Abstract
Aims: The aim of this study was to compare different radiation protection drapes in terms of radiation dose absorbed by operators during right or left transradial procedures.
Methods and results: Patients who underwent transradial coronary procedures were randomised initially into four groups: Group 1 (no drapes), Group 2 (drape on patient’s arm), Group 3 (pelvic drape), Group 4 (combined arm and pelvic drapes). Subsequently, each group was further randomised to right or left radial access. The primary endpoint was the operator radiation dose at the thorax. A total of 452 procedures were included. The use of drapes was associated with a lower radiation dose compared to no drapes (8.6 µSv [4.1-17.9] Group 1, 5.8 µSv [3.4-13] Group 2, 3.6 µSv [2.1-6.9] Group 3, 3.7 µSv [1.9-10.3] Group 4, p<0.001). Among radiation protection drapes groups the radiation dose was significantly lower in Groups 3 and 4 compared to Group 2 (p<0.008). Compared to Group 1, the dose in Group 2 was significantly lower only in right radial procedures (p<0.008) whereas in Groups 3 and 4 the dose was significantly lower in both radial accesses (p<0.008).
Conclusions: The use of radiation protection drapes during transradial coronary procedures is associated with a significantly lower radiation dose to operators, with the pelvic drape more effective than the use of a single arm drape.
Abbreviations
AK: air kerma
ANOVA: analysis of variance
DAP: dose area product
LRA: left radial access
PCI: percutaneous coronary intervention
RRA: right radial access
Introduction
The use of X-ray in interventional cardiology is associated with a potential risk of biological effects for both the patient and the operator1. In particular, the operators are exposed to a non-negligible risk of cataract and a possible increased risk of left brain cancer2,3. Consequently, interventional cardiologists should apply the “as low as reasonably achievable” principle when performing the procedure.
In recent years, all around the world there has been a significant increase in the use of the transradial approach for percutaneous coronary procedures due to a significant reduction in vascular complications and better patient comfort compared to the transfemoral access4. However, the transradial access seems to be associated with increased radiation exposure compared to the transfemoral approach5. Therefore, dedicated adjunctive radiation shields might be necessary to reduce the operators’ radiation exposure during transradial procedures.
Recently, different studies have shown the advantage of adjunctive radiation protection drapes in order to reduce operator radiation exposure during transradial procedures6-11. However, in these studies, different kinds and positioning of the drapes were used without direct comparisons. Moreover, the different effect of left radial access (LRA) vs. right radial access (RRA) was not evaluated.
The aim of our randomised study was to evaluate the radiation dose absorbed by interventional cardiologists performing transradial procedures using different adjunctive radiation protection drapes placed on the patient. Moreover, we also evaluated possible differences in the effect of these drapes using the RRA or the LRA.
Methods
STUDY DESIGN AND POPULATION
The RADIATION (RAdiation Dose In percutAneous coronary procedures through TransradIal apprOach using dedicated radiatioN shields) study (NCT 01839162) is a single-centre prospective, randomised, open-label, four-arm study designed to evaluate the radiation dose absorbed by operators during transradial percutaneous coronary procedures using different adjunctive radiation protection drapes.
All patients who underwent diagnostic or interventional percutaneous coronary procedures aged >18 years old were eligible for the study. Exclusion criteria were acute ST-elevation myocardial infarction, haemodynamic instability, previous coronary artery bypass, necessity of femoral approach or impossibility to perform transradial access, and lack of written informed consent. Moreover, after the enrolment, all patients requiring a switch of vascular access were excluded.
Before the procedure, all patients enrolled were initially randomised into four groups as follows: patients prepared without adjunctive radiation protection drapes (Group 1 – control group), patients prepared with an adjunctive radiation protection drape placed on the patient’s arm (Group 2 – arm drape), patients with an adjunctive drape on the pelvic region (Group 3 – pelvic drape), and finally patients prepared with combined pelvic and arm drapes (Group 4 – combined drape) (Figure 1, Figure 2). Allocation to one of the four groups was made by means of a computer-generated random sequence available on the Web (http://www.randomization.com) without stratification for clinical or procedural characteristics. Moreover, after allocation to the four groups, a second-order randomisation according to a 1:1 scheme in each group was performed in order to allocate patients to RRA or LRA (Figure 1). The randomisation list was managed by the nursing staff who informed the interventional cardiologist of the assigned approach just before the procedure.
