Introduction
Device embolisation is a complication after left atrial appendage closure (LAAC) and may occur in up to 0.24% cases1,2. The Munich consensus document defines the need for repeated catheterisation in case of embolisation as a major device embolisation, while a successful retrieval in the same procedure is considered a minor embolisation3. However, information on retrieval strategies for embolised LAAC devices is scarce.
Methods
PATIENT COHORT
The Cardioangiologisches Centrum Bethanien (CCB) Frankfurt database was used to identify patients with LAAC device embolisations and retrieval attempts between April 2010 and October 2019.
DEVICE RETRIEVAL
Percutaneous LAAC retrieval was performed by experienced cardiologists.
All procedures were executed taking account of guidelines such as the Munich consensus document3.
Results
MINOR AND MAJOR EMBOLISATION
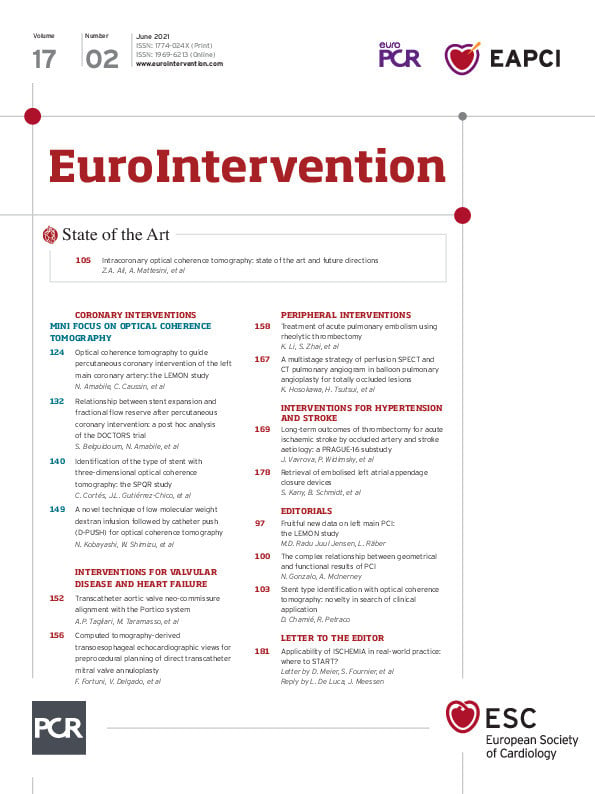
A total of 711 devices were implanted (Table 1). Total minor embolisation was 0.7% (n=5) and total major embolisation 0.8% (n=6). Major embolisation included WATCHMAN™ (n=2) (Boston Scientific, Marlborough, MA, USA), AMPLATZER™ Cardiac Plug (ACP) (n=2) (Abbott Vascular, Santa Clara, CA, USA), AMPLATZER™ Amulet™ (n=1) (Abbott Vascular) and LAmbre™ (n=1) (Lifetech Scientific, Shenzhen, China). Two additional cases were referred by external hospitals (WATCHMAN, n=1; Amulet, n=1).
TRANSSEPTAL RETRIEVAL FROM THE LEFT ATRIUM (n=6)
Transseptal retrieval of LAAC devices from the left atrium (LA) was attempted in six patients (ACP, n=2; AMPLATZER Amulet, n=3; Coherex WaveCrest® [Biosense Webster, Inc., Diamond Bar, CA, USA], n=1). While in four cases the embolisation was seen during implantation, in one patient it was discovered 47 days post implantation.
After transseptal puncture, a steerable sheath (MitraClip® delivery sheath [Abbott Vascular], 21 Fr inner diameter [ID], n=1; WaveCrest® delivery sheath, 17 Fr, n=1; and Cryoflex™, 12 Fr ID [FlexCath Advance™; Medtronic, Minneapolis, MN, USA], n=4) was placed in the LA. Procedural details are shown in Supplementary Table 1.
