The path of progress in cardiology is strewn with the corpses of promising but unfulfilled ideas. Interventional cardiology, perhaps more than any other procedural specialty, has a record of rigorous evaluation of new devices, techniques, and medications that were initially thought “self-evidently” beneficial. Progress is Darwinian, with only the fittest concepts surviving the cauldron of rigorous, randomised trials. In contrast, adoption of some genuinely good ideas has been slow because trials were either not done, or were poorly designed.
ST-elevation myocardial infarction (STEMI) is most commonly caused by thrombus on a ruptured or fissured atheromatous plaque. Rapid restoration of TIMI 3 coronary flow preserves left ventricular function. Because distal thrombo- and athero-embolism is associated with adverse outcomes, it seemed obvious that prevention of coronary embolism would be a good thing. When the single-centre, 1,000-patient TAPAS trial1 reported substantial clinical benefit from routine thrombectomy during primary percutaneous coronary intervention (PCI), the interventional community rapidly adopted thrombus aspiration. However, two subsequent larger trials, TASTE2 and TOTAL3, enrolling over 7,000 and 10,000 patients, respectively, found no benefit with routine thrombectomy. Moreover, thrombectomy was associated with a concerning excess risk of stroke, most likely due to systemic embolism of some of the aspirated material. While these trials do not exclude a role for thrombus aspiration in carefully selected patients, there is no place for routine thrombectomy during primary PCI. In retrospect, the initial enthusiasm might have been tempered by earlier trials demonstrating that, when used in patients with STEMI, distal vascular protection devices caught embolic material but also did not provide a clinical benefit4.
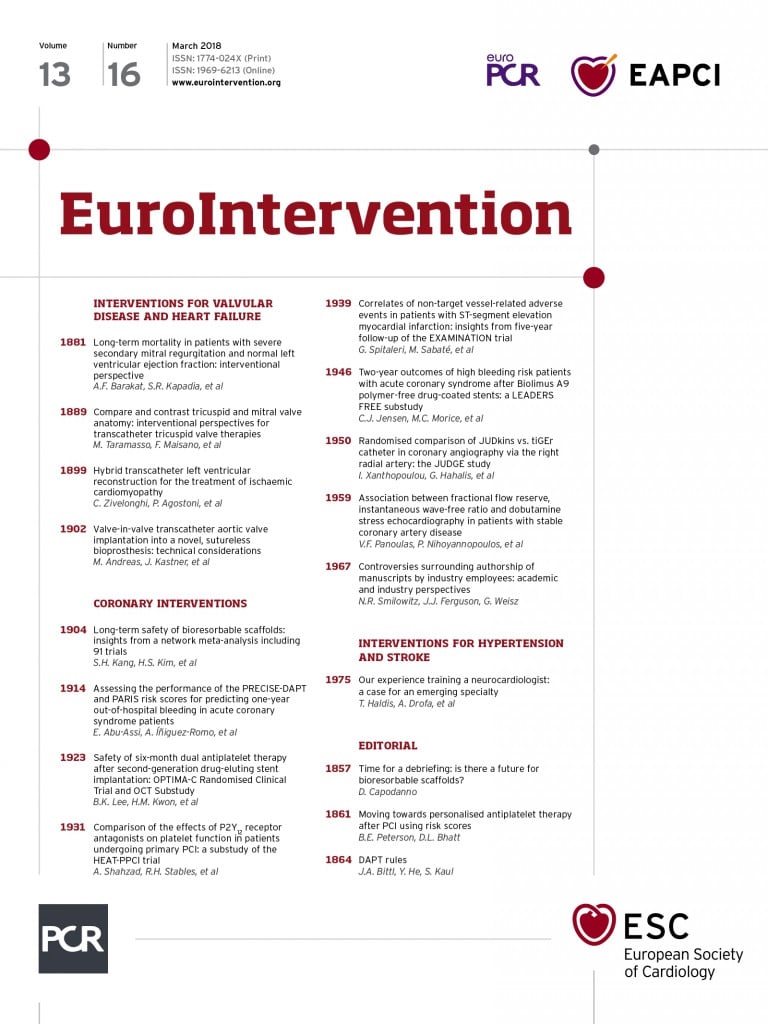
Another idea with strong conceptual appeal is that of bioresorbable scaffolds. These disappear when no longer needed and offer the potential for improved vasomotion, non-invasive imaging, and reduced late thrombosis and neoatherosclerosis at the treated site. After showing initial promise5,6, the first-generation Absorb™ polymeric everolimus-eluting scaffold (Abbott Vascular, Santa Clara, CA, USA) was associated with increased thrombosis at all evaluated time points, compared with current-generation drug-eluting stents7-9. Early stent thrombosis was likely associated with struts that are square, thick, wide and increased in number. This is so particularly if the scaffold is not fully expanded, not opposed to or embedded in the vessel wall, and deployed in small diameter vessels. Late thrombosis, at least in part, may be related to scaffold absorption taking longer than initially thought. The field is now in limbo. Although late advantages may accrue once the scaffold is completely absorbed, the earlier thrombotic cost may be too high. It is uncertain whether newer scaffolds with improved strut geometry, perhaps made of different materials, and with a shorter resorption time will overcome those limitations and provide a meaningful late benefit.