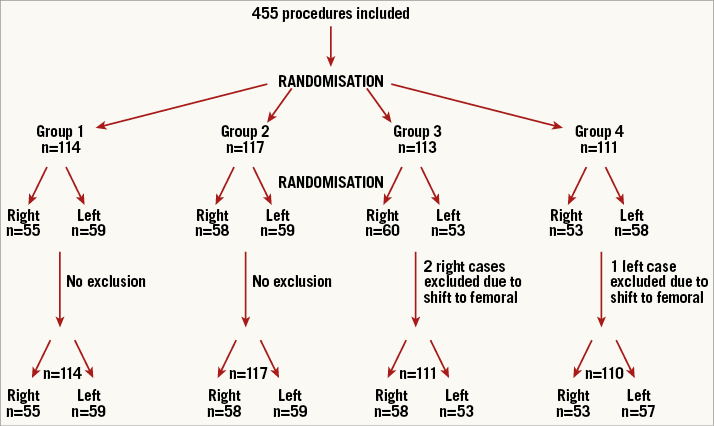
Figure 1. Flow chart. Description of the randomisation process.
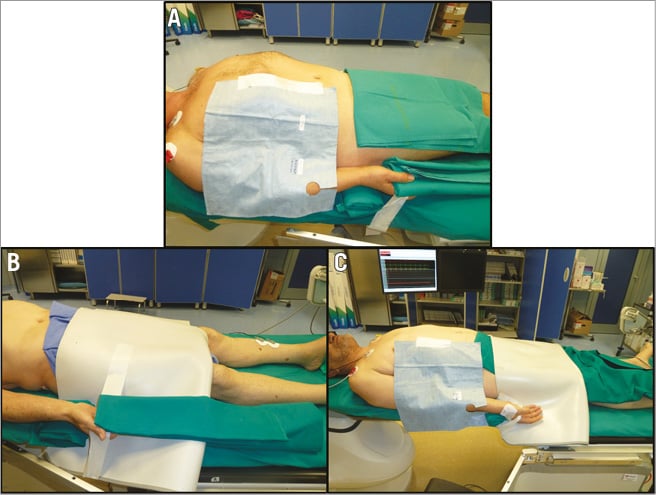
Figure 2. Patient preparation in right radial access. Positioning of the adjunctive protective drape at arm (A), pelvic (B) and combined arm and pelvic level (C).
The institutional ethics committee approved the protocol and all patients signed a written informed consent before participation.
TRANSRADIAL CORONARY CATHETERISATION
All procedures were performed using an angiographic “flat panel” system (IGS 520; GE Healthcare, Little Chalfont, Buckinghamshire, United Kingdom). The system was set using a field of view of 15 cm and a fluoroscopic and cine-acquisition speed of 15 frames/s. In all procedures, standard operator radioprotection was ensured using a lead apron, a thyroid lead collar, lower body X-ray curtain fixed on the angiographic table, suspended protective lead shield and leaded glasses.
In order to avoid a possible operator-related bias, only two interventional cardiologists (A. Sciahbasi and S. Rigattieri) performed all the procedures. The two cardiologists were high-volume transradial operators (>250 transradial procedures per year), of similar height (almost 185 cm), and performed the procedures using a similar position standing on the right of the table either for right or for left transradial procedures. The diagnostic procedures were generally performed using a standard sequence of three projections for the right coronary artery (left anterior oblique [LAO] 30°, LAO cranial 30°/20° and right anterior oblique [RAO] 30°) and five projections for the left coronary artery (LAO caudal 50°/20°, LAO cranial 50°/20°, RAO cranial 10°/30°, RAO caudal 30°/20° and anterior-posterior caudal 0°/20°).
