined as the change in the IIEF-5 score from baseline by ≥4 points or IIEF-5 ≥22 at one, three, and six months; the rates of IIEF-5 ≥22, indicative of normalisation of erectile function, at one, three, and six months; and the rates of clinical worsening defined as the decrease in the IIEF-5 score from baseline by ≥4 points or IIEF-5 <5 at one, three, and six months. A change of ≥4 points in the IIEF-5 score was deduced as clinically significant for assessing the therapeutic effects on erectile function (details are reported in the Online Appendix).
STATISTICAL ANALYSES
We estimated that 23 patients would need to be enrolled for the study to have a statistical power of 80% and a two-sided p-value of 0.05 to detect an absolute difference in IIEF-5 of four points10-12, given an assumed difference in IIEF-5 of six after penile artery angioplasty, an expected variance of nine for IIEF-5 in patients with erectile dysfunction13, and a positive predictive value for pelvic CT angiography of 80%. Categorical variables were summarised as counts or percentages and compared using Pearson’s chi-square test. Continuous variables were presented as mean±SD and compared using the independent samples t-test. Baseline IIEF-5 score was the average of two IIEF-5 scores obtained in the screening periods. To assess the therapeutic effect on IIEF-5 scores10, a paired t-test was used. Data analyses were performed with SPSS software package version 12.0 (SPSS, Chicago, IL, USA). A p-value <0.05 was considered significant.
Results
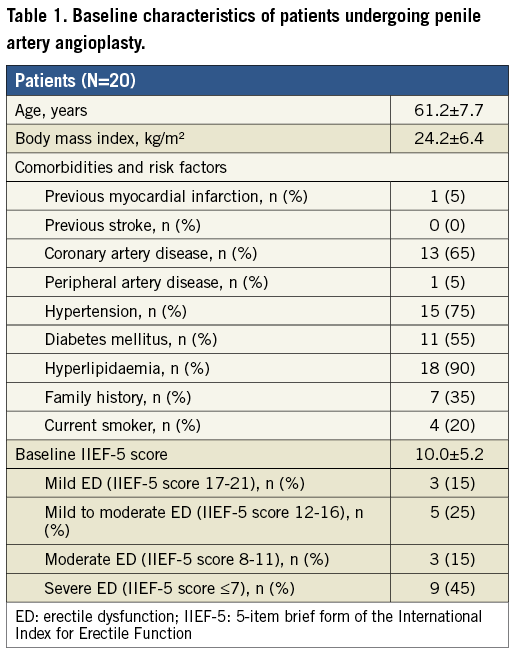
A total of 25 patients fulfilling the clinical and anatomical inclusion criteria based on pelvic CT angiography underwent invasive angiography to assess their eligibility for penile artery intervention. Five patients were excluded from the procedure because of insufficient penile artery disease following intra-arterial administration of nitroglycerine (n=5, 20%). The study flow chart is shown in Figure 1C. Baseline characteristics of the 20 patients undergoing penile artery angioplasty are shown in Table 1. The mean age was 61.2 (range 48 to 79) years. Cardiovascular risk factors were prevalent in the study patients and approximately two thirds had a history of coronary artery disease, reflecting the fact that most of the study patients were identified from a cardiovascular practice setting. The mean IIEF-5 score was 10.0.
The angiographic characteristics of the stenotic penile arteries are shown in Table 2. Three patients had bilateral penile artery stenoses. Among the 29 segmental stenotic lesions, 17 (59%) were located in the common penile artery, 11 (38%) in the dorsal penile artery proximal to the first cavernosal artery, and only one (3%) in the ostium of the cavernosal artery. The average diameter of the proximal reference vessels was 1.5 mm (range 1.0 to 2.25 mm). The mean lesion length was 10.5 mm (range 2.4 to 24.8 mm). No lesions were ulcerated, thrombotic, or calcified.