Sometimes the interventional community is slow to adopt proven advances in practice. Radial access coronary angiography was first reported by Campeau in 198910, and transradial PCI by Kiemeneij in 199211. Registry data demonstrating multiple benefits - reduced access-site bleeding, earlier patient ambulation and discharge, improved patient satisfaction, lower procedural cost and reduced morbidity – were confirmed by randomised trial data. In the RIVAL trial, those with STEMI undergoing primary PCI had a lower mortality with radial compared with femoral access, and a meta-analysis of all the randomised trials indicates that the mortality benefit applies beyond those with STEMI12,13. Despite the compelling evidence, radial access rates vary markedly from hospital to hospital and country to country. In New Zealand, 87% of all coronary procedures are radial, whereas in the USA the rate is only 23%14. Reasons for persisting with femoral access include the learning curve and a misconception that procedures such as bifurcation lesion PCI, rotational atherectomy, and chronic total occlusion intervention require larger calibre guide catheters than can be used radially14.
Some promising new technologies are hampered by less than compelling early trial data. Reasons for this include the design limitations of early-generation devices, limited clinical experience with the devices before study participation, and problems with study design. In particular, there may be problems with selecting the optimal study population (inclusion and exclusion criteria) and comparator group. The first randomised trial of left atrial appendage closure was the PROTECT AF trial, undertaken between 2005 and 2008, evaluating the WATCHMAN® device (Boston Scientific, Marlborough, MA, USA)15. It was designed as an equivalence study with warfarin in patients at increased stroke risk but who were able to be anticoagulated with warfarin. Because the safety endpoint (procedure-related device events and major bleeding) was higher in the WATCHMAN group, the FDA required another trial (PREVAIL)16; final device approval was not forthcoming until 2015. With the benefit of hindsight, the first randomised trial of left atrial appendage closure perhaps should have been in patients at high stroke risk and high bleeding risk, who were unable to take anticoagulants. Such a trial (ASAP-TOO) is only now being undertaken17.
Similarly, the association between a patent foramen ovale and stroke in younger patients was demonstrated in 198818,19, yet trial data showing clearly that closure was beneficial have only recently been published20-22. Although part of the delay related to the development of safe, easy-to-deploy closure devices, another important factor was that some earlier trial populations included patients in whom paradoxical embolism was probably not the mechanism of stroke.
An example of how to do things well is the introduction of transcatheter aortic valve implantation (TAVI). Surgical aortic valve replacement (AVR) for severe, symptomatic aortic stenosis, introduced in the 1960s23, has a Class I recommendation despite not being evaluated in a randomised trial in the 50 years since its introduction. The first two randomised trials in the PARTNER programme, evaluating a balloon-expandable TAVI valve (Edwards Lifesciences, Irvine, CA, USA), were undertaken concurrently in patient cohorts at very high surgical risk. Those deemed inoperable were randomised to TAVI or medical therapy24, whereas those considered surgical candidates were randomised to TAVI or surgical AVR25. A novel feature was the close collaboration between highly experienced cardiologists and cardiothoracic surgeons in both the study design and patient assessment for study participation, leading to the Heart Team approach widely employed in clinical practice today. Despite the limitations of the first-generation valve, including a 24 Fr delivery system, and the very limited experience of US TAVI operators at that time, those two trials established TAVI as a viable alternative to surgical AVR. The subsequent trial programme of both the Edwards valves26 and the self-expanding Medtronic CoreValve® (Medtronic, Minneapolis, MN, USA)27,28, extending into patient populations at progressively lower surgical risk, has evolved in concert with improved valve technology and increased operator experience, leading to TAVI consistently matching or bettering surgical AVR. Although there are some unresolved issues – long-term valve durability, bicuspid native valves, increased need for pacemakers, cost of the valve – TAVI has progressively replaced surgical AVR as the treatment of choice for most patients with aortic stenosis.
The pathway to acceptance or otherwise of a new interventional device or technique varies markedly for many reasons, including the effectiveness of the device and the quality of its assessment. Widespread clinical use should depend upon well-designed, appropriately sized, randomised trials undertaken at the right time in the development of the technology and in the right study population. If these are done well, what seems like a good idea at the time, often is.
Conflict of interest statement
J. Ormiston is a member of the Boston Scientific Advisory Board. M. Webster has no conflicts of interest to declare.