PATIENT PREPARATION WITH ADDITIONAL RADIATION PROTECTION DRAPES
Two different additional radiation protection drapes (arm or pelvic drape) were used in this study: the arm drape was a barium bismuth drape (RADPAD®; Worldwide Innovations & Technologies Inc., Kansas City, MS, USA) positioned along the patient’s right side covering the right arm (Figure 2, Figure 3). In case of RRA, the drape was positioned superior and medial to the sheath insertion point, immediately below the suspended protective lead shield. On the other hand, the pelvic lead shield used was a home-made lead drape obtained from a lower body X-ray curtain, 0.5 mm lead equivalent (Kenex Electro Medical Ltd, Harlow, United Kingdom). This drape was positioned over the pelvic region of the patient (Figure 2, Figure 3). All of the adjunctive radiation protection drapes were placed during patient preparation and positioned underneath the sterile standard drape.
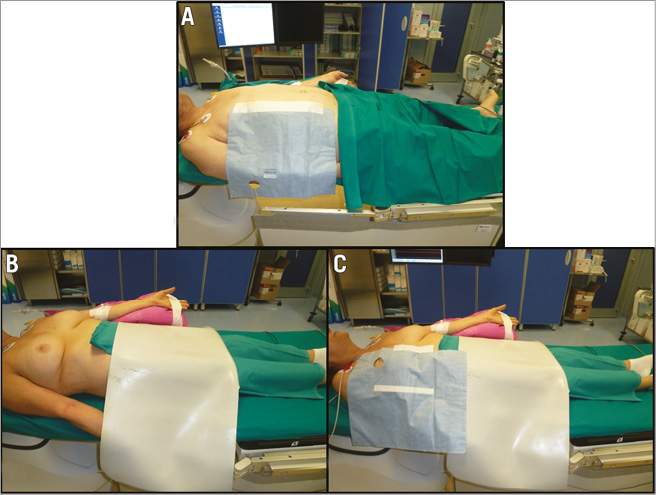
Figure 3. Patient preparation in left radial access. Positioning of the adjunctive protective drape at arm (A), pelvic (B) and combined arm and pelvic level (C).
RADIATION MEASUREMENT
Radiation measures collected were fluoroscopy time, air kerma (AK) and the dose area product (DAP). The AK is the adsorbed dose in air at a defined distance from the X-ray tube’s focal spot, which is generally 15 cm from the isocentre. The DAP is the product of the AK and the cross-sectional area of the X-ray field for all segments of the procedure. These parameters were measured using specially designed ionisation chambers mounted at the collimator system and elaborated by a dedicated software (Innova Dose Report; GE Healthcare).
Operator radiation exposure was measured using wearable personal electronic dosimeters placed at the left wrist (RADOS RAD-60; LAURUS Systems Inc., Ellicott City, MD, USA), at the thorax (outside the pocket of the lead apron) and at head level (in the middle front) (PM1610; Polimaster, Vienna, Austria). These dosimeters have a Geiger-Mueller detector dedicated for X-ray with an energy range of detection between 0.001 μSv and 12.0 Sv. The radiation and operator measures were recorded at the beginning and the end of each procedure. For those patients in whom a percutaneous coronary intervention (PCI) was performed after the diagnostic procedure, the measures of fluoroscopy time, DAP, AK and dose of the wearable dosimeters were reset after the end of the diagnostic procedure and restarted at the beginning of the PCI. All the radiological measures were recorded by the nursing staff in a dedicated electronic registry. The collection of these data was not blinded, as the operator can have the possibility of seeing the dose on the dosimeter display at the end of the procedure.
To take into account possible differences in patient radiation dose affecting the operator exposure, the DAP-normalised operator dose was also calculated.
ENDPOINT OF THE STUDY
The primary endpoint of the study was the operator radiation dose at the thorax in the four groups. We also pre-specified a secondary endpoint, defined as the operator radiation at the left wrist and head. Finally, we also pre-specified an analysis comparing the operator radiation dose according to the side of vascular access (RRA vs. LRA).
