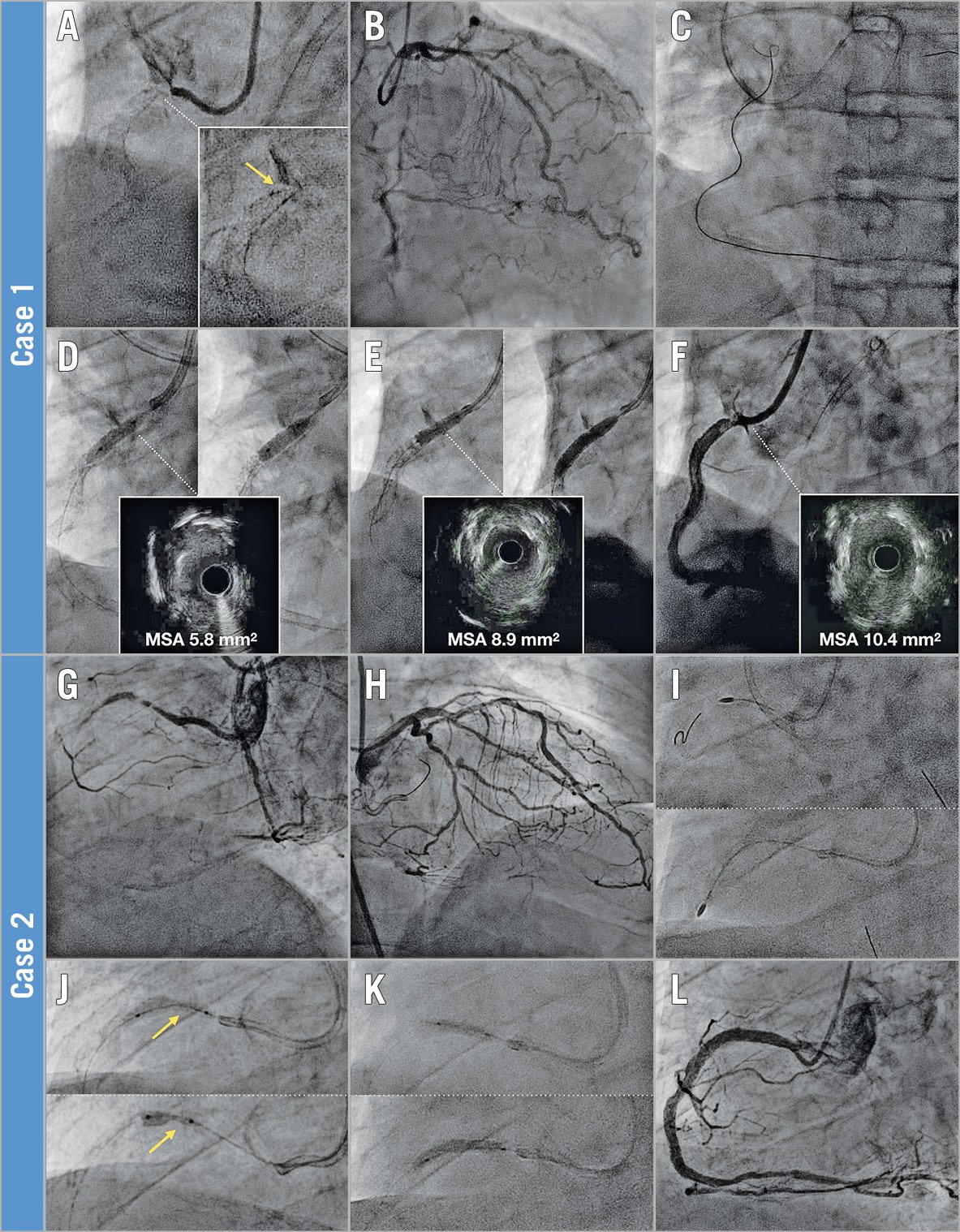
Figure 1. Intravascular lithotripsy in chronic total occlusion (CTO) percutaneous coronary intervention (PCI). A) Calcified ostial right coronary artery (RCA) CTO with recoiled stent (arrow) and (B) septal collaterals. C) Retrograde approach via septals and CTO crossing into the aorta. D) Incomplete expansion of 3.5 mm non-compliant (NC; left) and scoring (right) balloons. E) Intravascular lithotripsy (3.5 mm Shockwave; left), followed by balloon dilatation (4.0 mm NC; right), achieves better lesion preparation. F) Final result after implantation of two stents. G) Calcified mid RCA CTO with (H) septal collaterals. I) Rotational atherectomy (1.5 mm burr) on the proximal segment (top) and CTO (bottom). J) Underexpanded (arrow) 3.5 mm NC (top) and 3.0 mm scoring (bottom) balloons. K) Intravascular lithotripsy (3.5 mm Shockwave; top) and 3.5 mm NC balloon (bottom). L) Final result after implantation of three stents. MSA: minimal stent area
A 71-year-old man underwent ostial right coronary artery (RCA) in-stent chronic total occlusion (CTO) percutaneous coronary intervention (PCI). The occluded ostial stent appeared recoiled due to extensive calcification (Figure 1A). A retrograde approach via septal collaterals (Figure 1B) was chosen, and the guidewire crossed into the aorta (Figure 1C). After snaring and externalisation, the ostium was dilated with non-compliant (NC) and scoring balloons, but lesion preparation was suboptimal (Figure 1D). Therefore, intravascular lithotripsy (IVL) with a 3.5 mm Shockwave balloon (Shockwave Medical, Santa Clara, CA, USA; 70 pulses) was performed, which was followed by dilatation with a 4.0 mm NC balloon, achieving good expansion (Figure 1E). Two stents were then implanted, with a good result (Figure 1F).
A 62-year-old man underwent recanalisation of a mid RCA CTO (Figure 1G, Figure 1H). The lesion was crossed antegradely but, due to massive calcification, no balloon could be advanced. Rotational atherectomy (1.5 mm burr) was performed (Figure 1I). NC and scoring balloons could not expand adequately (Figure 1J). IVL (3.5 mm Shockwave) was then performed (20 pulses), followed by dilatation with a 3.5 mm NC balloon, which achieved optimal expansion (Figure 1K). Three stents were implanted, with a good result (Figure 1L).
Moderate/severe calcification is frequently found in CTOs. While atherectomy is effective in treating extensively calcified vessels, its use is not devoid of challenges and complications, particularly in difficult subsets such as CTOs (subintimal recanalisation, dissection planes, etc.)1.
IVL represents a novel alternative to achieve plaque modification in calcified lesions. Its ease of use, efficacy (sonic pressure waves are distributed uniformly across the inflated balloon, addressing calcium irrespective of its circumferential/eccentric location), and safety (IVL creates mechanical energy lasting <2 µs during low-pressure inflation, minimising vascular injury) make it particularly appealing to treat calcified CTOs. However, the high crossing profile (0.043”-0.046”) of the Shockwave catheter sometimes requires prior lesion preparation with rotational atherectomy to allow balloon delivery.
Conflict of interest statement
L. Azzalini received honoraria from Abbott Vascular, Guerbet, Terumo, and Sahajanand Medical Technologies; and research support from ACIST Medical Systems, Guerbet, and Terumo. The other authors have no conflicts of interest to declare.