Abstract
Aims: We investigated the relation between myocardial blush grade reserve (MBGreserve) and fractional flow reserve (FFR) measures. FFR is a marker of inducible myocardial ischaemia, which could guide percutaneous coronary intervention (PCI) and stent placement. However, it requires a pressure wire and is associated with additional costs and potential hazards. The aim of our study was to investigate the ability of MBG for the evaluation of functional significance in intermediate coronary lesions during pharmacologic hyperaemia.
Methods and results: Fifty-six patients who underwent routine cardiac catheterisation for known or suspected coronary artery disease (CAD) and clinically indicated FFR measures in at least one coronary vessel were analysed. MBGreserve was assessed at baseline and during pharmacologic hyperaemia. Video densitometric parameters were then calculated by the ratio of maximal density (Gmax) and the time to reach maximum density (Tmax). Gmax/Tmax during hyperaemia divided by Gmax/Tmax at baseline provided the MBGreserve. A significant association was observed between MBGreserve and FFR. A cut-off value of MBGreserve=2.1 demonstrated sensitivity of 80% and specificity of 96% for the prediction of abnormal FFR of ≤0.8. MBGreserve increased in coronary territories that underwent PCI, reaching similarly high values compared to those observed in FFR-negative lesions.
Conclusions: Quantitative MBGreserve is closely related to FFR measures and may obviate the need for pressure wire measurements in the interests of patient safety, time and costs.
Introduction
Assessment of fractional flow reserve (FFR) represents the current standard reference technique for the evaluation of functional significance in anatomically intermediate coronary lesions1. In the recent multicentre FAME trial, routine measurement of FFR in patients who underwent interventional treatment with drug-eluting stents was shown to reduce the rate of cardiac events significantly during two years of follow-up compared to patients who underwent standard angiography-guided PCI2-4. However, FFR requires the introduction of a flow wire into the coronary vessel of interest, which is associated with potential vessel wall injury and additional costs5.
We and others have previously demonstrated the ability of quantitative myocardial blush grade (MBG) to provide insight into the microvascular integrity of the myocardium in patients with acute coronary syndromes and in cardiac transplant recipients6-8. This method does not require the insertion of a catheter or wire into the periphery of the coronary vessel and is therefore less risky and potentially more time- and cost-effective.
The aim of our study was to investigate the ability of MBG for the evaluation of functional significance in intermediate coronary lesions during pharmacologic hyperaemia.
Methods
STUDY POPULATION
Our study patient group consisted of consecutive patients who underwent clinically indicated coronary angiography for suspected or known coronary artery disease (CAD) between April and September 2012. During this time period, 56 patients exhibited intermediate (40-70%) diameter stenosis and subsequently underwent clinically indicated FFR measures. A corresponding flow chart including exclusion criteria is depicted in Appendix Figure 1. Traditional risk factors including arterial hypertension, hyperlipidaemia, current or prior smoking, diabetes mellitus, family history of CAD, prior infarction and revascularisation and increased body mass index >30 kg/m² were recorded. History of CAD encompassed angiographically significant CAD (≥50% stenosis), prior infarction and revascularisation procedures. Informed consent was obtained from each patient and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the institution’s human research committee.
FRACTIONAL FLOW RESERVE AND MYOCARDIAL BLUSH GRADE
FFR measurements were performed in coronary arteries with intermediate lesions (40-70% diameter stenosis by visual estimation) as clinically indicated by the operating interventional cardiologist. Measures were performed using the RadiAnalyzer™ Xpress (St. Jude Medical, St. Paul, MN, USA) and a coronary pressure wire (Certus™; St. Jude Medical). After calibration and equalisation, the pressure wire was carefully advanced in the distal part of the vessel of interest. Hyperaemia was subsequently induced by intravenous administration of 140 µg/kg/min adenosine and, after reaching a steady state (~3 minutes), a wire pullback was performed to the position of the guiding catheter in order to correlate changes in the FFR during pullback with coronary anatomy and to check the equalising position, which should always be equal to 1.0, i.e., to exclude potential drift9,10. FFR values of ≤0.80 were considered as indicative of myocardial ischaemia4.