STATISTICAL ANALYSIS
The sample size was estimated on the primary endpoint according to data of a previous study performed using dedicated drapes placed at pelvic level8 that showed a mean operator dose of 21±14 µSv without drapes and a 50% reduction with the drapes. Using the one-way analysis of variance (ANOVA), to detect a 30% reduction of the radiation dose with the radiation protection drapes with a power of 80% and an alpha error of 0.05, a total of 110 procedures for each group was required.
Continuous variables are reported as mean and standard deviation for variables normally distributed and as median with interquartile range for those not normally distributed and were compared using ANOVA or the Kruskal-Wallis test as appropriate. Post hoc comparisons were performed using the Bonferroni correction. In this last case, since the between-group comparisons were six, the level of statistical significance was set at <0.0083. Normal distribution of each variable was assessed using the Kolmogorov-Smirnov test.
Categorical variables were compared by Pearson’s chi-square test or with Fisher’s exact test, as appropriate. Post hoc analysis using a Pearson’s chi-square test 2×2 with the Bonferroni correction was used for intergroup comparisons.
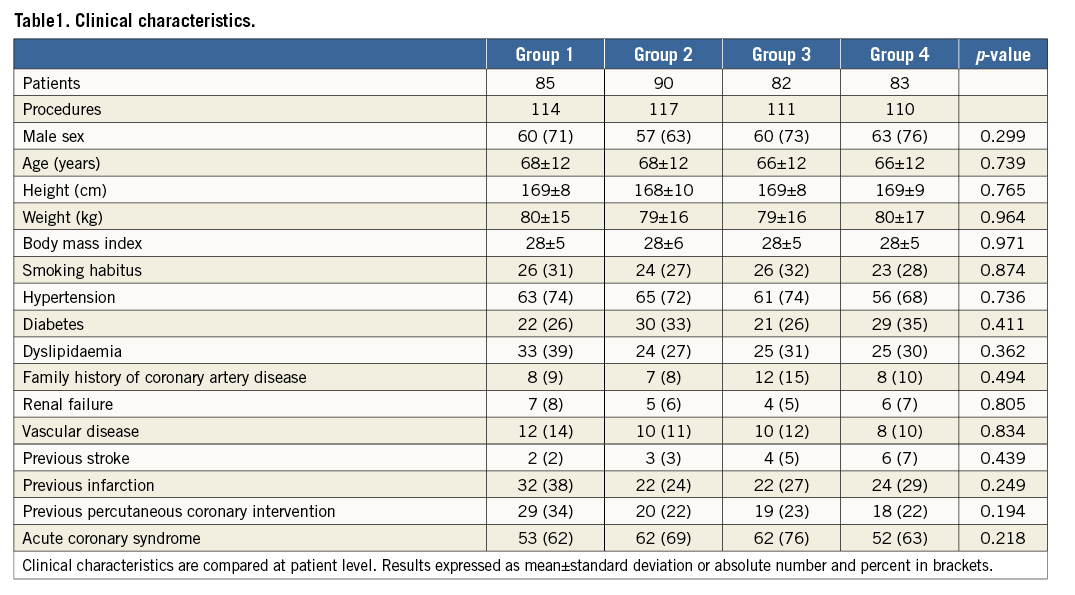
