Abstract
Aims: Patients with renal artery stenosis are treated with percutaneous intervention, but randomised studies are inconclusive. We aimed to compare renal percutaneous revascularisation versus medical therapy.
Methods and results: A systematic search for randomised controlled studies yielded three studies comparing renal angioplasty and two studies comparing renal angioplasty with stenting versus medical therapy, respectively. Six sets of data were extracted focusing on systolic and diastolic blood pressure as well as serum creatinine at follow-up. The five trials included 1,030 patients with renal artery stenosis. There was a trend toward, but no significant improvement in, systolic blood pressure (weighted mean difference [WMD] –2.76 mmHg, 95% confidence interval (CI) –5.71 to 0.18; p=0.07), diastolic blood pressure, (WMD –1.18 mmHg, 95% CI –2.69 to 0.32; p=0.12), or serum creatinine (WMD –7.26 mmol/L, 95% CI –14.99 to 0.47; p=0.07) in the patients who underwent percutaneous intervention compared to the medical therapy group. All but one trial showed at least a moderate overall bias risk.
Conclusions: We did not find a significant improvement in blood pressure or renal function in patients with renal artery stenosis treated with renal artery revascularisation compared to medical therapy alone. However, trial quality was a limitation.
Introduction
Renal artery stenosis (RAS) is the most common secondary cause of hypertension and affects 1-5% of hypertensive patients, but the true prevalence of RAS is not known1. In autopsy studies, the prevalence of RAS ranges from 26 to 62%2,3. The prevalence of RAS among patients older than 65 years of age has been shown to be 6.8%4. It has been estimated that there are 2-4 million people with RAS in the United States alone5.
Clinically, patients with RAS typically present with hypertension, renal insufficiency, or both. Renovascular hypertension results from hypoperfusion of one or both kidneys, which stimulates the renin-angiotensin system resulting in vasoconstriction, and salt and water retention. Intravascular fluid shifts can have significant clinical consequences for patients with congestive heart failure and/or coronary artery disease. RAS can be associated with episodic decompensations of heart failure, “flash” or sudden onset of pulmonary oedema, or unstable or refractory angina6. Hypoperfusion from RAS can also result in ischaemic injury to the renal parenchyma. It has been estimated that at least 10-15% of patients entering dialysis programs have RAS as a primary cause of renal failure although it is unclear based on current data what percentage of these patients have bilateral RAS, unilateral RAS, or RAS of a solitary functioning kidney7.
Over 40,000 percutaneous renal artery interventions are performed in the United States on a yearly basis5. The most common indications for these procedures include refractory hypertension, preservation of renal function and cardiac destabilisation syndromes, including congestive heart failure and unstable angina. Several randomised control trials have looked at the benefits of percutaneous renal artery interventions and medical therapy versus medical therapy alone, and have provided conflicting results. We conducted a systematic review and meta-analysis of randomised trials comparing percutaneous renal artery intervention (PTRI) (renal artery angioplasty with or without stenting) versus medical therapy.
Methods
A systematic search for randomised trials of revascularisation in atherosclerotic renal artery stensosis (ARAS) was undertaken searching PubMed, CENTRAL, mRCT, BioMed Central, CardioSource, ClinicalTrials.gov, and ISI Web of Science using a highly sensitive and specific strategy as previously described8. Search keywords included “random”, “control”, “trial”, “atherosclerotic”, “renal”, “revascularisation”, “angioplasty” and “stent”. The search was extended to June 2009. No language restriction was used. In addition, major journals in the field were hand searched for relevant material. The hand search also involved a search of conference proceedings to identify presentations made at international cardiology, vascular medicine and radiology meetings. Experts in the field were contacted in an attempt to identify studies not found by the electronic and hand searches, in order to identify trials that have not been formally published. Information was also sought from reviewing reference lists of already retrieved papers, including review papers and previous meta-analyses of renal artery revascularisation.
