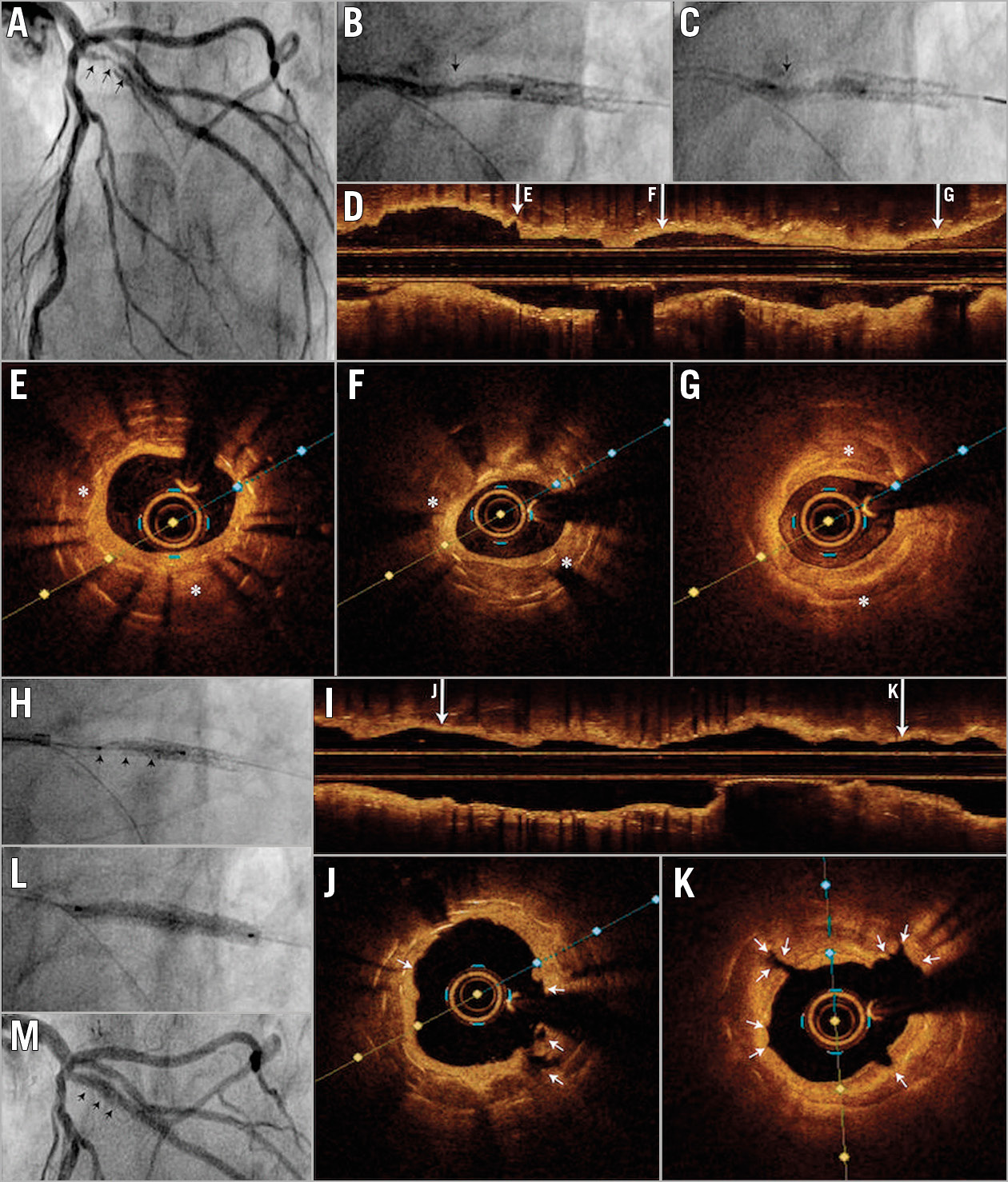
Figure 1. Treatment of calcific neoatherosclerosis with intravascular lithotripsy. A) Severe in-stent restenosis in the diagonal branch (arrows). B) & C) Undilatable stenosis with 2.0×15 mm semi-compliant balloon (arrow). D) Longitudinal OCT reconstruction. E) & F) Severe in-stent restenosis in a region with two layers of stent. Calcific neoatherosclerosis is visible between the two layers of struts (*). G) Proximal region with one layer of stent also shows severe restenosis caused by calcific neoatherosclerosis (*). H) Underexpansion was treated with a 3.0×12 mm IVL balloon achieving adequate balloon expansion at 4 atm after 80 pulses. I) Longitudinal OCT reconstruction. J) & K) OCT cross-sections showing significant luminal gain and multiple calcium fractures after IVL (arrows). L) Treatment with a 3.0×25 mm paclitaxel-coated balloon with good expansion. M) Final angiographic result.
A 73-year-old male presenting with NSTEMI was referred for angiography. He had a previous history of percutaneous coronary intervention to a diagonal branch, initially in 2002 with a bare metal stent and later in 2010 with a drug-eluting stent for stent restenosis. The current angiogram showed a new diffuse and severe in-stent restenosis in the diagonal branch (% diameter stenosis [%DS] 81% and minimum luminal diameter [MLD] 0.29 mm). Optical coherence tomography (OCT) was performed to investigate the substrate of the restenosis demonstrating a severe underexpansion of the second stent implanted, caused by the presence of severe calcific neoatherosclerosis between the two layers of struts with a calcium arc >270º and calcium thickness >0.7 mm (minimum lumen area [MLA] 1.51 mm2) (Figure 1).
After semi-compliant balloon failure to dilate the stenosis at 20 atm, intravascular lithotripsy (IVL) was chosen in order to modify the calcific plaque located between the two stent layers and allow stent expansion. Eighty shocks were delivered with a 3.0×12 mm IVL balloon inflated at 4 atm, achieving an adequate balloon inflation, generating calcium fractures visible on OCT and obtaining luminal gain (MLA post IVL 1.80 mm2) (Figure 1). After IVL, high-pressure post-dilatation with a 3.0×12 mm non-compliant balloon at 28 atm was performed with good balloon expansion. Final OCT confirmed the luminal gain and the procedure was finished with a 3.0×25 mm paclitaxel-coated balloon with a good result (final MLA 2.85 mm², %DS 20%, MLD 1.92 mm, stent expansion index 77%) (Figure 1).
Calcific neoatherosclerosis is a cause of late stent failure and poses significant management challenges. In the present case, the initial restenosis was treated with new stent implantation without intracoronary imaging or adequate plaque preparation. The calcific neoatherosclerotic nature of the original restenosis prevented adequate expansion, probably the driver for the repeated stent failure. The location of the calcific tissue between the two stent layers makes the interaction of devices used for plaque preparation (such as rotational atherectomy and cutting balloons) difficult. IVL was useful to modify the calcium located between the two stents, allowing stent expansion.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.