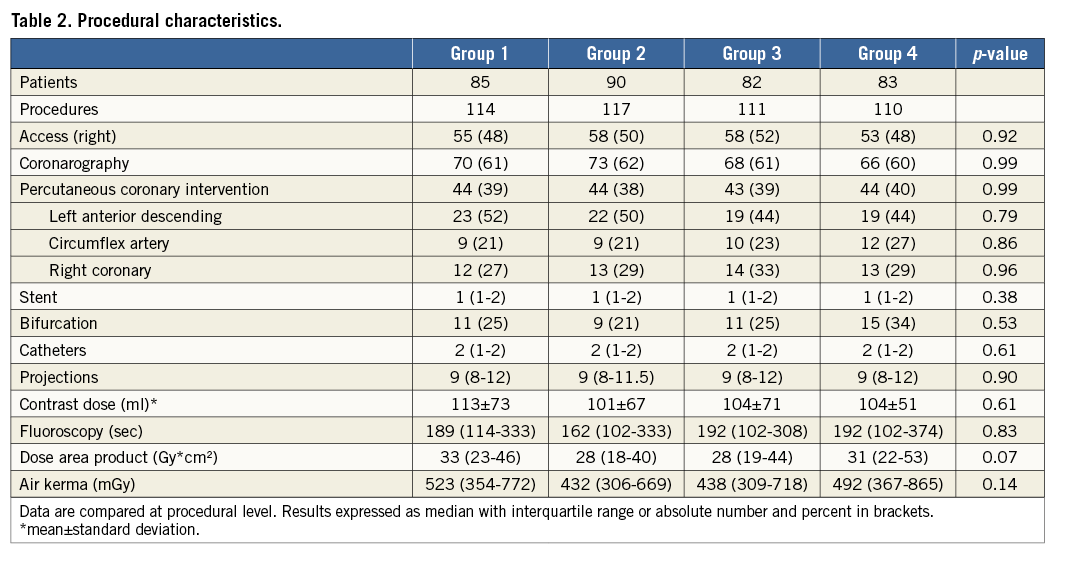
The clinical characteristics (Table 1) were analysed at patient level, whereas procedural characteristics and dosimetric data were analysed at procedural level. All analyses were performed with SPSS software, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 343 patients were enrolled and 455 procedures were performed; three procedures in three patients (two cases with RRA in Group 3 and one case with LRA in Group 4) were excluded after enrolment due to a procedural switch to the femoral access (globally 99% procedural success). The reasons for the switch were radial puncture failure (two cases) and severe radial tortuosity (one case). Consequently, the final sample size was 452 procedures in 340 patients. These procedures were divided as follows: 114 procedures in Group 1, 117 in Group 2, 111 in Group 3, and 110 in Group 4 (Figure 1).
PROCEDURAL AND CLINICAL CHARACTERISTICS
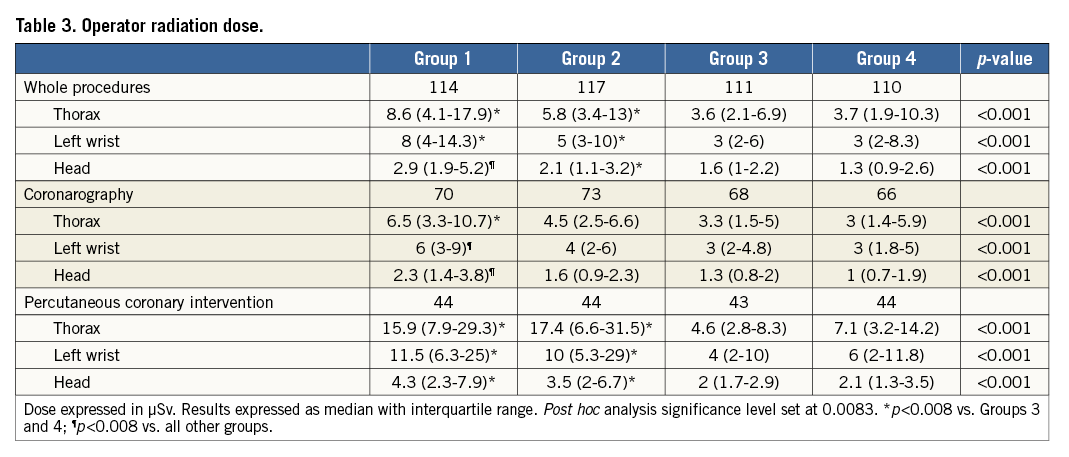
Clinical and procedural characteristics are summarised in Table 1 and Table 2. There were no significant differences among groups in terms of anthropometric data, cardiovascular risk factors or procedural data. There were no significant differences in fluoroscopy times, DAP or AK (Table 2), even if Group 1 and Group 4 showed a trend to higher DAP and AK values.