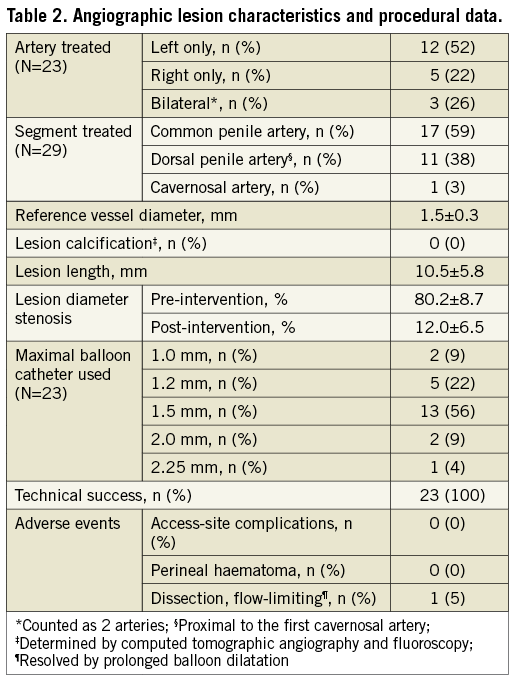
Technical success was achieved in all 23 vessels. There was one case in which flow-limiting dissection developed after dilating the stenotic common penile artery lesion with a 1.2 mm balloon catheter. After prolonged dilatation with the same balloon catheter, adequate distal run-off was established. The most commonly used maximal balloon catheter size was 1.5 mm, which was consistent with the mean reference vessel size. Two case examples are shown in Figure 3 and Online Figure 1.
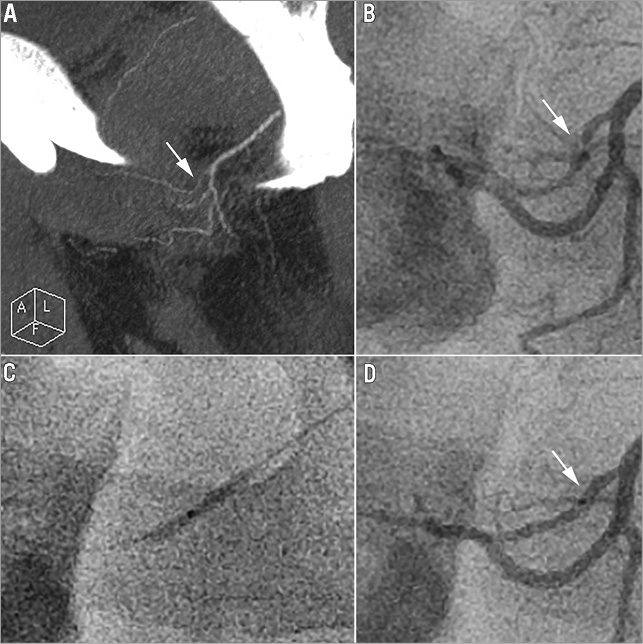
Figure 3. Case example. A 61-year-old man with progressive erectile dysfunction for 2 years. A) CT angiography in oblique MIP view showed focal stenosis (arrow) in the left common penile artery. B) Selective invasive angiography in LAO 60 degree projection revealed a stenotic lesion in the same location as shown in CT angiography. C) Angioplasty of the left common penile artery using a 1.5 mm-diameter balloon catheter. D) After angioplasty, there was no residual stenosis. The patient’s IIEF-5 score improved from 17 (at baseline) to 25 (at one and three months) and 22 (at six months).
