William Harvey published his seminal work in 1628, in book form, entitled “Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus” (Latin for “An anatomical exercise on the motion of the heart and blood in living beings”)1. Nearly a hundred years later, in 1711, Stephen Hales performed right and left heart catheterisation on a horse. Almost 250 years after that, in 1958, Mason Sones inadvertently injected contrast into a right coronary artery whilst performing cardiac catheterisation and interventional cardiology was born2. This translational route took 300 years, is still in development and likely to be so for as long as humans have coronary arteries. The way this development is evolving, not only longitudinally, but also widening in its breadth has been captivating. Interventional cardiology no longer relies just on understanding the anatomy and physiology of circulation, but also on understanding the many components of human biology that contribute to vascular health and disease. Thus, linking inflammation and genomics to the physiology of the circulation, molecular pathology of atherosclerosis and development of new technologies are at the centre of this rapidly evolving field3. What has become quite clear is that the gap between the many “basic science” disciplines involved and clinical application is narrowing both significantly and rapidly.
Early scientific research that may be aimed at translation often takes many years to evolve, with endless problem solving that often requires the researchers to adapt and sometimes start afresh when an idea fails. However, it is in the interest of the wider research community, as well as the clinical community, to support these early stage endeavours and engage with them at an embryonic stage.
As the world changes, and globalisation takes medical research to astronomical heights, the need for “translational medicine” has become a de facto one. This field brings those working in basic research closer to those undertaking clinical research and the general community of clinicians. It encompasses a broad spectrum of research foci. The main categories of translational research are those that encompass early-stage work from basic discoveries of new molecules, animal models and new devices all the way through to first-in-man, phase 1 and phase 2 studies. This is referred to as T1 translational research. The second part of translational medicine (T2) involves the implementation of clinical trial results in clinical practice. The third aspect, termed (T3), is research that promotes a dynamic interaction between laboratory-based science and population-based research in both directions. T3 is very interesting for us as interventionists, as it encourages a two-way stream between observations obtained either in the catheter laboratory or from clinical interventional studies, back to the science laboratory and vice versa4.
Furthermore, the all-encompassing umbrella of translational medicine, with all its challenges, requires the collaboration of many disciplines and a shared vision. Often, research is a collaboration among basic scientists, clinicians, engineers and industry partners. The need for partnership from non-commercial grant-funding bodies as well as industry is crucial5,6.
Within interventional cardiology, there is now a virtual explosion of novel and exciting ideas, with much early work that needs to be cultivated and critically appraised. The field is rich with device development, new molecules, and new concepts that are yet to be explored at a therapeutic level. Yet it seems that the “jobbing” cardiologist is pretty much deprived from taking a “peek” at this work in the mainstream cardiology journals. It is well recognised that discussion and interaction among basic scientists, bioengineers, translational cardiologists and the interventional community at large hardly ever seem to take place in a unified environment.
A significant obstacle for those undertaking translational work, in a research world that is rightly or wrongly judged by standardised units such as impact factor, is that their work may be overlooked by those journals only seeking high-impact publications. The difficulty in publishing translational work has historically been due to the conundrum of it not falling within “a basic science remit” or a “clinical trial remit”. Therefore, work that explores novel targets, models, and devices in early animal studies that lacks detailed mechanistic data tends to be excluded from high-impact basic science journals. Similarly, first-in-man studies or phase 1 and 2 studies can be largely ignored by mainstream clinical journals7.
Grant-funding bodies, such as the UK-based Wellcome Trust and the British Heart Foundation, now encourage translational research and offer dedicated funding as well as training streams for it. However, besides the need for funding and institutional support for translational interventional cardiology, there is a real need for a forum where the work is exposed to the general community and given due attention. Recently, general cardiology journals have identified the gap and there have been some efforts to develop new publications that expose translational work8 and alter the focus from impact factor to translational impact7.
EuroIntervention has traditionally published both experimental and preclinical papers in the past and continues to do so (Figure 1). In order to structure the future in line with the international push to focus on translational medicine, I (RK) have accepted the honourable invitation to take up the position of Translational Research Editor for the Journal. We will aim to welcome translational work that is judged by the editors to have a reasonable “translational impact”. We will not be shy in taking some risk on some of the work, to allow it an opportunity to flourish and be given adequate attention by the wider community at an early stage. We hope that the input and interaction from our audience will ease the route to clinical implementation of important ideas that have undergone rigorous study in translational models and early human studies.
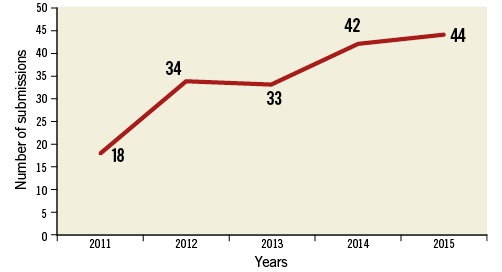
Figure 1. Preclinical/experimental research submissions in EuroIntervention.
In this issue of EuroIntervention, Schmitt et al present their pioneering translational interventional work testing a stent-mounted, fully tissue-engineered heart valve in an ovine model9. These valves are grown in the laboratory (this word can foster misunderstanding between scientists and clinicians – I refer here to the “science laboratory” rather than the “catheter laboratory”!), and are made from ovine vascular-derived cells. The valves are decellularised to reduce any immunogenic reactions when implanted, and sterilised prior to implantation via the transcatheter route in the pulmonary position. The bioengineering novelty is in complete endothelialisation and remodelling of the valvular matrix, with the valve being quickly populated by the recipient’s autologous cells. Although the results show worsening regurgitation over time, probably due to technical tissue engineering issues and adaptation to the ovality of the valve when implanted, the authors eloquently describe these challenges and offer explanations. Clearly, the current version of this valve is still in need of significant development prior to first-in-man study, but the research is innovative and has been long awaited by the structural interventional community. Therefore, there is a real prospect that this approach will have a long-standing impact on the future of transcatheter valve interventions. We really hope that you will be pleased to see this innovation featured in this issue of EuroIntervention.
Conflict of interest statement
The authors have no conflicts of interest to declare.