PRIMARY ENDPOINT
There was a statistically significant difference in thorax radiation dose among the four groups (p<0.0001) (Figure 4, Table 3). In particular, in all groups with adjunctive drapes there was a lower radiation dose compared to Group 1 (Figure 4) that was statistically significant in Groups 3 and 4 but did not reach the pre-specified criteria for significance in Group 2. Moreover, in the three groups with adjunctive drapes, the use of the pelvic drape was associated with a significantly lower radiation dose compared to the arm drape (p<0.001); the combined use of the pelvic and arm drapes was not associated with a significant advantage over the pelvic drape alone (p=0.302) (Figure 4).
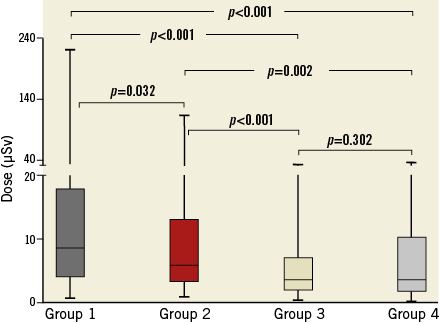
Figure 4. Primary endpoint. Radiation dose absorbed by operators at the thorax in the four groups of patients. Results are expressed as median, interquartile range and maximum and minimum values.
SECONDARY ENDPOINTS
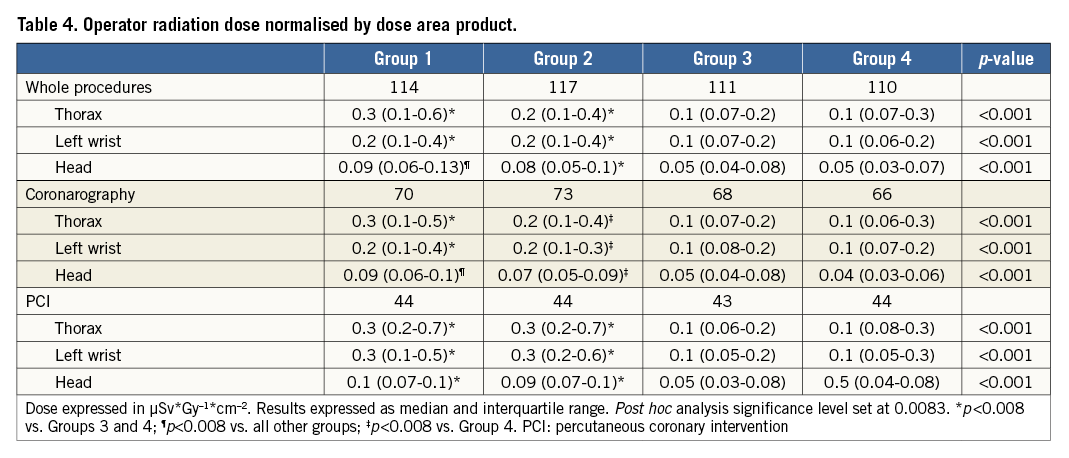
Table 3 reports the head and left wrist radiation dose. At head level in all groups with drapes, there was a lower radiation dose compared to Group 1 (p<0.0001), whereas at left wrist only in Groups 3 and 4 there was a significantly lower dose compared to Group 1. Moreover, Group 3 and Group 4 showed a significantly lower radiation dose for all the dosimeters compared to Group 2 both at head and left wrist level. When we split the analysis evaluating diagnostic and interventional procedures independently, the use of the arm drape was effective only in case of diagnostic procedure, whereas there was no effect during PCI (Table 3). In contrast, the use of the pelvic drape was effective both in diagnostic and in interventional procedures. The results of data normalised by DAP were similar compared to standard analysis (Table 4).
When operator dose was analysed separately in the two cardiologists involved, the effect of the adjunctive drapes was observed in both the operators.
