Abstract
Aims: Our aim was to evaluate the safety and efficacy of intracoronary (IC) nicorandil as an alternative choice of hyperaemic agent for invasive physiologic studies.
Methods and results: A total of 480 intermediate coronary lesions from 429 patients enrolled from six Japanese and Korean centres were analysed. IC nicorandil showed earlier achievement of hyperaemia (time to the lowest FFR: 18.0 s [1st and 3rd quartile value 15.6-21.5] vs. 44.0 s [36.0-60.0], p<0.001) with similar hyperaemic efficacy, compared with intravenous (IV) adenosine/ATP (FFR 0.82 [0.75-0.87] vs. 0.82 [0.74-0.88], p=0.207). FFR measurements with both agents showed excellent correlation and classification agreement (CA) for FFR ≤0.80 (r=0.941, ICC 0.980, CA 90.8%, kappa=0.814, AUC of nicorandil 0.980, all p<0.001). Only three patients (0.7%) showed changes in classification across the grey zone (0.75-0.80). IC nicorandil produced fewer changes in blood pressure (BP) and heart rate (HR) and showed less chest pain than IV adenosine/ATP (all p<0.001). When comparing ΔFFR according to ΔBP or ΔHR between IV adenosine/ATP and IC nicorandil, there were no correlations, either between ΔFFR and ΔBP (r=-0.114, p=0.091), or between ΔFFR and ΔHR (r=1.000, p=0.151).
Conclusions: Nicorandil IC bolus injection is a simple, safe and effective hyperaemic method for FFR measurement and can be used as a substitute for adenosine.
Abbreviations
ATP: adenosine triphosphate
AV: atrioventricular
AUC: area under the curve
BP: blood pressure
CA: classification agreement
FFR: fractional flow reserve
GEE: generalised estimating equation
HR: heart rate
IC: intracoronary
ICC: intraclass correlation coefficient
IV: intravenous
LAD: left anterior descending
Pa: aortic pressure
Pd: distal coronary artery pressure
VAS: visual analogue scale
Introduction
Fractional flow reserve (FFR) has become a standard invasive assessment for determining the functional significance of coronary artery stenosis. FFR-guided percutaneous coronary intervention (PCI) has been shown to improve clinical outcomes over medical treatment or an angiography-guided intervention strategy in patients with coronary artery disease. FFR is defined by the ratio of maximal hyperaemic flow in the presence of coronary artery disease to the maximum hyperaemic flow in the hypothetical case where the supplying vessels are normal. Clinically, FFR is measured by the ratio of distal coronary artery pressure (Pd) to aortic pressure (Pa) under conditions of pharmacologically induced hyperaemia. As Pd is determined by both epicardial stenosis and microvascular resistance, maximal hyperaemia is a critical prerequisite for the accurate measurement of FFR1,2. Intravenous (IV) infusion of adenosine through the central vein is the gold standard method for the induction of hyperaemia3. Alternative methods to achieve hyperaemia using different routes of administration or with hyperaemic agents targeting different receptors have also been evaluated and have shown promising results1,4.
Intracoronary (IC) bolus injection of nicorandil (Sigmart®; Chugai Pharmaceutical Co., Ltd., Tokyo, Japan), a coronary vasodilator which acts on both macrovascular and microvascular systems, has been reported to be safe and cardioprotective in patients with coronary artery disease1,4-7. In this study, we performed a patient-level pooled analysis of previous studies1,4-7, which compared FFR measurement using IV adenosine/adenosine triphosphate (ATP) and IC nicorandil, in order to compare comprehensively hyperaemic efficacy, haemodynamic changes, occurrence of chest pain and atrioventricular block, and variability of FFR, according to changes in blood pressure (BP) and heart rate (HR) with two different methods of hyperaemia induction.
Methods
STUDY POPULATION
The study population comprised a pooled cohort of five previous studies which compared FFR measurement between IV adenosine/ATP and IC nicorandil (Appendix Figure 1)1,4-7. A total of 480 lesions from 429 patients with coronary artery disease enrolled from six centres in Japan and Korea were included. Among the total number of patients, 44.9% were enrolled from Korea, and 55.1% of the pooled population were enrolled from Japan. In all lesions, pre-interventional FFR values were measured with hyperaemia, achieved by both conventional method (continuous IV infusion of adenosine 140 μg/kg/min1,4 or ATP 150 μg/kg/min5-7) and IC bolus injection of nicorandil 2 mg1,4-7.
From the total number of lesions, 210 lesions underwent repeated FFR measurement with IV adenosine infusion, and repeated measurement with IC nicorandil administration. In this subgroup, reproducibility and per-range diagnostic accuracy were analysed. In each participating centre, institutional review board approval and written informed consent were obtained as per current regulations. The study protocol was in accordance with the Declaration of Helsinki.
CORONARY PHYSIOLOGIC MEASUREMENTS, HAEMODYNAMIC DATA COLLECTION AND HYPERAEMIC AGENTS
Coronary angiography was performed using standard techniques. Angiographic views were obtained after the administration of IC nitrate (100 or 200 μg). All coronary physiologic measurements were obtained as previously described8. In brief, a 4-7 Fr guiding catheter without side holes was used to engage the coronary artery and a pressure-temperature sensor guidewire (St. Jude Medical, St. Paul, MN, USA) was used for FFR. The pressure sensor was positioned at the distal segment of the target vessel and IC nitrate (100 or 200 μg) was administered before each physiologic measurement. Hyperaemic proximal Pa and distal coronary artery pressure (Pd) were obtained during sustained hyperaemia, and FFR was calculated as mean Pd/Pa during hyperaemia. The time to the lowest FFR (time needed to reach >90% of the minimal value of Pd/Pa) and the plateau time (the time during which FFR remained at >90% of its lowest value) were measured1,5. The visual analogue scale (VAS) pain score was assessed during IV infusion of adenosine and IC bolus injection of nicorandil1. Each hyperaemic agent was administered after confirming that the Pa, Pd, and heart rate had recovered to baseline values. Haemodynamic parameters such as BP and HR were also recorded from baseline to maximal hyperaemia.