Study selection
Inclusion in the analysis required that the treatment group underwent PTRI with percutaneous balloon angioplasty and/or endovascular stenting in addition to medical treatment, that the control group received medical therapy alone, and that the group assignments were randomly allocated.
Outcome measures and statistics
The main outcome measures were systolic blood pressure (SBP), diastolic blood pressure (DBP) and serum creatinine (SCr) at follow-up. The mean and standard deviations for each outcome measure were extracted from published papers9. Standard methods for meta-analyses of study level data were employed10. Specifically, we tested the hypothesis of statistical homogeneity by means of the Q-statistic and χ2 test, and measured the extent of statistical consistency by computing the I-square index. Small study effects (e.g., publication bias) was assessed for the main endpoints by visual examination for funnel plots and the Egger method11. Mean differences in SBP, DBP, and SCr at follow-up from the individual studies were pooled with fixed-effect methods by means of weighted mean difference (WMD) and corresponding 95% confidence intervals. Statistical significance was set at the 0.05 and 0.10 2-tailed levels for, respectively, statistical effect and statistical homogeneity. Computations were performed with Review Manager (RevMan) 4.2 (The Cochrane Collaboration, Oxford, United Kingdom). Analysis was based on the intention-to-treat data from the primary trials, when available.
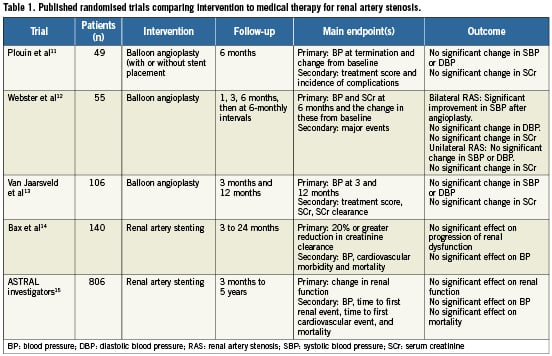
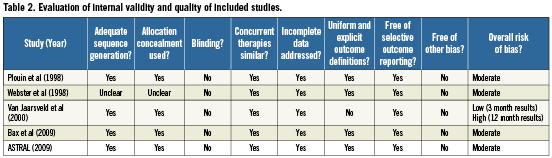
Table 1 outlines for each study, the number and type of patients included in the trial, the randomised treatment comparison, the endpoints, and the duration of follow-up. All the trials reported endpoints of SBP, DBP, and SCr. Our analysis includes comparisons of BP and SCr at follow-up between treatment and control groups. Plouin et al did not report SCr at follow-up in their original manuscript but this data has been reported separately12. Comparisons of BP and SCr to baseline were not possible due to lack of reporting of these values in the original manuscripts. Table 2 addresses the risk of bias in the results of the included studies and a summary score of low, moderate or high risk of bias was given according to the criteria indicated by the Cochrane Collaboration Handbook13.