LEFT VERSUS RIGHT ACCESS
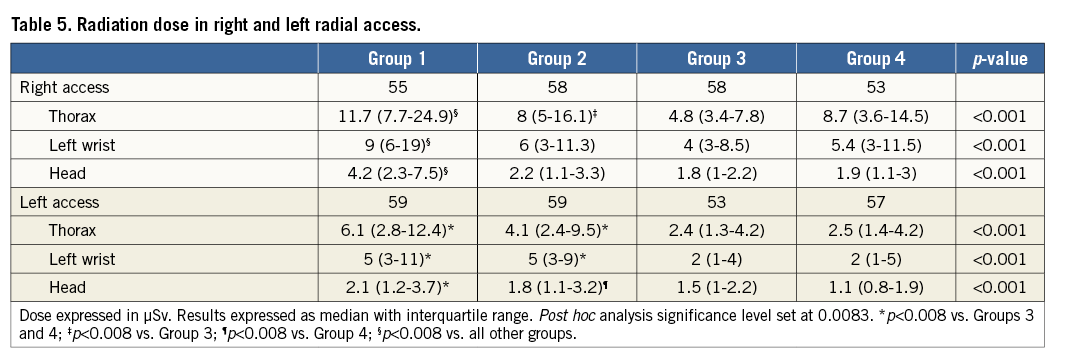
Comparing the RRA with the LRA in the whole population, we observed a significantly lower radiation dose for the LRA at the thorax (3.2 [1.9-6.5] µSv and 7.8 [4.3-15.4] µSv, respectively, p<0.0001), at left wrist (3 [2-7] µSv and 7 [3-12] µSv, respectively, p<0.0001) and at head level (1.6 [1-2.3] µSv and 2.2 [1.2-3.8] µSv, respectively, p<0.0001) (Figure 5). When we analysed the effect of the adjunctive drapes, the pelvic drape was effective in both vascular accesses, whereas the arm drape was effective only in the RRA (Table 5).
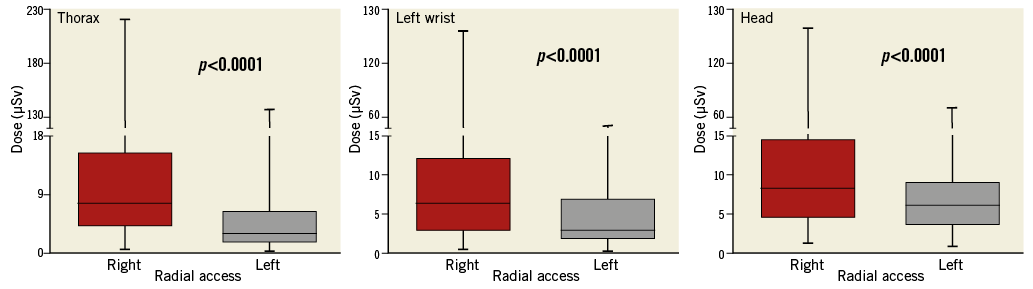
Figure 5. Right versus left radial effect. Radiation dose absorbed by operators at the thorax, left wrist and head comparing the right versus the left radial access. Results are expressed as median, interquartile range and maximum and minimum values.
Discussion
In our study we investigated the effect of different radiation protection drapes on operator radiation exposure during transradial percutaneous coronary procedures. The results of our randomised study underline three important messages:
– The use of adjunctive radiation protection drapes during percutaneous transradial coronary procedures is associated with a significantly lower radiation dose compared to standard preparation of the patient.
– The use of a pelvic drape (alone or combined with an arm drape) is more effective compared to the isolated use of an arm drape.
– The LRA is associated with a significantly lower operator radiation dose compared to the RRA, even with the use of adjunctive radiation protection drapes.
Radiation safety should be a priority in the cardiac catheterisation laboratory considering the possible increased radiation risk for the patient and for the operator2,3. In this context, some studies6-11 have shown a possible reduction of the operator radiation dose with the use of adjunctive radiation protection drapes during transradial percutaneous coronary procedures. However, in our study there are some important differences compared to previous ones. First of all, in some of these studies only a diagnostic procedure was performed and, in particular, the arm drape was tested only in this patient setting7. Moreover, in most, the operator used the RRA and data on the LRA are poor. Finally, no study performed a direct comparison of the position of the drapes (arm versus pelvis). In our study, we confirmed the effective role of the adjunctive radiation protection drapes during either diagnostic or interventional procedures. Moreover, we observed that the pelvic compared to the arm drape was more effective in reducing the operator radiation dose. The possible explanation of the higher efficacy of the pelvic drape lies in the significant amounts of scatter radiation from the pelvic bones that cannot be shielded using an isolated arm drape but can be significantly reduced by a shield covering the patient’s pelvis and thighs.