ASSESSMENT OF CLASSIFICATION AGREEMENT AND VARIABILITY OF FFR VALUES
In order to compare classification agreement between IV adenosine/ATP and IC nicorandil, an FFR value of ≤0.80 was used as a cut-off value to define the presence of myocardial ischaemia. Classification agreement was established when both FFR values were ≤0.80 or when both were >0.80. The difference of FFR values between two hyperaemic stimuli was evaluated according to the change in BP (ΔBP) or HR (ΔHR) to assess the FFR variability according to the haemodynamic changes and different hyperaemic stimuli.
In addition, a comparison of hyperaemic efficacy and classification agreement between IV adenosine/ATP and IC nicorandil was performed according to the different target interrogated vessels and in a subgroup of patients with diabetes mellitus who were treated with sulphonylurea.
STATISTICAL ANALYSIS
Categorical variables are presented as numbers and relative frequencies (percentages), and were compared using McNemar’s test. Continuous variables were presented as means and standard deviations or median with 1st and 3rd quartile values, and were compared with the paired samples t-test or Wilcoxon signed-rank test, according to their distribution. Unimodal distribution of FFR data measured by IV adenosine/ATP and IC nicorandil were confirmed by Hartigan’s dip test. Classification agreement of the two FFR values with different hyperaemic methods was evaluated by Cohen’s kappa coefficient and intraclass correlation coefficient (ICC). Linear regression analysis was used to estimate the correlation coefficient (Pearson or Spearman, according to the normality of the variables) between FFR measurements from two different hyperaemic methods. Per-range agreement (diagnostic accuracy) between two repeated measures of FFR was calculated in quantiles of mean FFR values, which was divided from 0.2 to 1.0, using a cut-off value of 0.80, as previously described4,9. The comparison of the mean difference of FFR values between IV adenosine/ATP and IC nicorandil among the three target vessels was performed with a generalised estimating equation (GEE) with pairwise comparisons to adjust for intra-subject variability among vessels from the same patient. Receiver operating curve analysis was used as an overall discriminant function of IC nicorandil to predict the ischaemic range of FFR values measured by IV adenosine/ATP infusion.
Results
BASELINE CHARACTERISTICS
Baseline clinical and lesion characteristics are summarised in Table 1. The mean age of the study population was 66.6±9.8 years, 71.1% were male, and 41.5% of patients had diabetes mellitus. Half of the patients presented with stable angina and 17.2% of patients underwent coronary angiography due to asymptomatic coronary artery disease diagnosed with coronary CT angiography or routine follow-up angiography. Among the 480 lesions, the majority of stenoses were located in the left anterior descending artery (LAD), and most of these lesions were of intermediate degree of stenosis (mean percent diameter stenosis 54.3±15.2%). Analysis of FFR values showed a unimodal distribution with a mean value of 0.80±0.11 for IV adenosine/ATP and 0.80±0.11 for IC nicorandil; 69.6% of IV adenosine/ATP FFR and 70.8% of IC nicorandil FFR values fell between 0.70-0.90, suggesting that most of the lesions were functionally intermediate stenoses. Unimodal distribution was confirmed by Hartigan’s dip test (D statistics and p-value: 0.026, p=0.113 and 0.027, p=0.092, respectively) (Figure 1).
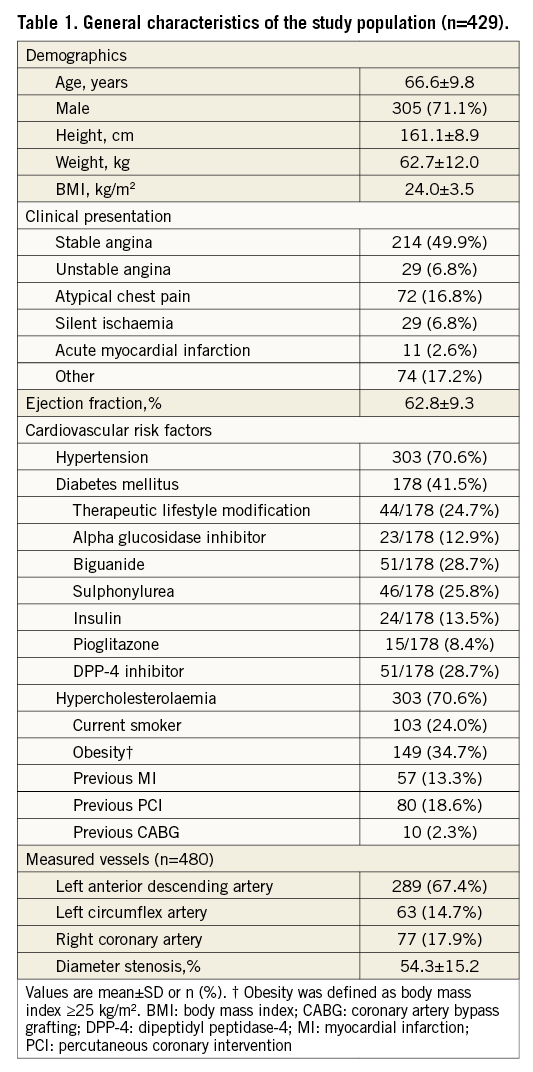
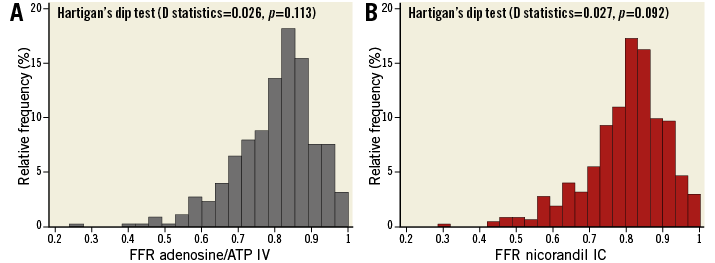
Figure 1. Distribution of FFR values. The distributions of FFR values with relative frequency are presented. A) FFR values measured with IV infusion of adenosine/ATP. B) FFR values measured with IC administration of nicorandil 2 mg. ATP: adenosine triphosphate; FFR: fractional flow reserve; IC: intracoronary; IV: intravenous
HYPERAEMIC EFFICACY AND FFR VARIABILITY BETWEEN TWO DIFFERENT METHODS OF HYPERAEMIA INDUCTION
Table 2 shows the hyperaemic efficacy of IV adenosine/ATP and IC nicorandil. The median FFR value with IV adenosine/ATP was 0.82 (0.74-0.88) and that with IC nicorandil was 0.82 (0.75-0.87) (p for difference=0.207) (Table 2). Both FFR values showed an excellent correlation (r=0.941, p<0.001), with negligible mean differences and narrow 95% limits of agreement (mean difference 0.002, 95% limits of agreement -0.056-0.061) (Figure 2). There were only three patients (0.7%) who showed changes in classification across the grey zone (0.75-0.80), in which the FFR was >0.80 with one hyperaemic agent and ≤0.75 with another agent.