FOLLOW-UP
Complete follow-up data were obtained from all 20 patients at one, three, and six months. For the primary safety endpoint, there were no major adverse events within one month or during the six months of follow-up (Table 3). For the primary feasibility endpoint, the IIEF-5 score was significantly increased by 5.2 points (95% CI: 3.0-7.4) from baseline to six months. Clinical success was achieved in 75%, 65%, and 60% of 20 patients at one, three, and six months, respectively. Likewise, IIEF-5 ≥22 was achieved in 20%, 20%, and 15% of 20 patients at one, three, and six months, respectively. Despite the fact that the number of patients with clinical success gradually decreased, the post-procedure IIEF-5 scores and their changes did not decline during the six months of follow-up (Figure 4). Gradual decreases in IIEF-5 scores were observed in four (27%) out of the 15 patients who achieved clinical success at one month, whereas gradual increases in IIEF-5 scores were observed in another four clinical responders. There was no one who did not achieve clinical success at one month who achieved clinical response later on. There were no significant differences in baseline and lesion characteristics between patients with and without clinical success at six months (data not shown). There was no case of clinical worsening or need for reintervention during the six months of follow-up. There were no significant changes in IIEF-5 scores from baseline to six months among the five patients not undergoing angioplasty because of insufficient disease (data not shown).
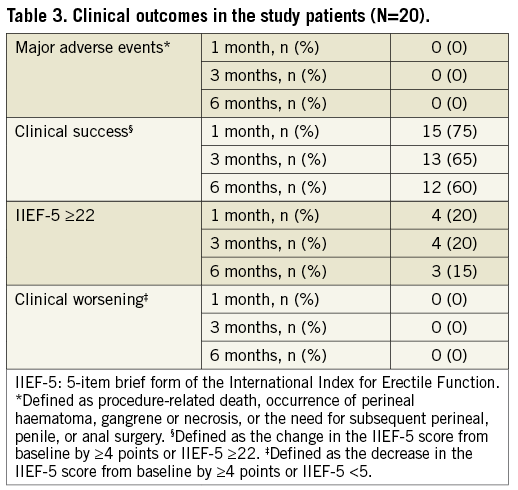
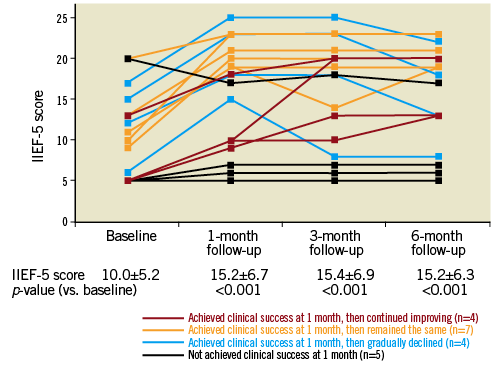
Figure 4. Results of IIEF-5 scores over time. IIEF-5: 5-item brief form of the International Index for Erectile Function.
Discussion
In this study, we demonstrated for the first time that penile artery angioplasty is safe and feasible and can achieve clinically significant improvement in erectile function in 60% of patients with erectile dysfunction not initially responsive to phosphodiesterase-5 inhibitors and with isolated penile artery stenoses. This improvement in the IIEF-5 score (5.2 points) is numerically greater than the average IIEF-5 improvement (2.1 points) shown in a meta-analysis of three clinical trials evaluating lifestyle interventions or pharmacotherapy with statins in patients with erectile dysfunction not responsive to phosphodiesterase-5 inhibitors14. Compared to previous reports of endovascular therapy for arteriogenic erectile dysfunction3,9,15, our PERFECT-1 study is not only the first to extend the realm of endovascular angioplasty to the penile artery and its major branches (dorsal penile artery and cavernosal artery), but it also demonstrates three refinements in the whole interventional setting, namely, application of pelvic CT angiography, intra-arterial nitroglycerine use, and routinely beginning with a1.0 mm-diameter balloon catheter.