Results
Five randomised controlled trials comparing PTRI plus medical therapy and medical therapy alone in patients with ARAS were identified. In the study by Plouin et al, 49 patients with hypertension and unilateral ARAS were randomised with 26 allocated to the medical therapy group and 23 allocated to the PTRI group14. Of the 23 patients in the PTRI group, 21 underwent renal artery angioplasty and two underwent renal artery angioplasty and stent placement. With regard to renal artery lesion severity, 65% of the patients in the PTRI group had renal artery lesions between 60 and 74%. The study by Webster et al enrolled patients with hypertension and was stratified according to whether the patient had unilateral or bilateral ARAS. These patients were analysed separately, resulting in two sets of data (28 patients with bilateral ARAS and 27 patients with unilateral ARAS15). Of the 28 patients with bilateral ARAS, 12 were randomised to the PTRI group with 10 undergoing percutaneous renal artery angioplasty. Of the 27 patients with unilateral ARAS, 13 were randomised to the PTRI group with 10 undergoing renal artery angioplasty. The only assessment of severity of the renal artery lesions of the patients enrolled in this study was that the lesions were >50%. In the study by van Jaarsveld et al, 106 patients with hypertension and unilateral or bilateral ARAS were randomised; 56 patients (23% with bilateral ARAS) in the renal artery angioplasty group and 50 patients (30% with bilateral ARAS) in the medical therapy group16. Of the 56 patients randomised to the PTRI group, 54 underwent renal artery angioplasty and two underwent renal artery stenting and, in terms of severity of ARAS, 21% had lesions between 50% and 69%. In the study by Bax et al, 140 patients with abnormal renal function were randomised, and 64 (46%) were allocated to the PTRI group17. Eighteen patients (28%) allocated to the PTRI group did not receive percutaneous renal artery stenting. Of those 18 patients, 12 patients were found to have ARAS <50%. In the study from the ASTRAL investigators, 806 patients were randomised and 403 (50%) were allocated to the PTRI group18. Of these 403 patients, 317 (79%) underwent percutaneous renal artery stenting. Eighty-six patients (21%) were not percutaneously revascularised after randomisation. Thirty-three patients (8%) were reported to have minimal stenoses.
Six sets of results from five trials were included in this meta-analysis. The six sets of data included 1,030 patients with ARAS with the smallest data set including 27 patients (Webster - unilateral ARAS) and the largest data set including 680 patients (ASTRAL investigators). Although 806 patients were randomised in the ASTRAL trial, only data from 680 were available at 12 months and used for analysis. In total, the final analysis had 500 (48.4%) randomised to receive PTRI (angioplasty with or without stent placement) and 533 patients (51.6%) randomised to receive medical therapy alone. Follow-up data for the studies by Plouin et al and Webster et al were taken at six months. The study by van Jaarsveld et al had follow-up data from three and 12 months, but this trial was criticised because nearly half of the patients randomised to medical management underwent angioplasty between three and 12 months post-randomisation.
Consequently, in our analysis, the results for this trial are presented at three months, when there had been no crossovers from medical management to angioplasty. In the study by Bax et al, results at 24 months follow-up were used. In the study by the ASTRAL investigators, results were available up to five years after initial randomisation. In this case, our study used the results from 12 months because it provided the largest number of patients for analysis.
Comparisons between patients with ARAS who underwent PTRI versus those who received medical therapy alone were made for SBP, DBP, and SCr at follow-up intervals from three to 24 months, as noted above. SBP was decreased, but not significantly so in the group undergoing PTRI (WMD –2.76 mmHg [–5.71 to 0.18], p for effect=0.07, p for heterogeneity=0.84, I-square=0) (Figure 1), and DBP was also not significantly decreased (WMD –1.18 mmHg [–2.69 to 0.32], p for effect=0.12, p for heterogeneity=0.17, I-square=36%) (Figure 2). In addition, the SCr was lower, but not significantly so in patients who underwent PTRI compared to the medical therapy group (WMD –7.26 mmol/L [–14.99 to 0.47], p for effect=0.07, p for heterogeneity=0.38, I-square=6%) (Figure 3). The corresponding funnel plots for SBP, DBP, and SCr did not suggest that there was significant publication bias associated with these results (Figure 4). Accordingly, Egger regression tests showed non-significant results in all cases (all p>0.05), although the small number of studies makes it difficult to draw firm conclusions.