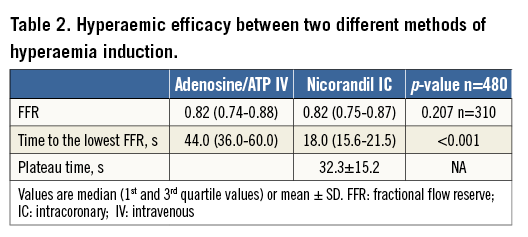
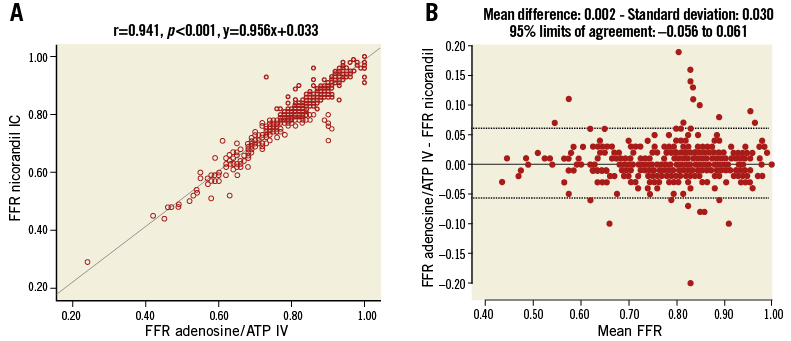
Figure 2. Correlation and reproducibility between FFR measurements of IV adenosine/ATP and IC nicorandil. A) Strong correlation with linear association between FFR values with IV infusion of adenosine/ATP and IC administration of nicorandil 2 mg was observed. B) Both FFR values showed excellent reproducibility. ATP: adenosine triphosphate; FFR: fractional flow reserve; IC: intracoronary; IV: intravenous
IC nicorandil showed earlier achievement of hyperaemia (time to lowest FFR: 44.0 s [36.0-60.0] for IV adenosine/ATP and 18.0 s [15.6-21.5] for IC nicorandil, p<0.001), and the plateau time of IC nicorandil was 32.3±15.2 s (median 34.6) (Table 2). Overall classification agreement for FFR ≤0.80 or FFR ≤0.75 between IV adenosine/ATP and IC nicorandil was 90.8% (kappa=0.814, p<0.001) or 95.2% (kappa=0.878, p<0.001), respectively. ICC was 0.980 (p<0.001) between IV adenosine/ATP and IC nicorandil. The area under the curve (AUC) of IC nicorandil to predict IV adenosine/ATP FFR ≤0.80 was 0.969 (95% CI: 0.955-0.983). The AUC of IC nicorandil to predict IV adenosine FFR ≤0.80 and IV ATP FFR ≤0.80 was 0.973 (95% CI: 0.954-0.993) and 0.968 (95% CI: 0.949-0.987), respectively (Figure 3).
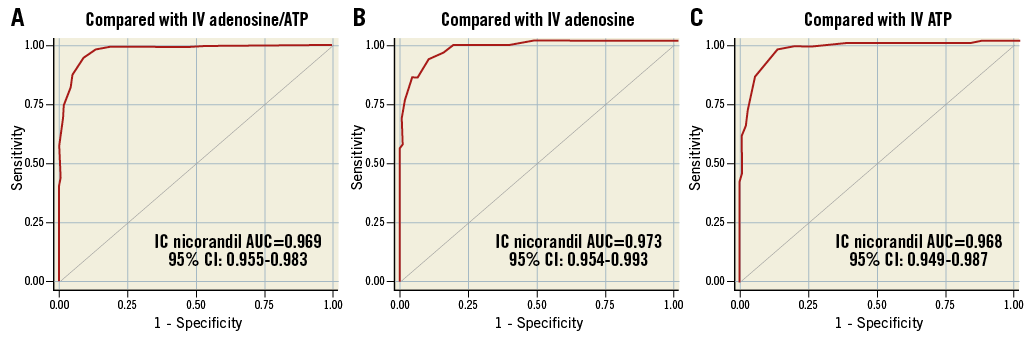
Figure 3. Classification agreement of FFR measurements of IC nicorandil. Classification agreement of FFR values measured with IC nicorandil administration was compared with (A) IV infusion of adenosine/ATP; (B) IV adenosine only; (C) IV ATP only. ATP: adenosine triphosphate; AUC: area under the curve; CI: confidence interval; IC: intracoronary; IV: intravenous
In reproducibility and per-range agreement analysis, classification agreement per 0.05 interval between the two measurements using IV adenosine was 100% at each extreme, falling to about 80% around a mean FFR value of 0.80. A strong correlation was also observed between the two FFR measurements with IC nicorandil. Classification agreement per 0.05 intervals between the two FFR values using IC nicorandil was 100% at each extreme and decreased to 68% around a mean FFR value of 0.80. Correlation between FFR values with IV adenosine and FFR values with IC nicorandil administration was excellent. Classification agreement was 100% at each extreme, decreasing to 69.2% around a mean FFR value of 0.80 between IV adenosine and IC nicorandil FFR (Appendix Figure 2).