Despite the fact that erectile-related arterial insufficiency has been widely recognised as an important cause of erectile dysfunction, there are relatively few studies to have assessed the feasibility of using non-invasive CT angiography as a diagnostic tool for patients with erectile dysfunction4,16-18. Doppler ultrasound with intracavernosal vasodilator injection is the most studied non-invasive diagnostic tool for arteriogenic erectile dysfunction19. However, it could not provide information about the topography and pathology of the entire ilio-pudendal-penile arterial system proximal to the cavernosal artery and may cast psychological stress upon patients because of fear and pain incurred by direct penile injection. Previous studies assessing the diagnostic accuracy of pelvic CT angiography have shown that CT angiography can clearly delineate the anatomic features of the internal pudendal artery, but not the common penile artery4,17. In this study, we further extend the diagnostic capability of multi-detector CT angiography down to the level of the common penile artery and its major branches by using the 64-detector row CT scanner. Compared to the coronary arteries which are located on the beating heart, pelvic arteries which remain still in place could be visualised with a better spatial resolution by CT angiography. We herein demonstrated that vessels with a diameter of 1 mm or less like the dorsal penile artery and the proximal cavernosal artery could be finely displayed by current multi-detector CT angiography together with the sliding-thin-slab maximum intensity projections reformation technique20. Given that the penile artery and its branches are not fully dilated while the penis is in the flaccid state, sublingual nitroglycerine, rather than intracavernosal vasodilator injection, was routinely given before CT angiography. Some patients who were diagnosed as having significant stenosis in penile arteries by CT angiography were excluded from angioplasty because of insufficient penile artery disease following intra-arterial nitroglycerine administration during invasive angiography, suggestive of suboptimal dilatation of distal penile arteries by sublingual nitroglycerine in a certain number of cases. However, the positive predictive value in the present study was 80% (20/25), superior even to that of the internal pudendal artery (60-70%) reported in previous CT angiographic studies with pre-procedural intracavernosal vasodilator injections17,18.
There is considerable variation in the origin of the internal pudendal artery and the presence of accessory vascular supply to the dorsal penile and cavernosal arteries18. Pelvic CT angiography can provide a clear roadmap to guide interventional therapy and the best projection angles for visualising the lesions, which may save a great deal of time and amount of contrast used during an interventional procedure. Another strength of CT angiography is to detect the presence of calcification or thrombus in vascular stenotic lesions before endovascular therapies. It is noteworthy that there was no calcification or thrombus in any penile arterial stenotic lesion in the present study. This finding suggests that the tissue characteristics of all these lesions were favourable for balloon angioplasty. Whether these tissue features are universal for most penile arterial stenotic lesions awaits further verification.
Intracavernosal vasodilator injection to achieve optimal dilatation of cavernosal arteries was generally performed before diagnostic pelvic angiography and endovascular therapy for internal pudendal artery stenosis6,7,9,17. Because of this, the term “pharmaco-arteriography” has been used exclusively to describe pelvic angiography with intracavernosal vasodilator injection21. Nevertheless, intracavernosal vasodilator injection is not without risk and may cause adverse events like priapism, prolonged erection, faulty injection, and pain2. In this study, we found that the administration of intra-arterial nitroglycerine (150-200 µg) was able to achieve significant dilatation of the common penile artery and its branches in all 25 patients. However, it is still premature to pronounce that intra-arterial nitroglycerine could achieve “optimal” dilatation of the common penile artery and its distal branches since there is still no head-to-head comparison between intra-arterial nitroglycerine and intracavernosal vasodilator injection regarding their capability to achieve adequate vasodilatation in erectile-related arterial beds. Furthermore, incomplete vasodilatation could result in overestimation of the angiographic results following angioplasty since the reference segment would be smaller than its real size. We noticed that both the internal pudendal artery and the common penile artery were easy to spasm whenever either a guidewire or a diagnostic or guiding catheter touched their lumen. Therefore, it is mandatory to administer intra-arterial nitroglycerine during pelvic diagnostic or interventional procedures to avoid overestimation of the severity of stenosis in these erectile-related arteries. Moreover, we highly recommend using pelvic CT angiography to help discriminate the true stenotic lesions from pseudolesions caused by inadvertent vasospasm during selective pelvic angiography.