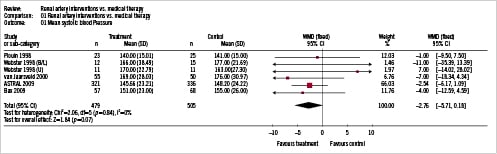
Figure 1. Systolic blood pressure at follow-up (Mean[SD]) with corresponding forest plot. B/L: bilateral; CI: confidence interval; Rx: treatment; SD: standard deviation; U: unilateral; WMD: weighted mean difference
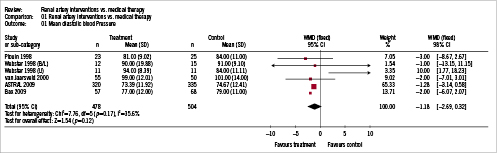
Figure 2. Diastolic blood pressure at follow-up (Mean[SD]) with corresponding forest plot. B/L: bilateral; CI: confidence interval; Rx: treatment; SD: standard deviation; U: unilateral; WMD: weighted mean difference

Figure 3. Serum creatinine at follow-up (Mean[SD]) with corresponding forest plot. B/L: bilateral; CI: confidence interval; Rx: treatment; SD: standard deviation; U: unilateral; WMD: weighted mean difference
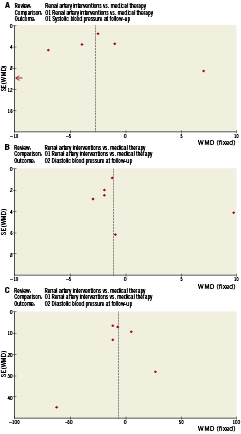
Figure 4. Begg funnel plots for: A) systolic blood pressure; B) diastolic blood pressure; C) serum creatinine. SE: standard error; WMD: weighted mean difference
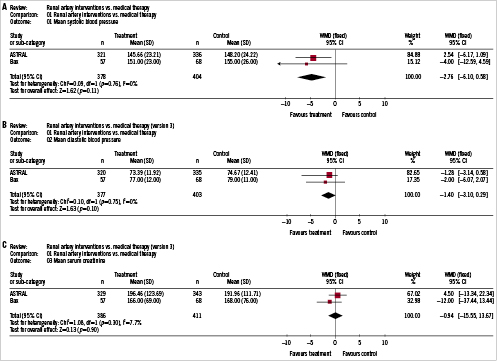
Figure 5. Meta-analysis and forest plots of stenting trials only. A) Systolic blood pressure; B) diastolic blood pressure; and C) serum creatinine. B/L: bilateral; CI: confidence interval; Rx: treatment; SD: standard deviation; U: unilateral; WMD: weighted mean difference
A subgroup meta-analysis of the two trials comparing renal artery stenting versus medical therapy (Figure 5) comprised fewer patients and did not materially change the results of our analysis at this time. Specifically, no significant differences were found in SBP (WMD –2.76 mmHg [–6.10 to 0.58], p for effect=0.11, p for heterogeneity=0.76, I-square=0), DBP (WMD –1.40 mmHg [–3.10 to 0.29], p for effect=0.10, p for heterogeneity=0.75, I-square=0), and SCr (WMD –0.94 mmol/L [–15.55 to 13.67], p for effect=0.90, p for heterogeneity=0.30, I-square=8%).
Discussion
This meta-analysis of 1,030 patients who received renal artery intervention and medical therapy for ARAS or medical therapy alone showed a trend toward, but no statistically significant benefit of, PTRI in combination with medical therapy on SBP, DBP, or SCr. Based on this data, the effect of renal revascularisation intervention in the populations studied is likely small and inconsistent.
Intuitively, these results do not make physiologic sense. Alleviation of significant renal artery lesions should decrease the substrate for renovascular hypertension and improve renal blood flow resulting in improved renal function or at least prevent deterioration of renal function.
Several considerations need to be taken into account before definitive conclusions are drawn from these results. All the trials included in this meta-analysis were subject to potential bias. The risk of bias, defined by the Cochrane Collaboration Handbook, was at least moderate for four out of the five studies included. The three-month results from the trial by van Jaarsveld et al were considered to have a low risk of bias whereas the 12-month results of this study were considered to have a high risk of bias due to the significant crossover of patients from the medical treatment group to the angioplasty group. One of the most important contributors to bias in these studies was the varying definitions of ARAS with some authors admitting that certain patients who were randomised did not have “significant” ARAS at the time of angiography. The majority of patients in these trials were screened with Doppler ultrasound, CT, and/or MRI to determine ARAS severity prior to randomisation. Unfortunately, ARAS severity as determined by these screening tests did not always correlate with subsequent angiography. In the two largest trials, 12% of patients randomised to the PTRI group had ARAS of <50%.
