This article in the EuroIntervention Tools & Techniques series provides the “How-to-do” aortoiliac and common femoral endovascular interventions. The complete, unabridged e-version with dynamic images can be viewed at www.eurointervention.org. The following is a summary and highlights the key approach that underpins a safe practice and the way to obtain good results.
The infrarenal abdominal aorta and iliac arteries are among the most common sites of chronic obliterative atherosclerosis, accounting for about one-third of all symptomatic peripheral artery disease (PAD) cases. The percutaneous approach has become the treatment of choice for the majority of patients presenting with atherosclerotic aortoiliac disease. The TransAtlantic Inter-Society Consensus (TASC) working group published in the year 2007 an update of the management of PAD, including classification and interventional guidelines of aortoiliac disease (Figure 1).
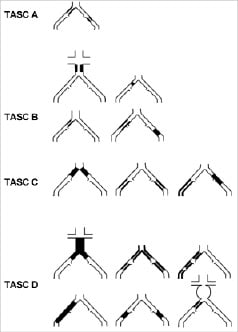
Figure 1. TransAtlantic Inter-Society Consensus (TASC II) morphologic stratification of iliac lesions.
Currently, percutaneous transluminal angioplasty (PTA) ±stenting has become the treatment of choice for short abdominal aortic stenosis in the absence of significant iliac disease, while surgery should be proposed for distal aortic occlusion (i.e., Leriche syndrome). Access is usually gained using the single retrograde common femoral artery (CFA) approach. On occasion a bilateral retrograde CFA access may be used if balloon dilatation or stent expansion is performed with a double balloon technique or a further brachial access may be necessary to recanalise complex aortic occlusions (Figure 2).
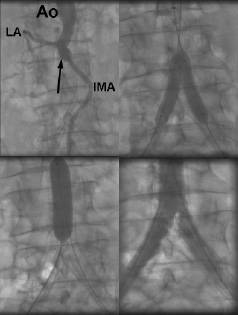
Figure 2. Complete occlusion of the distal abdominal aorta (Leriche Syndrome: arrow) with abundant collateralisation via the inferior mesenteric artery (IMA) and the lumbar artery (LA) (upper panel left). After successful antegrade recanalisation (brachial access), implantation of two large self-expanding stents at the common iliac artery (CIA) level and kissing balloon dilatation (one brachial, the other femoral access) (upper panel right). Final stent implantation at the distal aorta level with final balloon inflation at that level (lower panel left). Final angiographic results show very good results at the distal aorta and the right CIA ostium, and 30% residual stenosis at the left CIA ostium (lower panel right). Ao: abdominal aorta.
Ostial lesions of the common iliac artery are best approached using an ipsilateral retrograde CFA access because an optimal stent placement using the crossover approach may result challenging. Reconstruction of the aortic bifurcation is usually performed with kissing angioplasty/stenting. Simultaneous balloon/stent inflation at the level of the aortic bifurcation is aimed to prevent plaque shift in patients with severe bilateral ostial iliac disease (Figure 3).
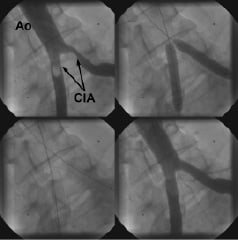
Figure 3. Significant stenosis of the ostia of both common iliac arteries (CIA) (upper panel left: arrows). Simultaneous kissing stenting of both common iliac artery ostia (upper panel right), in order to minimise the risk of significant plaque shifting. The stent struts are not protruding in the distal aorta, thus allowing future crossover manoeuvres (lower panel left: arrow). Final angiographic result (lower panel right). Ao: abdominal aorta.
In the presence of a stenosis located in the distal portion of the external iliac artery or the proximal segment of the CFA, the retrograde approach should not be used due to the immediate proximity between the access site and the lesion. Therefore, access should be gained using a crossover technique. For lesions of the CFA, surgery should be considered the therapy of choice, as it may be performed with local anaesthesia, may yield good results, and does not jeopardise future access. If a percutaneous intervention is performed, the contralateral approach is mandatory and a debulking strategy with atherectomy devices may be preferred in order to minimise the need of stent placement and to reduce any potential plaque shift into the profunda femoral artery.
Stenting is recommended for the treatment of iliac long or ostial lesions, total occlusions, and for suboptimal PTA results. Alternatively, stenting is regarded as default strategy by many investigators. Regarding stent type, the high radial strength of balloon-expandable stents and the lack of foreshortening make them suitable in particular for ostial or severely calcified iliac lesions. The greater flexibility and conformability of self-expanding stents apply well to long lesions in tortuous segments. With respect to CFA interventions, stenting should be avoided whenever possible, in order to prevent crushing and to preserve future vascular access.