For the assessment of myocardial blush, predefined projections were used, as described previously6. A frame rate of 12.5/s was used for the acquisition of all MBG data. Choosing these projections, we sought to assess the perfusion territory of the corresponding coronary artery and simultaneously to avoid superpositioning of the other coronary territories11. Contrast injections were performed by manual injection of ~8 ml contrast over ~1 s and using 6 Fr guiding catheters for the left and right coronary arteries.
QUANTIFICATION OF MYOCARDIAL BLUSH GRADE
A computer-assisted procedure which was applied in digital subtraction angiography images was used to quantify myocardial tissue level perfusion. The technical details of this procedure have been described elsewhere6,12, whereas an image series for MBG intensity rise assessment after background subtraction is provided in Appendix Figure 2. Briefly, the time course of MBG intensity rise was analysed using ECG-gated angiograms. Regions of interest were placed in the distal perfusion territory of the corresponding coronary vessel to estimate the plateau of mean grey level pixel intensity (Gmax measured on a standard greyscale of 0-255) and the time to maximal intensity rise (Tmax measured in seconds). Subsequently, the ratio Gmax/Tmax was computed. Furthermore, based on the temporal distribution of myocardial blush in epicardial vessels, arterioles and capillaries, parametric quantification was applied according to the timing of maximal grey values. Frames had to be long enough to allow filling of the venous coronary system, and images were acquired during breath hold to avoid potential artefacts due to diaphragmal shift.
Acquisitions were performed in identical projections at baseline and during pharmacologic hyperaemia with adenosine, administered during FFR. For each coronary lesion, the myocardial blush reserve was calculated as follows:
Myocardial blush reserve (MBGreserve)=
![]()
A schematic illustration of a region of interest (red coloured areas) placed in the LAD perfusion territory during blush grade acquisitions and the corresponding curves at baseline and during maximal hyperaemia are shown in Figure 1A and Figure 1B, respectively.
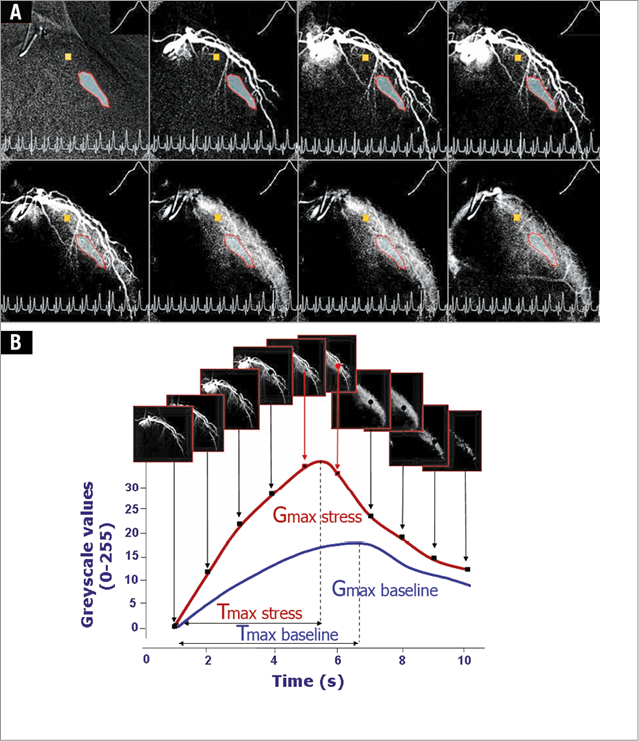
Figure 1. Image acquisition for the computer-assisted algorithm with digital subtraction angiography. In a region of interest (red-rimmed), grey level intensity rise at baseline and during adenosine infusion (A). Time replenishment kinetics of the myocardial blush grade at baseline and during hyperaemia for the calculation of MBGreserve (B).