HAEMODYNAMIC CHANGES DURING INDUCTION OF HYPERAEMIA AND FFR VARIABILITY ACCORDING TO HAEMODYNAMIC VARIABILITY
In order to evaluate the effect of haemodynamic changes during hyperaemia on FFR variability, 220 patients whose haemodynamic parameters were recorded were analysed separately. IV adenosine/ATP induced significantly higher reduction in BP and increase in HR, compared with IC nicorandil (both p-values <0.001) (Table 3). However, when ΔBP or ΔHR were compared with changes in FFR values (ΔFFR) between IV adenosine/ATP and IC nicorandil administration, there were no significant correlations, either between ΔBP and ΔFFR (r=–0.114, p=0.091) or between ΔBP and ΔFFR (r=1.000, p=0.151) (Figure 4).
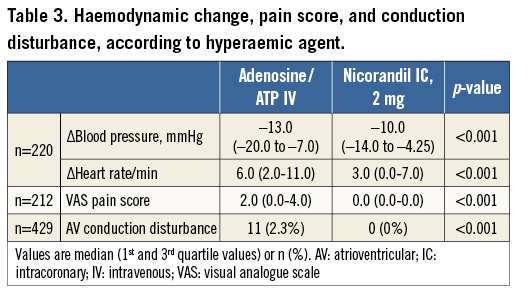
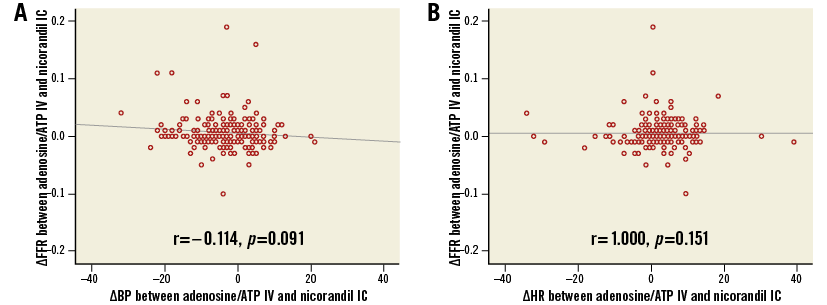
Figure 4. Haemodynamic changes and variability of FFR according to hyperaemic agents. In comparison of IV infusion of adenosine/ATP with IC administration of nicorandil 2 mg, there were no correlations (A) between changes in blood pressure (ΔBP) and changes in FFR (ΔFFR) measurements or (B) between changes in heart rate (ΔHR) and ΔFFR measurements. ATP: adenosine triphosphate; FFR: fractional flow reserve; IC: intracoronary; IV: intravenous
Among the total population, 44 patients showed substantial BP reduction (>20 mmHg) during the infusion of IV adenosine/ATP, but not with IC bolus administration of nicorandil 2 mg. In these patients, the excellent correlation and classification agreement of FFR values between IV adenosine/ATP and IC nicorandil were still maintained and even showed significantly higher correlations between the two FFR values than the results from the overall cohort (r=0.979, ICC 0.989, CA 95.5%, kappa=0.906, AUC of IC nicorandil 0.994, all p-values <0.001, and p for comparison of correlation coefficient with overall cohort <0.001).
In addition, IV adenosine/ATP infusion caused a significantly higher VAS pain score than IC nicorandil, and also caused a significantly higher incidence of AV conduction disturbance (2.3% vs. 0.0%, p<0.001) (Table 3).
IMPACT OF TARGET INTERROGATED VESSELS OR BODY MASS INDEX
The excellent correlation and classification agreement between FFR values from IV adenosine/ATP and IC nicorandil administration were maintained, regardless of the different target interrogated vessels (Appendix Figure 3). Although the mean difference between FFR values from IV adenosine/ATP and IC nicorandil in the left circumflex artery (LCX) was significantly higher than in the LAD or RCA, the absolute value of mean differences across the different target vessels was minimal to affect the decision for revascularisation (mean differences 0.003, –0.005, and 0.006 for LAD, LCX, and RCA, respectively) (Appendix Figure 3). In addition, ΔFFR was not influenced by ΔBP or ΔHR, regardless of the different target interrogated vessels, as with the results of the overall analysis (Appendix Figure 4). The excellent correlation and classification agreement between FFR values from IV adenosine/ATP and IC nicorandil administration were also maintained, regardless of BMI (Appendix Figure 5).
THE IMPACT OF SULPHONYLUREA ON THE EFFECTS OF NICORANDIL
Among patients with diabetes mellitus, 46 (25.8%) had been treated with sulphonylurea and showed no differences in FFR values between IV adenosine/ATP and IC nicorandil (0.82 [0.74-0.87] vs. 0.81 [0.76-0.86], p=0.077). Patients with diabetes mellitus and sulphonylurea treatment also showed excellent correlation and classification agreement for an FFR value ≤0.80 between IV adenosine/ATP and IC nicorandil (r=0.965, ICC 0.982, CA 90.2%, kappa=0.919, AUC of IC nicorandil 0.991, all p-values <0.001).