The advantage of our pelvic drape is also in economic terms as it is associated with no adjunctive procedural costs. Actually, according to our results, the use of the adjunctive pelvic drape has become the standard of care for most of our transradial procedures.
The LRA has some important advantages over the RRA in terms of lower fluoroscopy times12 and lower rate of subclavian or radial tortuosity13. However, many operators are concerned about a possible increased higher operator radiation exposure compared to the RRA, as has recently been observed14. In this context, our study is reassuring for operators who prefer the use of LRA. Indeed, we observed that, compared to the RRA, the LRA is associated with a significantly lower radiation dose for the operator at the left wrist, head and thorax, even with the use of adjunctive radiation protection drapes. The reasons for the lower radiation dose associated with LRA are several. First of all, in RRA procedures the suspended protective lead shield cannot be positioned close to the operator but should be placed proximal to the patient in order to permit vascular access. This positioning creates a gap between the suspended protective lead shield and the operator, increasing the radiation exposure. By contrast, in the LRA the suspended protective lead shield can be adequately positioned in order to avoid this gap. Another reason is the position taken by the operator during the procedures. In RRA, in particular in left projections (that are associated with the highest radiation doses), the body and the arm of operators are closer to the X-ray tube compared to LRA with the operator bending over the patient and far from the tube. However, we cannot exclude that the LRA might be associated with higher radiation dose absorbed in different parts of the operator’s body, as documented in a previous bench test15. Our study confirms the data of almost all previous studies that compared the LRA with the RRA in terms of operator radiation dose16-19, except the results observed in the REVERE trial14. Probably operator anthropometric data (height and weight) and the arrangement of the cathlab in terms of protective shields might be responsible for the different data obtained. The results of the RAD-MATRIX study20 might contribute to a better understanding of the RRA versus LRA effect in terms of radiation dose absorbed by the operators.
Limitations
Our study has some limitations. First of all, the study lacks a “sham” drape in Group 1. Consequently, we cannot exclude that the presence of the drapes made the operators more aware of radiation safety compared to procedures performed without drapes, increasing the effect of radiation dose reduction obtained with the drapes. Another limitation is the single-centre design of the study: we cannot exclude that, in different centres with a different arrangement of the cathlab, different results can be obtained. Moreover, only two tall and expert operators were involved in the study and consequently our results might not be applicable to shorter or less experienced operators. Besides, the pelvic and arm drapes are composed of different materials and we cannot exclude a possible different radiation attenuation power in favour of the pelvic drape. In our study, we regularly used a medium rate of fluoroscopy (15 fps), even if previous studies showed a significant reduction of operator radiation dose using a low rate of fluoroscopy (7.5 fps)21. We cannot exclude that the effectiveness of the adjunctive protective drapes could be reduced using a low rate of fluoroscopy. The sample size was estimated according to the primary endpoint. Consequently, the analysis of secondary endpoints might not have had enough power to detect differences among groups. Furthermore, despite significant differences among groups in terms of operator radiation dose there is a considerable overlap of data. Finally, we did not directly measure the patients’ radiation exposure and we cannot exclude a possible increased radiation dose in patients, as previously shown10. In that study, the dose to the patient was almost double with the adjunctive drapes but very low in absolute terms.
Conclusions
In our study, the use of adjunctive radiation protection drapes during transradial percutaneous coronary procedures was associated with a significantly lower radiation dose to operators. However, the use of a pelvic drape is more effective and less expensive than the use of a single arm drape.
| Impact on daily practice Operator radiation exposure during transradial percutaneous coronary procedures can be reduced using different radiation protection drapes placed on the patient’s arm or at pelvic level. However, the use of a pelvic drape is more effective than a single arm drape. Probably the use of a pelvic drape should be the standard equipment in patient preparation during transradial coronary procedures in order to reduce the operator radiation exposure significantly. |
Conflict of interest statement
The authors have no conflicts of interest to declare.