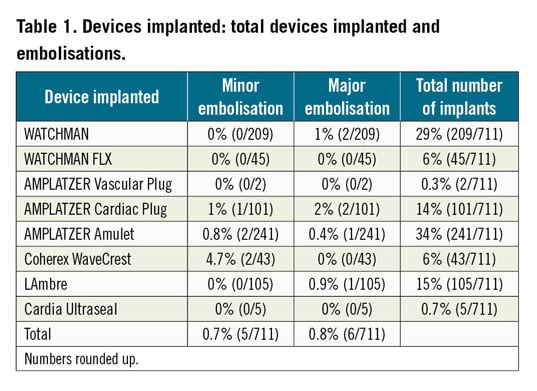
In four cases (ACP/Amulet; n=3, Coherex WaveCrest; n=1), the device was dislocated into the LA. For fixation, a 30 mm gooseneck snare was used to grab the occluder. For ACP/Amulet retrieval, a second 15 mm gooseneck snare was advanced to grab the central screw (Figure 1, Moving image 1). The Coherex WaveCrest occluder could only be partially retracted into the sheath. Subsequently, it was pulled through the interatrial septum (Figure 2).
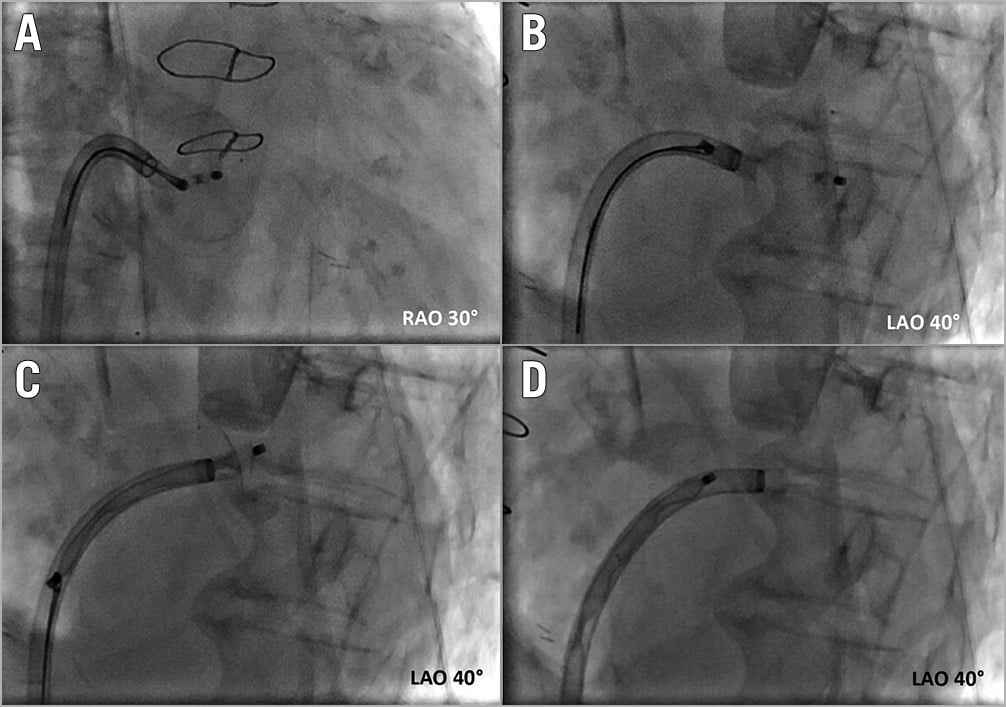
Figure 1. Transseptal retrieval of an ACP from the LA via a steerable sheath. A) The disc’s screw is snared to the IAS. B) - D) Stepwise complete retraction of the disc and the lobe into the sheath.
Figure 2. Transseptal retrieval of a Coherex WaveCrest device from the LA. A) Anterior-posterior (PA) projection of an occluder in the LA. B) Fixation through the 17 Fr delivery sheath with a 30 mm gooseneck snare. C) Unsuccessful re-sheathing. Therefore, retraction of the fixed device and sheath through the IAS (D), the right atrium (E), and through the femoral vein (F).
In one case, Amulet fixation failed and the device embolised into the aorta. After arterial access, the occluder was pulled into the 12 Fr sheath by a gooseneck snare.
In one patient a first-generation Amulet device could not be retracted into the sheath. The device was then retracted through the interatrial septum and removed by snaring.
One Amulet was partially dislodged in the LAA. Despite extensive manipulation using gooseneck snares and bioptomes, the device could not be retracted into the sheath. The procedure was abandoned and oral anticoagulation (OAC) continued.
TRANSARTERIAL RETRIEVAL FROM THE AORTA (n=5)
In four patients device retrieval from the aorta was attempted (Amulet 22 mm, n=1; WATCHMAN [21 and 24 mm], n=2; Coherex WaveCrest 27 mm, n=1; LAmbre 36/40 mm, n=1) using fluoroscopy via arterial access.