The Appendix describes the study results further.
Discussion
In this study, we evaluated the correlation and classification agreement of FFR values between IV adenosine/ATP infusion and IC nicorandil from a pooled population, composed predominantly of patients with angiographically and functionally intermediate coronary lesions. IC nicorandil showed a significantly faster induction of hyperaemia along with significantly less development of chest pain, AV conduction disturbance, and a smaller decrease in BP during hyperaemia. The plateau time of IC nicorandil was about 32 seconds, which is sufficient to use the thermodilution method to obtain coronary flow reserve and index of microcirculatory resistance (IMR) and pressure-wire pullback tracings. Haemodynamic changes did not have any impact on the measured values of FFR, regardless of the different hyperaemic agents with different routes of administration. In addition, the reproducibility and classification agreement of FFR values between IV adenosine/ATP infusion and IC nicorandil were not influenced by the different target interrogated vessels or by the use of sulphonylurea.
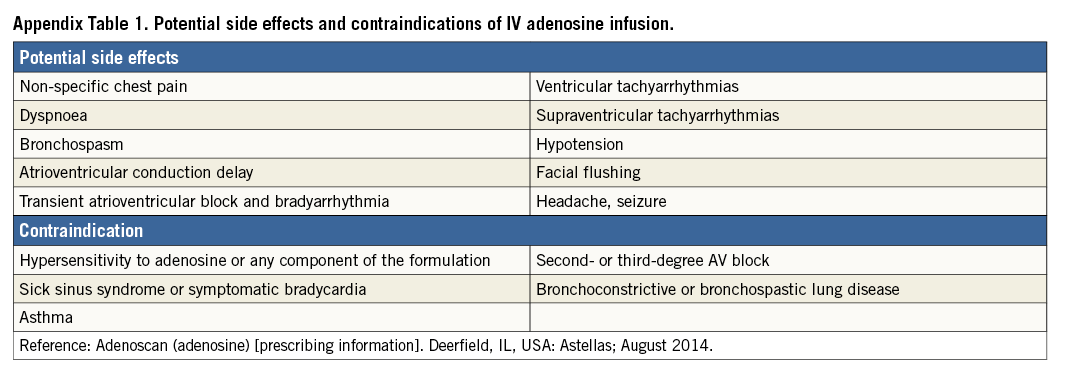
NICORANDIL AS A NOVEL HYPERAEMIC AGENT AND AN ALTERNATIVE FOR IV ADENOSINE/ATP
Theoretically, FFR is calculated under the assumption of a linear relationship between coronary flow and pressure during maximal coronary vasodilation with minimal and stable microvascular resistance3. Therefore, achieving maximal hyperaemia is an essential prerequisite for the accurate measurement of FFR values, and IV infusion of adenosine via a central vein has been the gold standard method for hyperaemia2,3. However, this technique requires an additional femoral venous access route, along with the potential complications of high-dose adenosine infusion, such as AV conduction disturbance, bronchial hyperreactivity, and chest pain (Appendix Table 1). Whilst the IC bolus injection of adenosine is a more convenient and simpler method than IV adenosine infusion, the hyperaemic efficacy of this method is suboptimal in some patients, in that the haemodynamic changes could be different with IV adenosine infusion, and this method cannot provide sufficient hyperaemic duration for pressure pullback tracings and IMR measurement10. Nicorandil is a nicotinamide ester and has a dual mechanism of action, i.e., first, it is an ATP-sensitive potassium channel opener which dilates coronary resistance arterioles, and second, it induces nitric oxide, which dilates epicardial coronary arteries1,5. Therefore, nicorandil dilates both macrovascular and microvascular systems. In addition, there is mounting evidence that IC nicorandil provides a cardioprotective effect, including reducing periprocedural myocardial injury after elective PCI and preventing microvascular dysfunction after primary PCI for ST-elevation myocardial infarction11,12. In this study, we comprehensively evaluated the hyperaemic efficacy and safety of IC nicorandil from pooled individual patient data from all previously published studies which evaluated IC nicorandil as a hyperaemic agent for invasive physiologic measurements1,4-7. This large sample size of a pooled population, who presented with predominantly intermediate stenoses, enabled us to evaluate some remaining concerns regarding the potentially limited hyperaemic efficacy of IC nicorandil in patients with diabetes mellitus treated with sulphonylurea or differential hyperaemic efficacy according to the different target interrogated vessels.
HYPERAEMIC EFFICACY AND SAFETY OF NICORANDIL
The hyperaemic efficacy of an IC bolus of nicorandil 2 mg was similar to the IV infusion of adenosine 140 μg/kg/min and ATP 150 μg/kg/min. However, time to the lowest FFR was significantly reduced with IC nicorandil, despite the less significant decrease of BP or increase in HR than in IV adenosine/ATP infusion. Along with similar hyperaemic efficacy, IC nicorandil caused significantly fewer incidences of AV conduction disturbance and chest pain compared with IV adenosine/ATP infusion. Nonetheless, the mean duration of plateau time was about 32 seconds, which might be sufficient to perform pressure pullback tracing for simple lesions, yet may be insufficient to measure IMR and to perform pressure pullback tracings in complex lesions for less experienced operators. Considering the abovementioned results, IC nicorandil 2 mg is thought to be a reasonable alternative as a hyperaemic agent for FFR measurement when clinically indicated, especially in patients with borderline hypotension, AV conduction disturbance, underlying bronchial hyperreactivity, such as asthma, insufficient hyperaemic responses to IV or IC adenosine administration, poor IV access site, and possibly in patients with obesity (defined as BMI ≥30 kg/m2) who have been reported to show more frequent hypotensive responses to IV adenosine infusion12,13.