In our previous experience, we noticed that, compared to coronary arteries, the distal internal pudendal artery and common penile artery were more prone to developing dissection if we directly used a balloon catheter with a diameter similar to the reference vessel size for balloon angioplasty. We therefore routinely started with a balloon catheter with a diameter of 1.0 mm and cautiously upgraded the size of balloon catheter to achieve optimal vasodilatation for penile artery angioplasty. Using this strategy, only one out of 20 patients developed a flow-limiting dissection, which was resolved by prolonged balloon dilatation. Although the dissection-prone phenomenon of small pelvic arteries might only be due to oversizing of the balloon catheter used for angioplasty, another speculative reason for this intriguing finding is that there might be differences in certain characteristics of the artery and surrounding tissues (like perivascular adipose tissue) between different arterial beds22,23. In keeping with this speculation, the ZEN trial showed a much higher six-month restenosis rate (34%) with the use of drug-eluting stents in the internal pudendal artery than in the coronary artery (9.2%)9,24, suggestive of a differential tissue response pattern to stenting across different arterial beds.
The 60% six-month clinical success rate for penile artery angioplasty in our patients with erectile dysfunction and isolated penile artery stenosis is very close to that achieved in the ZEN trial. In the ZEN trial, 59.3% of 27 patients with erectile dysfunction and isolated internal pudendal artery stenosis achieved a change in IIEF-Erectile Function domain ≥4 points at six months following internal pudendal artery stenting9. With regard to the serial post-intervention IIEF changes, both our study and the ZEN trial showed persistent improvement in IIEF scores in patients undergoing penile artery and internal pudendal artery angioplasty, respectively. Furthermore, we demonstrated a heterogeneous pattern of IIEF-5 changes following penile artery intervention among those clinical responders. After one month, one quarter of clinical responders experienced a gradual decline in erectile function, another quarter experienced further improvement, whereas the rest (one half) had persistent improvement. In keeping with the speculation that balloon angioplasty alone in smaller arteries might be associated with a higher restenosis rate, we observed a trend towards a higher restenosis rate, as nine (45%) out of the 20 treated patients were either non-responsive (n=5) or had a gradual decline in erectile function (n=4). A decline in clinical response might suggest the presence of a placebo effect or the occurrence of restenosis, which will be elucidated by follow-up CT angiography scheduled at six to nine months following angioplasty in this study. A further increase in erectile function suggests that distal vascular remodelling takes time in certain patients after the resumption of normal penile arterial inflow, a finding similar to the myocardial perfusion scan response following coronary interventions25.
Limitations
There are several limitations in this study. First, the sample size in this first-in-man study was small, though it fulfilled the statistical requirement according to our pre-specified sample size estimation. Second, there was no control arm in this study. We therefore cannot exclude the possibility that placebo or Hawthorne effects might have contributed to the therapeutic benefits. Nevertheless, the absence of significant changes in the IIEF-5 scores in the five patients enrolled but not undergoing angioplasty indicates that the improvement in IIEF-5 might be real. Third, both IIEF-5 and IIEF-Erectile Function domain have been widely used to evaluate the efficacy of interventions for erectile dysfunction10,14,26. Despite the fact that nearly identical diagnostic capabilities of both assessment tools have been reported10, it is still not certain whether results from both tools serving as efficacy measures are comparable. Fourth, objective penile blood flow assessments like duplex ultrasonography were not routinely performed prior to intervention in this study. Thus, patients with concomitant venogenic erectile dysfunction may have been included in this study. We herein for the first time used pelvic CT angiography as the screening tool and achieved a high inclusion rate (80%) and clinically significant improvement in erectile function in 60% of patients, suggesting that an arterial cause might be the dominant factor in causing erectile dysfunction. It has also been shown that there was only moderate agreement between penile duplex ultrasonography and invasive penile angiography as well as the presence or severity of erectile dysfunction6,27,28. It is still not certain whether a duplex ultrasonography-based approach or a pelvic CT angiography-based approach is more effective in identifying potential candidates who will benefit from endovascular therapy for erectile dysfunction. Fifth, the unavailability of follow-up CT angiography at the present stage precludes further exploration of the associations between anatomical changes of penile arterial obstructive lesions and changes in erectile function. Lastly, only subjective assessment of erectile function (IIEF-5 questionnaire) was used as the endpoint measurement in this study. To improve the reliability of this subjective assessment, we excluded patients with differences in the two pre-procedural IIEF-5 scores >2 points (Figure 1C). The reliability of IIEF-5 in our study patients is also reflected in the absence of significant changes in follow-up IIEF-5 scores in the five patients not qualified to undergo angioplasty.