As a result, a considerable selection bias may have occurred while enrolling patients into the randomised control trials calling into question what percentage of these patients actually had haemodynamically significant ARAS. Schwarzwalder et al point out that the reason for this selection bias occurs is that the patients with potentially the highest benefit from PTRI are frequently not enrolled in these randomised control trials for fear of harm to the patient by committing them to a conservative treatment arm19. This has resulted in a heterogeneous population of patients with questionably significant ARAS in whom generalisation about the population as a whole is difficult at best.
The size of the studies is also an important consideration and the fact that only one trial had more than 100 patients in each arm is a serious limitation of the available data. This is further compounded by the fact that the total number of patients is about 1,000, which limits the power of detecting smaller effects. Moreover, 95 (19%) patients who underwent PTRI in our analysis had angioplasty alone. It is generally accepted that for ARAS, renal artery stenting is the standard of care for PTRI with higher procedural success rates and lower restenosis rates. As a result, having a significant percentage of patients who underwent only renal angioplasty may have altered the results of the analysis.
Furthermore, the studies included did not all have the same primary endpoint, and there is the question of whether or not randomised trials thus far have looked at the appropriate study endpoints. SBP, DBP, and SCr were used in this meta-analysis because they were the only variables that were consistently measured in all the individual studies. Schwarzwalder et al argue that what the randomised trials so far have shown us is that blood pressure can possibly be controlled almost as well with medical therapy as with PTRI, but they have not given us insight into the most important endpoint, which is patient survival19. The ASTRAL trialists attempted to investigate this and showed no improvement in survival with PTRI, but limitations imposed on patient selection in this study likely affected the results.
More recent studies have supported the idea that identifying patients who have clearly documented haemodynamically significant ARAS or high risk clinical features such as renal dysfunction and/or myocardial dysfunction may be more likely to benefit from PTRI. Leesar et al showed that a hyperaemic systolic gradient, as measured by a pressure guidewire after a 30 mg bolus dose of papaverine of >21 mmHg, identified haemodynamically significant ARAS and predicted sustained improvement in blood pressure at 12 months20. Also of note, the majority of patients in the study by Bax et al and ASTRAL had normal or near-normal renal function as measured by SCr, which likely makes it difficult to show any benefit from revascularisation on renal function. Kalra et al looked at patients with ARAS with stage four and stage five chronic kidney disease and found that PTRI improved renal function and was associated with increased survival21.
These more recent studies lend support to the argument that patient selection has been the major shortcoming of the randomised control trials so far19,22,23, and that broad conclusions regarding PTRI cannot be made at this time. The next challenge is to design studies to examine PTRI in patients with haemodynamically significant ARAS looking at clinical endpoints. Upcoming prospective studies such as CORAL24, NITER25, RAVE26 and RADAR27 will hopefully help us refine our approach and identify those patients who benefit most from PTRI and provide a larger data set that would allow a meta-analysis of renal artery stenting versus medical therapy in patients with renal artery stenosis.
Conclusion
The patient diagnosed with ARAS should first undergo aggressive medical therapy for hypertension. The question whether to also treat with PTRI remains. Based on the data so far available, it appears that patients who have bilateral ARAS or ARAS of a solitary functioning kidney benefit most from PTRI. In unselected patients with unilateral ARAS, the effects of revascularisation in addition to optimal medical therapy are probably small and have not been proven by our meta-analysis. However, because of the limitations of the studies published up to this point, the data needs to be interpreted with caution.
Conflict of interest statement
The authors have no conflict of interest to declare.