FFR VARIABILITY ACCORDING TO HAEMODYNAMIC CHANGES
Previously, there have been concerns regarding the variability of FFR according to haemodynamic changes, especially decrease of hyperaemic aortic pressure, due to IV adenosine infusion14. The rationale for this concern is that decreasing aortic pressure (Pa) might reduce maximal coronary flow during hyperaemia and thereby underestimate FFR values15. However, those changes in BP or HR obviously were not associated with changes in FFR values according to the current study, whose populations were enrolled from multiple centres in Korea and Japan. In addition, in 44 patients who showed a substantial BP drop (>20 mmHg) during the infusion of IV adenosine/ATP, but not with an IC bolus administration of nicorandil 2 mg, the excellent correlation and classification agreement of FFR values between IV adenosine/ATP and IC nicorandil did not change at all. Our current and previous results4 reaffirm the previous work of de Bruyne et al who reported that FFR values showed minimal variation during haemodynamic changes induced by rapid atrial pacing, nitroprusside infusion, or dobutamine infusion16.
These findings suggest that the changes in haemodynamic conditions due to different hyperaemic agents and routes of administration do not significantly affect the measured FFR values in the clinical decision-making process in real-world practice.
Some previous reports have raised concern about limited “true” hyperaemic efficacy with one specific hyperaemic agent due to the complex mechanism of coronary vasodilation14. Although the mechanism of action with nicorandil is inherently different from adenosine, with dual mechanisms to induce hyperaemia, there was no difference in FFR values measured with IV adenosine/ATP and IC nicorandil. Our results are in line with the individual studies which were pooled in the current study. Furthermore, Jang et al clearly showed that the additional administration of IC nicorandil to IV adenosine infusion did not have an additive hyperaemic effect. Considering these results, FFR measurement showed excellent reproducibility and low variability, regardless of different hyperaemic agents, different routes of administration, changes in haemodynamic parameters, or multiple mechanisms of coronary vasodilation.
ISSUES REGARDING DIFFERENT TARGET INTERROGATED VESSELS AND SULPHONYLUREA USE
Since nicorandil was administered via an IC bolus injection, there might be a possible influence of different coronary flow patterns in the distribution of nicorandil throughout the coronary arteries. Nonetheless, there were no differences regarding correlations and classification agreement between IV adenosine/ATP and IC nicorandil according to the different target interrogated vessels. Although the mean difference between two FFR values (ΔFFR) was slightly higher in the LCX compared with the LAD and RCA, the absolute difference in ΔFFR among the coronary arteries ranged from 0.008 (LAD-LCX) to 0.011 (RCA-LCX), which is obviously too small to influence clinical decision making in real-world practice.
In addition, there has been concern about the limited hyperaemic efficacy of nicorandil in patients with diabetes mellitus being treated with sulphonylurea. Since sulphonylurea, which is one of the most commonly used oral hypoglycaemic agents in diabetic patients, predominantly acts with inhibition of ATP-sensitive potassium channel opening, it might show drug interaction with nicorandil, the ATP-sensitive potassium channel opener17. However, FFR values measured with IC nicorandil administration did not show any difference with those measured with IV adenosine/ATP infusion. This might be explained by the fact that any oral hypoglycaemic agent is usually discontinued prior to the invasive procedure. Since the duration of the biologic effect of most sulphonylureas is less than 24 hours18, the impact of sulphonylurea on FFR measurement with IC nicorandil might be minimal in real-world practice. However, some agents in the sulphonylurea category (glyburide, glimepiride) can last more than 24 hours due to the formation of active metabolites. Therefore, these specific kinds of oral hypoglycaemic agents may need to be discontinued earlier than others19.
Limitations
Some limitations of the current study should be considered. First, nicorandil is not available in all countries, despite its rapid action and excellent safety profile. Although there has been mounting evidence regarding the additional cardioprotective action of nicorandil in both elective PCI for stable angina and primary PCI for acute myocardial infarction, the limited availability of the drug represents a major obstacle to expanding its use in real-world practice. Second, this study is a patient-level pooled analysis of five studies, and therefore there is some possibility of selection bias. Since all previous studies were non-blinded, in that blinding the physician is inherently impossible, there is some possibility of subjectivity in the interpretation of pressure tracings. Third, haemodynamic parameters were not available for the entire pooled population. Last, among the total population, 216 patients (50.3%) underwent FFR measurement with adenosine/ATP IV followed by FFR measurement with nicorandil IC administration without the randomisation of administration order. In these patients, we cannot fully exclude the possible influence of the 1st hyperaemic agent on the effect of the 2nd agent.
Conclusion
Nicorandil IC bolus injection is a simple, safe and effective hyperaemic method for FFR measurement and can be used as a substitute for adenosine in patients with coronary artery disease.
| Impact on daily practice Intracoronary nicorandil showed significantly earlier achievement of hyperaemia with similar hyperaemic efficacy, compared with intravenous adenosine/ATP. Along with the favourable hyperaemic efficacy of IC nicorandil, it produced significantly fewer changes in blood pressure and heart rate, and showed significantly less chest pain than IV adenosine/ATP. Nicorandil IC bolus injection is a simple, safe and effective hyperaemic method for FFR measurement and can be used as a substitute for adenosine in patients with coronary artery disease. |
Conflict of interest statement
B.K. Koo has received an institutional research grant from St. Jude Medical. The other authors have no conflicts of interest to declare.