Conclusions
Penile artery angioplasty for patients with erectile dysfunction and isolated penile artery stenoses was shown to be safe and feasible and resulted in clinically significant improvement in erectile function in 60% of patients in this PERFECT-1 study. Pelvic CT angiography provides a clear roadmap of the whole pelvic arterial system, tissue characteristics of stenotic lesions, and an unbiased quantitative assessment of stenotic lesions, and could be used as a guide for endovascular therapies. We simplified the interventional therapy for arteriogenic erectile dysfunction by showing that better pelvic angiography could be obtained by intra-arterial nitroglycerine administration. We recommend that penile artery angioplasty should be performed cautiously by beginning with the smallest balloon catheter since these vessels can easily develop dissection. The long-term durability of penile artery angioplasty is not known and merits further investigation.
| Impact on daily practice Penile artery stenoses are more prevalent in patients with arteriogenic erectile dysfunction and, if left untreated, can obviously compromise the therapeutic effects of endovascular treatment restricted to stenotic lesions proximal to the common penile artery. We herein extend the realm of endovascular angioplasty to the penile artery and its major branches (dorsal penile artery and cavernosal artery) by demonstrating that penile artery angioplasty together with intra-arterial nitroglycerine administration can achieve clinically significant improvement in erectile function in 60% of patients with erectile dysfunction and isolated penile artery stenoses. We also demonstrated that pelvic CT angiography provides a clear roadmap of the whole pelvic arterial system, tissue characters of stenotic lesions, and an unbiased quantitative assessment of stenotic lesions. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Appendix. Methods.
DETAILS OF PELVIC COMPUTED TOMOGRAPHIC (CT) ANGIOGRAPHY AND ITS IMAGING ANALYSES
Contrast bolus tracking with the region of interest in the lower abdominal aorta was used. Biphasic injection of 80 mL of contrast media and 40 mL of saline flush was implemented at a rate of 3 mL/s. Images were reconstructed with 0.625 mm slice thickness and 22 cm field-of-view. CT images were transferred to a dedicated CT workstation (Extended Brilliance Workspace; Philips Medical Systems, Amsterdam, Netherlands) and interpreted by one radiologist (W.-J. L.) with 10 years’ experience of interpreting cardiovascular CT and unaware of the patients’ clinical information.
EXCLUSION CRITERIA
The exclusion criteria included: 1) arterial inflow to the penis entirely from the accessory pudendal arteries rather than the usual internal pudendal artery and common penile artery; 2) the presence of focal diameter stenosis ≥50% in the common iliac artery, internal iliac artery, anterior division of internal iliac artery, or internal pudendal artery; 3) previous radical prostatectomy, pelvic radiation, or Peyronie’s disease; 4) untreated hypogonadism (serum total testosterone <300 ng/dL within 14 days before enrolment); 5) acute coronary syndrome, stroke, or life-threatening arrhythmia within three months before enrolment; 6) poorly controlled diabetes mellitus with glycosylated haemoglobin levels >9%; 7) serum creatinine levels >2.5 mg/dL; 8) bleeding diathesis or known hypercoagulopathy; 9) life expectancy of less than 12 months; and 10) known intolerance to contrast agents.
ANGIOGRAPHIC PROJECTIONS FOR IMAGING THE ERECTILE-RELATED ARTERIES
Biplane selective angiography was performed to evaluate the anatomical features of all erectile-related arteries. Anteroposterior projections were used for the distal aorta and common iliac arteries, contralateral 20-degree oblique projections for the origins of internal iliac arteries, both anteroposterior and ipsilateral straight 60-degree oblique views for the origins of internal pudendal and obturator arteries, both anteroposterior projections with 20-degree cranial angulations and ipsilateral straight (or with caudal angulations) 60-degree oblique projections for the distal internal pudendal and the proximal common penile arteries, and anteroposterior projections with 25-degree caudal angulations and ipsilateral straight (or with cranial angulations) 60-degree oblique projections were best for identification of the distal common penile, dorsal penile, and cavernosal arteries.
