
Abstract
Aims: Our aim was to examine procedural viability and midterm outcomes following the use of rotational atherectomy (RA) on malapposed, crippled, otherwise non-salvageable metallic stents (i.e., stentablation [SA]), and convey important procedural pointers for practitioners encountering such situations.
Methods and results: Data on twelve SA subjects were analysed. The primary endpoint was procedural success: effective ablation of the malapposed stent and successful implantation of a new device. Major adverse cardiac events (MACE) and all-cause death at six months following the index procedure were examined as a secondary endpoint. All twelve patients underwent successful SA and novel stent implantation, with sufficient salvage of coronary anatomy (residual stenosis <30%). At six-month follow-up, however, MACE amounted to 50% and all-cause mortality to 25% in the inspected subjects.
Conclusions: We found that, although feasible as an acute salvage option, SA distinctively increases post-procedural midterm MACE and mortality rates. This places emphasis on the importance of avoiding eventual SA situations, underlining the importance of ample lesion preparation prior to stent implantation.
Abbreviations
FU: follow-up
MACE: major adverse cardiac events
%DS: percent diameter stenosis
PCI: percutaneous coronary intervention
RA: rotational atherectomy
RA stenting: rotational atherectomy and stent implantation
SA: stentablation
Introduction
Rotational atherectomy (RA) and subsequent stent implantation (RA stenting) is the contemporary method of choice when handling uncrossable and/or undilatable coronary lesions, with several authors (including our working group) demonstrating satisfactory in-hospital and long-term results1. Unsurprisingly, corresponding guidelines and a recently published expert consensus report2 classify RA as a means of lesion/plaque modification which facilitates eventual stent deployment.
Published case reports describe a notable non-conventional RA application: using the burrs’ sheer power to ablate underexpanded and undilatable coronary stents forcefully implanted into ill-prepared lesions as a bail-out method of successfully handling this troublesome complication3.
However, despite these brave stentablation (SA) attempts, no comprehensive data on the efficacy or longer-term patency of these procedures have yet been published. Therefore, our working group sought to assess the outcomes of such procedures. Severe calcific restenosis episodes requiring RA were excluded, as strut metal ablation is not performed in such cases. Additionally, we decided to include recommended procedural pointers for practitioners encountering SA situations.
Methods
SA SUBJECTS, ENDPOINTS
After providing written consent, all subjects who undergo RA at our institution are enrolled into a prospective registry, sanctioned by our institutional ethics committee. After examining our database, we found that twelve individuals (4% of RA cases) had undergone genuine SA.
As a primary endpoint we examined procedural success. Major adverse cardiac events (MACE), encompassing new-onset myocardial infarction, target lesion failure and/or revascularisation, were assessed as a six-month secondary endpoint along with all-cause mortality.
SA SUBJECTS TREATED
All subjects examined underwent an initial, failed PCI attempt without RA. In five cases, SA was performed as a secondary (dual-instance) procedure, whereas in the other seven cases procedures were carried out in one (single-instance) session. SA interventions were executed using the RotaLink™ Plus system (Boston Scientific, Marlborough, MA, USA) guided on a standard 0.009 inch guidewire (RotaWire™; Boston Scientific).
Optimal medical therapy, according to applicable guidelines, was initiated in every case.
ANGIOGRAPHIC ANALYSIS, DEFINITIONS
Quantitative angiographic analysis was performed: segments analysed included the implanted stent and the bidirectional 2 mm overhang. The percent diameter stenosis (%DS), reference vessel diameter and crippled stent length were measured before and after SA. Acute gain was defined as the decrease in %DS after successful SA and new stent implantation. Procedural success was defined as successful RA of the crippled stent followed by an implantation of a new, adequately apposed stent (residual stenosis <30%).
FOLLOW-UP (FU) DETAILS
FU of patients was clinically driven. Morbidity and mortality data were collected and verified via personal contact, telephone calls or from records of the Hungarian National Health Insurance.