Appendix. Results: cost of nicorandil and adenosine as hyperaemic agents in Korea
In Korea, nicorandil is supplied as one vial (48 mg) at a cost of $22.00/vial. Conversely, adenosine (Adenocor®; Sanofi-Aventis, Frankfurt, Germany) is supplied as one vial (6 mg) at a cost of $6.64/vial. To induce hyperaemia in a 70 kg patient with an infusion rate of 140 μg/kg/min would require 10 vials of adenosine (~$66.00) in contrast to one vial of nicorandil ($22.00), making nicorandil more cost-effective.
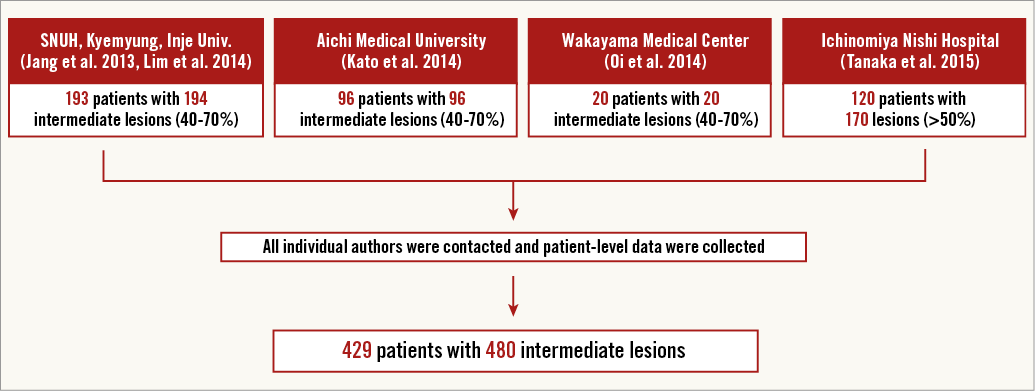
Appendix Figure 1. Construction of patient-level pooled cohort of nicorandil FFR. The study population comprised a pooled cohort of five previous studies which compared FFR measurement between IV adenosine/ATP and IC nicorandil1,4-7. A total of 480 lesions from 429 patients with coronary artery disease were included. These patients were enrolled from six centres in Japan and Korea.
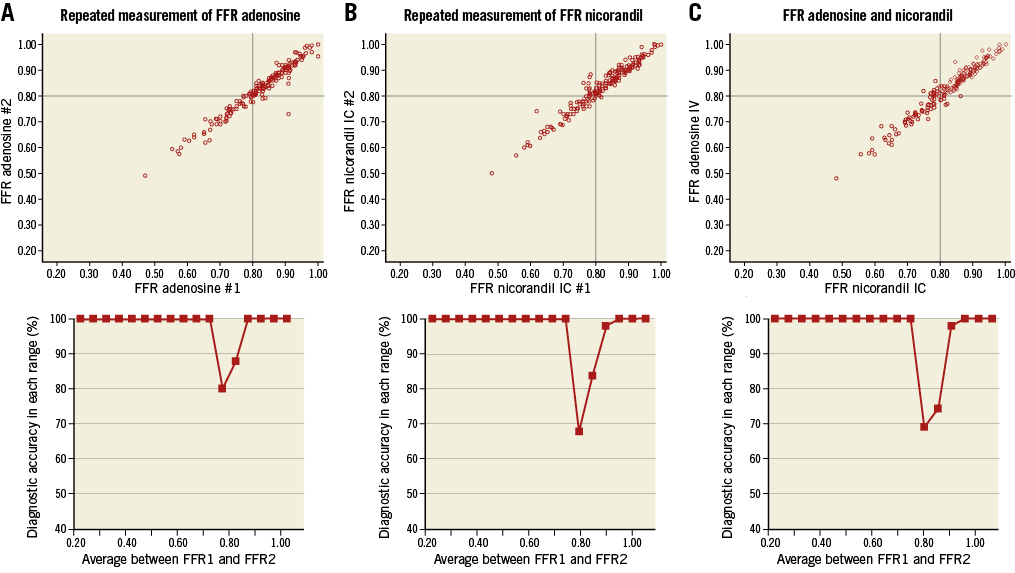
Appendix Figure 2. Correlation and per-range agreement between repeated measures of adenosine or nicorandil FFR. There was an excellent correlation between two FFR measurements with intravenous (IV) adenosine administration. Classification agreement per 0.05 interval between the two measurements was 100% at each extreme, falling to about 80% around a mean FFR value of 0.80 (A). A strong correlation was also observed between two FFR measurements with IC nicorandil. Classification agreement per 0.05 interval between the two FFR values was 100% at each extreme, decreasing to 68% around a mean FFR of 0.80 (B). Correlation between FFR values with IV adenosine and FFR values with IC nicorandil administration was also excellent and classification agreement was 100% at each extreme, decreasing to 69.2% around a mean FFR of 0.80 (C).