For Amulet retrieval, the central screw was snared and the device retracted. WATCHMAN occluders were retrieved by pulling the devices with a gooseneck snare or vascular forceps (Supplementary Figure 1).
In one patient, a complex Coherex WaveCrest device retrieval from the descending aorta (Supplementary Figure 2, Moving image 2) was performed. Failed retraction into a 12 Fr sheath using a gooseneck snare led to dislodgement to the iliac bifurcation.
From the left femoral artery (16 Fr), the central hub of the device was wired, and the wire snared from the right femoral access sheath. Then, a balloon was advanced over the wire from the right femoral artery (12 Fr) to push the occluder while simultaneously pulling the device with retrieval forceps from the left.
Similarly, one embolised LAmbre device could not be retrieved by gooseneck snare (Supplementary Figure 3, Moving image 3). Bilateral arterial access was gained, and the device was retrieved by a push and pull manoeuvre.
RETRIEVAL FROM THE LEFT VENTRICLE (n=2)
In two patients (Amulet, n=1; WATCHMAN, n=1) the device embolised to the left ventricle one day post implantation.
After transseptal access via a 12 Fr steerable sheath, extensive manipulation was performed using a steerable electrophysiology (EP) catheter and snaring, but retrieval failed. Consequently, the patient became haemodynamically unstable due to acute mitral regurgitation. The patient was transferred to emergency heart surgery. After successful device explant and mitral valve repair, the patient went into acute right heart failure and died three weeks after the procedure.
The second patient with left ventricular (LV) embolisation was referred directly to successful surgical salvage.
Discussion
Despite the small number of patients, it appears feasible and safe to attempt percutaneous retrieval for devices embolised to the LA or aorta; however, surgery may be favoured for devices in the LV.
The AMULET registry reported a major device embolisation rate of 0.2%, while in EWOLUTION and in the post-approval WATCHMAN experience embolisation rates were reported as 0.2% and 0.24%, respectively1,2,4. This single centre reports a major embolisation rate of 0.8%. This included early market experience and one first-generation Amulet. Additionally, an unexpectedly high embolisation rate of the Coherex WaveCrest occluder of 4.7% was observed.
In contrast to a recent meta-analysis of case reports5, we discovered device embolisation within 24 hours after implant in 12/13 cases. This underscores the recommendation for adequate imaging before discharge. Moreover, the same meta-analysis revealed embolisation to the LV as the most common location in 43%5 in contrast to our data where the LV was the least common location (15%). This may be due to possible reporting bias in case reports.
For successful percutaneous retrieval, a large bore sheath (12-16 Fr) should be used to allow complete re-sheathing of the device. In the LA, steerable sheaths are helpful to improve manoeuvrability. Device fixation tools include gooseneck snares and bioptome forceps. Re-sheathing of some device types is difficult and successful retrieval warrants complex strategies. Interventional device retrieval from the LV is discouraged if device interaction with the mitral apparatus is present.
Limitations
This report is observational and retrieval approaches were left to the cardiologist’s discretion. Additionally, the total number of embolisations is small (n=11 + 2 external LAAC devices).
Conclusion
Transcatheter retrieval of embolised devices is safe in most cases. Device retrieval from the LV carries a high risk of structural damage to valves and should prompt referral to cardiac surgery.
|
Impact on daily practice These data and the educational moving images have instructional value for a planned retrieval procedure. Transcatheter retrieval of LAAC devices embolised to the LA or the aorta appears safe and feasible. Percutaneous device retrieval from the LV should not be considered, and patients should be referred for heart surgery. |
Funding
Institutional funding by CCB.
Conflict of interest statement
B. Schmidt has received speaker fees from Boston Scientific, Abbott and Lifetech. M. Piorkowski has received speaker’s honoraria from W.L. Gore, C.R. Bard, Veryan Medical, and Philips B.V. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Transseptal retrieval of an ACP from the LA via a steerable sheath. The disc’s screw is snared to the IAS. Stepwise complete retraction of the disc and the lobe into the sheath. IAS: interatrial septum
Moving image 2. Percutaneous retrieval of a Coherex WaveCrest device from the aorta.
Moving image 3. Percutaneous retrieval of a LAmbre device from the aorta.