Results
DEMOGRAPHIC AND CLINICAL DATA
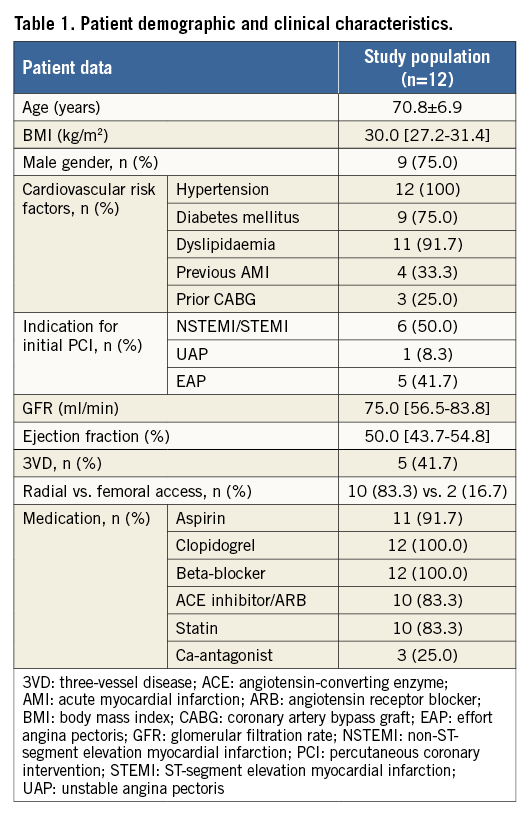
Table 1 displays all relevant demographic and clinical data of the patients. Of note is the fact that patients were mostly high-risk subjects, with numerous comorbidities, often presenting under acute coronary syndrome conditions for the initial PCI.
PROCEDURAL, ANGIOGRAPHIC AND MACE DATA
Table 2 contains procedural and quantitative angiographic data. All subjects underwent successful SA and eventual secondary stent implantation. Successful high-pressure post-dilation was carried out in every case. Residual stenosis was low with a median of 10.0% (0.0-20.0 interquartile range) and final lumen gain was considerable: median 60.0% (50.0-72.5 interquartile range).
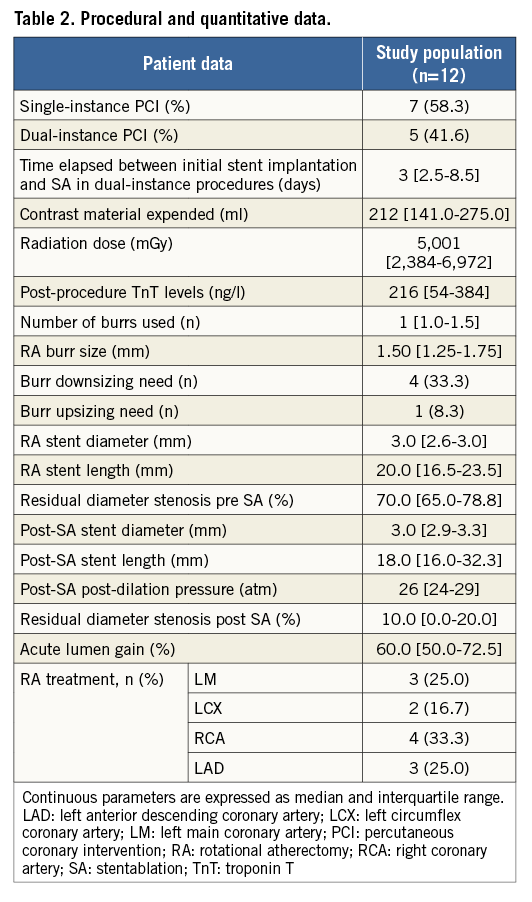
Table 3 contains relevant data on adverse events. There were no in-hospital MACE or fatalities, but procedural adverse events were encountered in every case. Most notable were burr deceleration, balloon rupture and sticking.
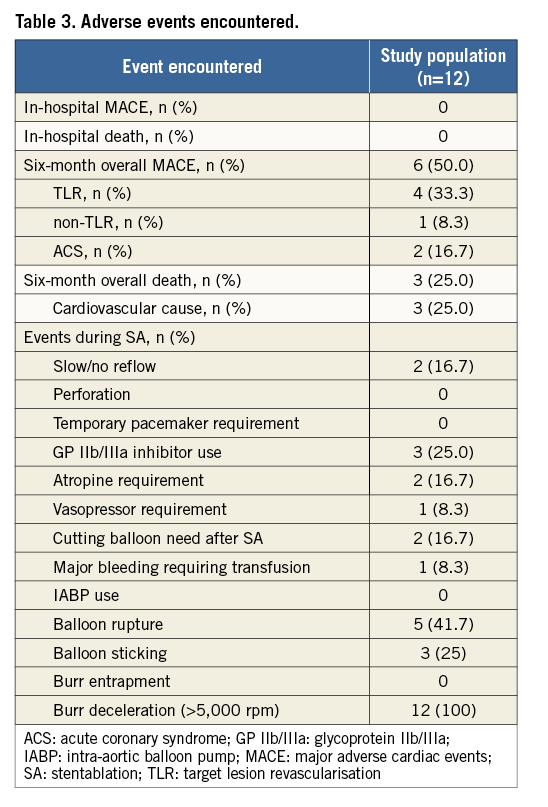
At the six-month FU visit, MACE had occurred in 50% (n=6) of the investigated subjects, while 25% (n=3) of the patients had died, all due to cardiovascular causes.