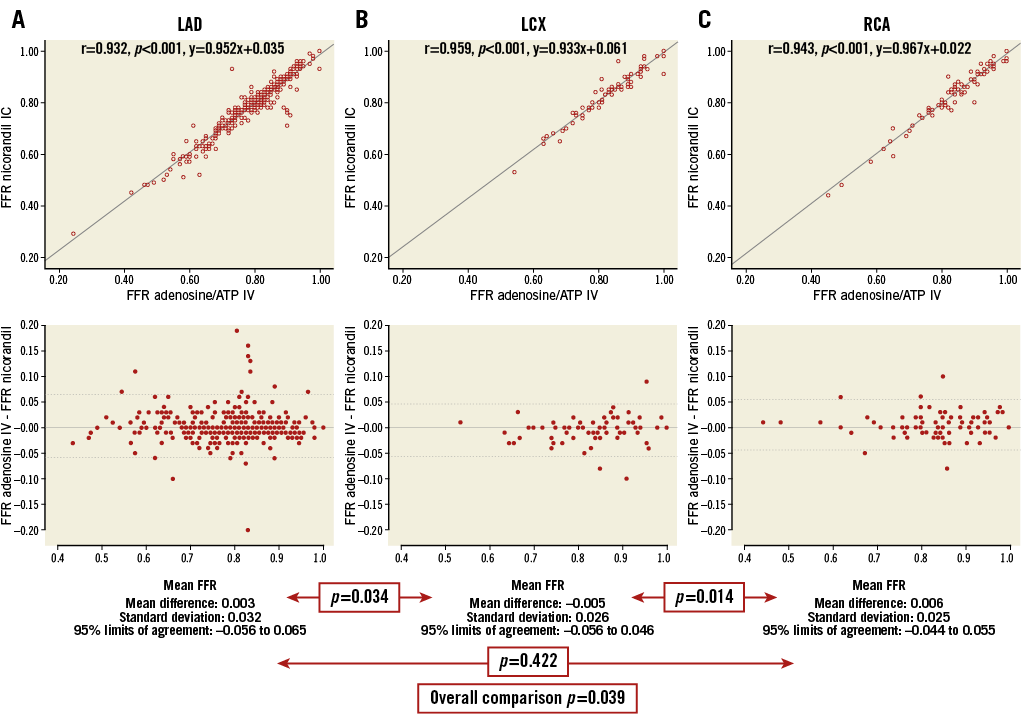
Appendix Figure 3. Correlation and reproducibility between FFR measurements of IV adenosine/ATP and IC nicorandil, according to the target vessel A) LAD; B) LCX; C) RCA. A strong correlation with linear association between FFR values with intravenous infusion of adenosine/ATP and intracoronary administration of nicorandil 2 mg was observed, regardless of the different target interrogated vessels. ATP: adenosine triphosphate; FFR: fractional flow reserve; IC: intracoronary; IV: intravenous
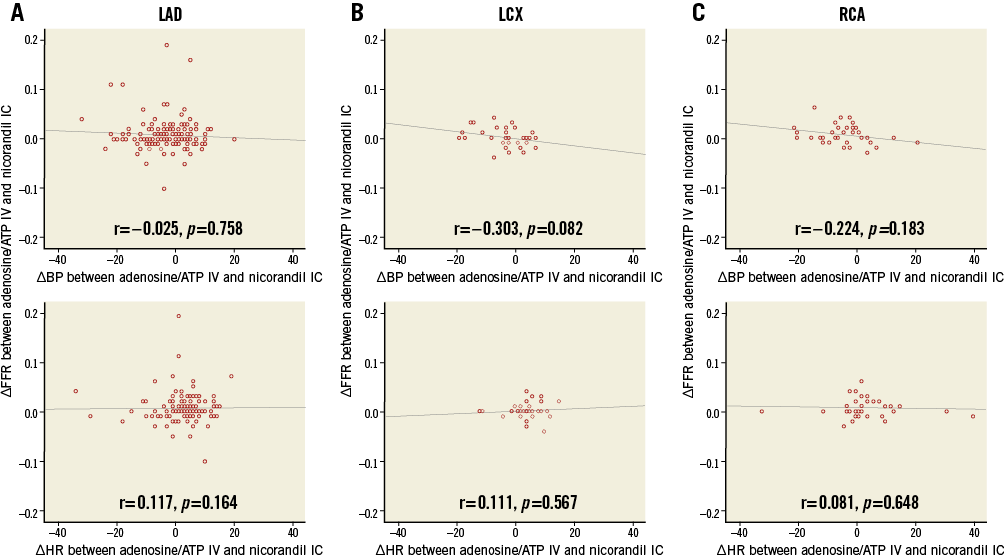
Appendix Figure 4. Haemodynamic changes and variability of FFR according to hyperaemic agents, according to the target vessel. A) LAD; B) LCX; C) RCA. There were no correlations between ΔFFR and any haemodynamic changes, regardless of the different target interrogated vessels. ATP: adenosine triphosphate; FFR: fractional flow reserve; IC: intracoronary; IV: intravenous
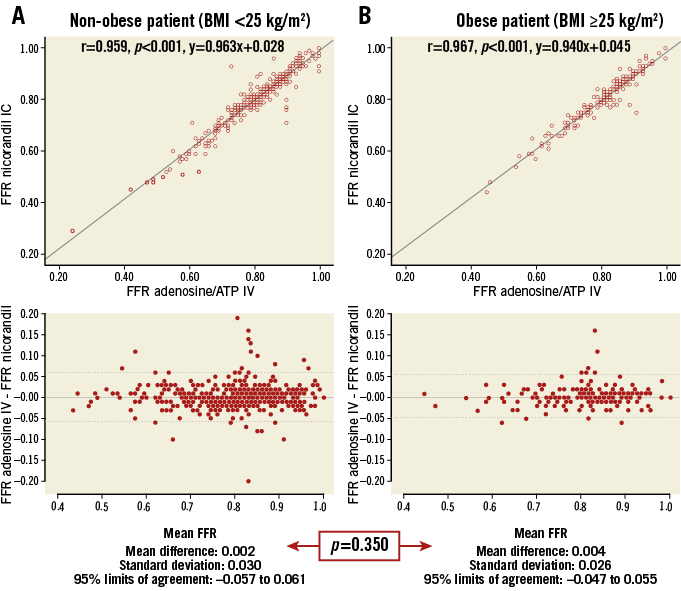
Appendix Figure 5. Correlation and reproducibility between FFR measurements of IV adenosine/ATP and IC nicorandil, according to BMI. A) Non-obese patient. B) Obese patient. Strong correlation with linear association between FFR values with intravenous infusion of adenosine/ATP and IC administration of nicorandil 2 mg was observed, regardless of accompanying obesity. ATP: adenosine triphosphate; FFR: fractional flow reserve; IC: intracoronary; IV: intravenous