RATIONALE FOR THE ADOPTION OF THE IIEF-5 CHANGE OF ≥4 AS CLINICALLY SIGNIFICANT
The concept of minimal clinically important differences (MCID) in erectile function assessment was introduced for the IIEF-Erectile Function (IIEF-EF or IIEF-6) domain12. The MCID for IIEF-6 (6 items) was calculated as the minimal change of IIEF-6 which was in accordance with the minimal improvement in item 7 (an item not included in the IIEF-6) on sexual intercourse satisfaction. The MCID for IIEF-6 was calculated to be 4, which was in accordance with the defined minimal improvement in item 7 (from little or no satisfactory intercourse [either 1, “almost never”, or 2, “a few times”] to satisfactory intercourse sometimes [3, “sometimes”]). As a matter of fact, this item 7 is included in the IIEF-5 but not in the IIEF-6 and is viewed as the central element in the National Institute of Health definition of erectile dysfunction11. The inclusion of item 7 on sexual intercourse satisfaction is a distinguishing feature of the IIEF-5 that is absent from the IIEF-6. In the IIEF-5, the other 4 items are also included in the IIEF-6. Given that the MCID of 4 in IIEF-6 equals the change of 1 (from 2 to 3) or 2 (from 1 to 3) in item 7, we therefore deduced that the clinically significant difference for IIEF-5 (similar to the MCID for IIEF-6) should be 4 as well (4×4/6 [4 out of the 6 items in IIEF-6]+1.5 [item 7]=4.2, close to 4).
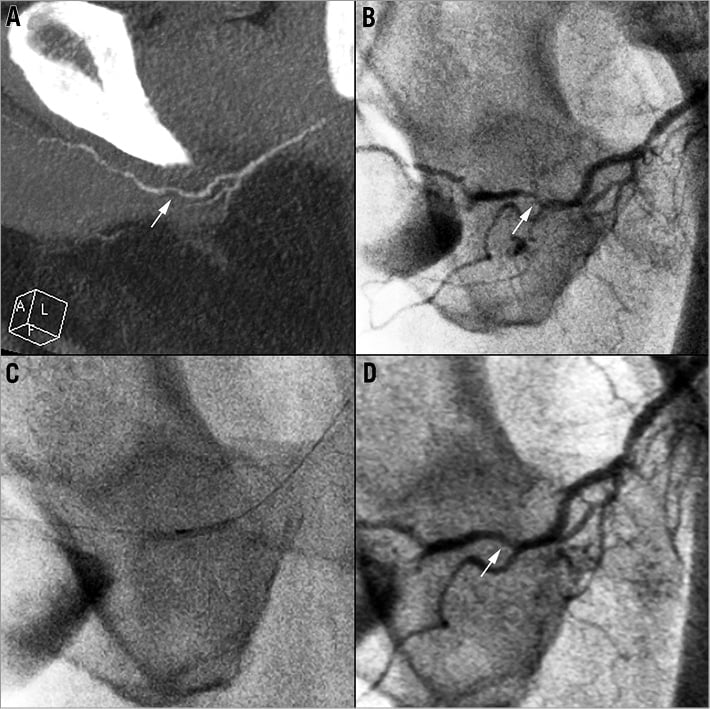
Online Figure 1. Case example. A 67-year-old man with progressive erectile dysfunction for two years. A) CT angiography in oblique MIP view showed focal stenosis (arrow) in the left common penile artery. B) Selective invasive angiography in LAO 60 degree projection revealed a stenotic lesion in the same location as shown in CT angiography. C) Angioplasty of the left common penile artery using a 1.5 mm diameter balloon catheter. D) After angioplasty, there was no residual stenosis. The patient’s IIEF-5 score improved from 13 (at baseline) to 19 (at 1, 3, and 6 months).