STATISTICAL ANALYSIS
Continuous variables were expressed as mean±standard deviation for parametric or as median with interquartile range (IQR) for non-parametric variables. For continuous variables, differences between groups were compared using repeated measures analysis of variance with Bonferroni correction for multiple comparisons. Categorical variables were expressed as counts or percentages. Linear regression was used to assess the relation between myocardial blush and FFR. Receiver operating characteristics (ROC) analysis was used to define the optimal cut-off values for myocardial blush to predict functional significance as assessed by the reference standard FFR. For the assessment of the optimal cut-off value, the Youden index J was used13,14. For all analyses, a p-value of <0.05 was regarded as statistically significant. All tests were two-sided. Intra-observer variabilities for myocardial blush reserve were assessed by repeated analysis of all patients and by selecting different ROIs in each vessel of interest by the two independent readers. Readings were separated by eight weeks to minimise recall bias. The MedCalc 13.2 (MedCalc Software, Mariakerke, Belgium) computer programme was used throughout.
Results
BASELINE CHARACTERISTICS
The demographic, laboratory and angiographic characteristics of our patient cohort are illustrated in Table 1. FFR was performed in 66 coronary vessels of 56 patients. Six vessels (9%) included more than one coronary lesion. Lesions were located in the LAD (n=17 [26%]), LCX (n=26 [39%]) and RCA (n=20 [30%]). Two cases (3%) involved the first diagonal branch and one case (1.5%) involved the first marginal branch. Calculation of myocardial blush was feasible in all cases, independent of the location of the lesions. Twenty patients (36%) had single-vessel CAD, whereas 36 (64%) had multivessel CAD.
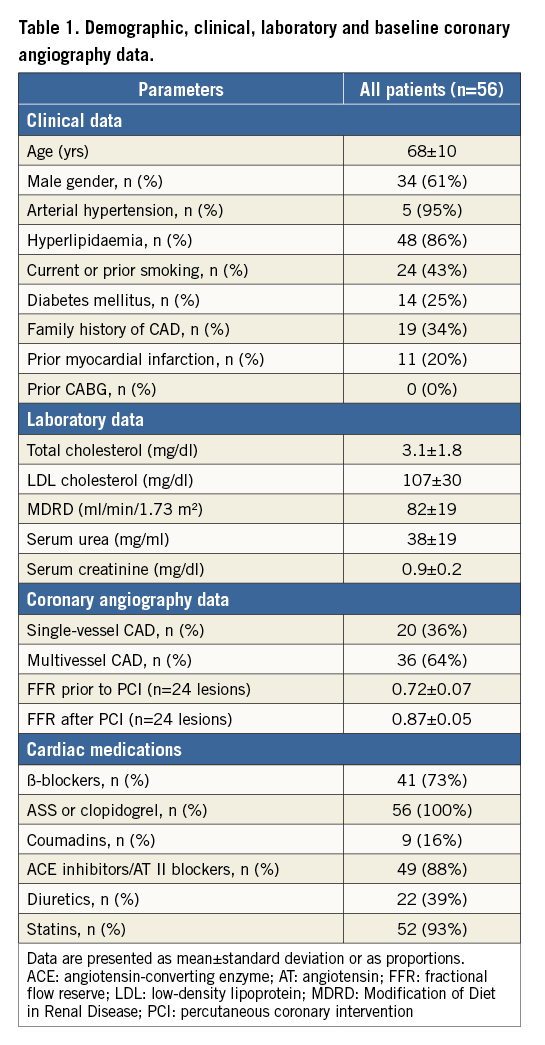
In 42 cases, FFR was >0.80, deferring PCI. On the other hand, in 24 lesions FFR was ≤0.80, so that PCI was performed. FFR was repeated in all lesions after PCI and stent placement.
ASSOCIATIONS BETWEEN FFR AND MYOCARDIAL BLUSH RESERVE (MBGRESERVE) PRIOR TO PCI
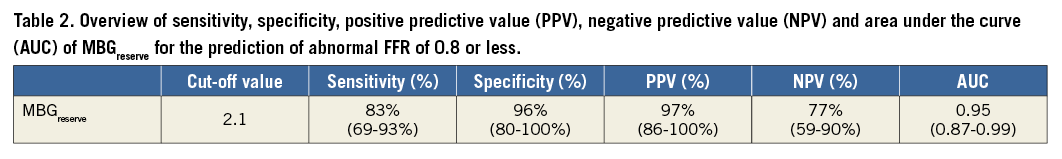
A significant association was observed between FFR and MBGreserve (r=0.70, 95% CI: 0.55-0.80, p<0.001) (Figure 2A). Using ROC analysis, a cut-off value of MBGreserve ