A major focus of cardiovascular medicine is to prevent, diagnose, and relieve vascular stenoses. We know that many of our patients suffer from erectile dysfunction (ED). Therefore, it is no surprise that several recent investigations have focused on the identification and interventional treatment of arterial disease that might be contributing to erectile dysfunction. The quest for a vascular intervention to improve erectile function continues in the PElvic Revascularization For arteriogenic EreCTile dysfunction (PERFECT-1) study by Wang and colleagues1 from Taiwan in this issue of EuroIntervention.
This novel study explores the use of computed tomographic angiography (CTA) to identify distal vascular stenoses that may be related to insufficient penile arterial inflow and therefore ED. Patients with common penile artery stenoses identifiable by CTA were taken for invasive angiography. Small balloon angioplasty was performed if possible (87% of lesions were treated with a ≤1.5 mm balloon catheter). The authors report that penile angioplasty can be done safely with intraprocedural angiographic relief of vascular narrowing. These patients experienced a modest improvement in the IIEF-5 score post-procedure, and at six months after the procedure.
While this study is provocative, fundamental questions in this new field of investigation still need to be answered:
1) What is the aetiology of ED in the patient population being studied?
2) If the aetiology is likely to be vascular arterial insufficiency, how is the impaired arterial flow quantified? Are the documented vascular stenoses sufficient to cause a clinically significant decrement in flow?
3) After intervention, is there improvement in vascular flow that can be quantified, and does this correlate with clinical improvement?
ED is a complex, multifactorial psycho-physical condition. For interventionalists, it is tempting to look at an angiographic stenosis in an erectile-related artery in a patient with ED and attribute a cause-effect relationship. Unfortunately, the authors have not provided any objective measure of cavernosal arterial flow since penile duplex was not used to assess arterial insufficiency. While subject to its own limitations, penile duplex is nonetheless a readily available diagnostic tool which can be used to evaluate the peak systolic flow in the cavernosal arteries during tumescence, the quality of the cavernosal arteries (for atherosclerotic narrowings), the cavernosal tissue (for fibrosis), and to exclude venous leak. Importantly, the authors did not exclude subjects who had venous leak from the corpora cavernosa. In the Zotarolimus-Eluting Peripheral Stent System for the Treatment of Erectile Dysfunction in Males with Suboptimal Response to PDE5 Inhibitors (ZEN) trial, after screening by penile duplex, 15% of subjects were excluded because of venous leak, and an additional 15% were excluded because they had normal arterial inflow2. These types of patients would not be expected to improve with penile angioplasty. Distal stenoses were also seen in the ZEN trial and these patients were excluded from enrolment since the blockages were too small for stent therapy (Figure 1). It is certainly possible, however, that such patients might have derived benefit from small vessel angioplasty.
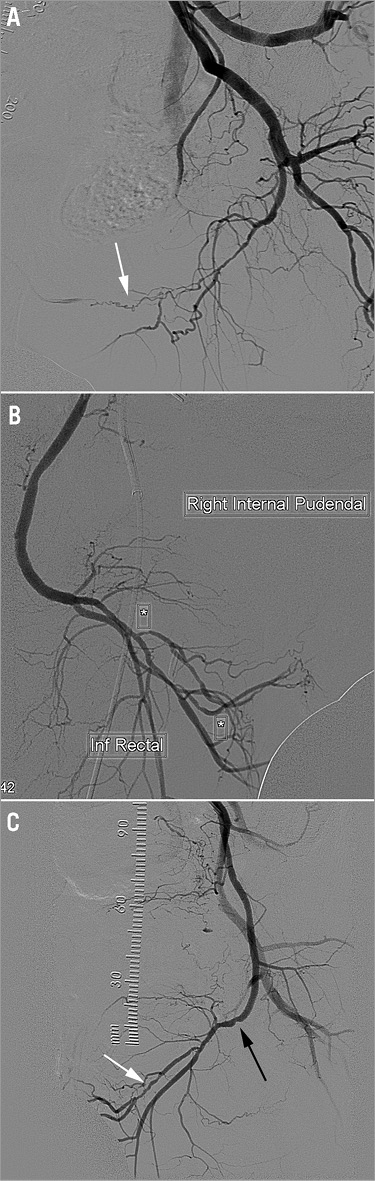
Figure 1. Examples of angiographic distal disease seen in patients from the ZEN trial, all of whom had penile Doppler evidence of arterial insufficiency. These patients were excluded from enrolment in the ZEN trial. A) Left distal common penile chronic total occlusion with bridging antegrade collaterals (arrow). There is also diffuse severe disease in the distal internal pudendal artery. B) Dual right common penile arteries (asterisks), both with severe proximal disease. C) Combined distal left internal pudendal (black arrow) and left common penile (white arrow) disease.
An exciting aspect of the PERFECT-1 trial was the use of CTA to identify the vascular anatomy and stenoses in the pelvic vasculature. The advantage of CTA to resolve the complex 3D architecture of erectile-related arteries is a topic of great importance to investigators making progress in this new field3,4. In terms of patient selection, it is notable that, of 120 patients screened by CTA, only 20 (15%) were deemed to be acceptable candidates for the distal intervention described in this study. In the ZEN trial, only 8% of screened subjects were treated. It is encouraging to speculate that, with a combined internal pudendal and common penile revascularisation approach, perhaps over 20% of subjects may now be candidates for erectile-related artery intervention.
Very small balloon angioplasty was performed on subjects with stenoses of the common penile artery in the current study with good immediate angiographic results. Since there is no imaging follow-up reported in this study, it is not possible to comment on the short or long-term durability of angioplasty for these small vessels. Given the high six-month angiographic binary restenosis rate with drug-eluting stents (34%) in the ZEN trial, it is hard to imagine favourable long-term patency with 1.5 mm balloon angioplasty.
Finally, it should be noted that the response to intervention as measured by IIEF-5 was modest, and could be explained by the placebo effect. Eighty-five percent of subjects at six months still had an IIEF score <22, which continues to meet the definition for some degree of ED. Longer-term clinical follow-up will be required. Without any objective assessment of penile arterial inflow or imaging follow-up, it is not possible to describe what physiologic effect was achieved by performing angioplasty.
Given the excitement to find an interventional solution for such a common clinical condition as ED, carefully controlled studies are required. Ultimately, randomised data will be necessary to prove the efficacy of erectile-related artery intervention. Currently, a single-centre randomised trial of vascular intervention for ED as compared to medical therapy is underway in Singapore. ED is a complex condition that can arise from dysfunction “between the legs, between the couple, and between the ears”. The number of variables that can affect a man’s perception of his erectile function is difficult to control for in any small study. New interventional procedures can generate initial enthusiasm that is undermined by subsequent negative results in randomised clinical trials such as we have seen for patent foramen ovale closure in cryptogenic stroke and renal denervation for resistant hypertension. We should interpret the current report cautiously and seek to produce ED data that will hold up under scrutiny – and this may prove to be more difficult than you might think.
Conflict of interest statement
The author has no conflicts of interest to declare.