Discussion
Our study involving SA subjects, although limited in numbers, yielded interesting results for RA practitioners. Below, we would like to sum up procedure viability and alternative options, patient-related implications and a series of important recommendations for eventual procedures.
VIABILITY OF SA PROCEDURES, ALTERNATIVES
Our data have shown that, if required, SA is a viable option for handling a profoundly difficult situation. We verified that RA of stents is possible with excellent procedural results. In addition, an alternative or even synergic method with SA can be the use of excimer laser atherectomy, where similar results were reported4 in corresponding clinical situations.
IMPLICATIONS ON MACE AND MORTALITY
The secondary endpoints investigated proved that, despite initial procedural success, six-month adverse events were plentiful (Table 3). Nevertheless, calcified coronary disease by itself harbours an increased risk of mortality and morbidity. Furthermore, PCI outcomes are known to be more modest in this patient population, indicating a potentially higher intrinsic risk.
RECOMMENDATIONS FOR SA
Lastly, we sought to recommend key points when operators encounter an unavoidable SA situation. If required, the subject should be transferred to a competent RA-capable centre as soon as possible.
Advancement of the RA guidewire may prove difficult through a crippled stent. RotaWires should be advanced along a primary, conventional guidewire to make adequate placement unproblematic. This initial guidewire should only be removed once the RotaWire has reached a promising position. If direct RotaWire delivery along the first device proves unsuccessful after multiple attempts, the use of coronary microcatheters or small-profile over-the-wire balloons is recommended for exchange.
RA of a crippled stent should be performed at maximum turbine power (~180,000-190,000 rpm) with a smaller diameter burr. Besides chiselling of the stent, the role of SA further extends to fracturing the ring calcification underneath the malapposed stent, allowing additional manipulation. We only recommend the 1.25 or 1.5 mm burr to start the procedure. Upon first contact of the burr and the malapposed metallic structure, operators will encounter a significant drop (>5,000 rpm) in turbine speed. Increased finesse and attention is mandatory at this time point to avoid catastrophic burr jamming and/or entrapment5. Slow and delicate, gradual movement of the burr is recommended upon initial and further stent contact. If the first burr fails to pass the metallic struts, even after several (~10) runs, downsizing is always the endorsed practice. However, if operators do encounter burr entrapment, the methods previously reported should be undertaken to recover this complication2.
Once the burr initially clears the crippled stent, ablation runs should be continued until no drop in turbine speed is encountered during passage. Extended, upsized non-compliant balloon dilatations are necessary afterwards, until full expansion is evident. If this proves unsuccessful due to balloon crossing or expansion failure, upsizing the burr should be considered to a maximum burr/artery ratio of 0.6-0.7, with repeat high-pressure dilations afterwards. The use of coronary microtomes is also an option at this time. Only after sufficient expansion of these balloons should operators attempt to advance a new stent into the lesion. The novel stent should cover the entire ablated portion of the initial device and a final post-dilation is also mandatory.
Although not conducted during our procedures, intracoronary imaging is strongly recommended both before and after SA, as well as after secondary stent implantation in order to assess detailed intraluminal parameters.
Limitation
The main limitations of our work are that our study group was limited to twelve subjects and intravascular images were not obtained.
Conclusions
To sum up our experiences regarding SA, we acknowledge our considerable midterm MACE and mortality frequencies, despite promising in-hospital outcomes. We would like to emphasise that the main message of the work is to point out that substantial measures should be taken to avoid the need for SA, thus again underlining the need for ample lesion preparation before stent implantation. However, if absolutely required, SA is a solid option for treatment and coronary salvage.
| Impact on daily practice Stentablation is a tactic which may justly be considered by interventional cardiologists when facing the problem of an ill-fated, malapposed stent that is refractory to further balloon manipulation. Yet, few have attempted this manoeuvre given its apparently invasive nature. Stentablation has been shown to be an effective emergency treatment option, a way to salvage coronary anatomy. Nonetheless, utilisation is discouraged due to distinctly poor midterm outcomes. Emphasis lies on preventing situations that require eventual stentablation by meticulous, thorough lesion preparation before stent implantation may be considered. Stentablation thus remains only a bail-out option. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

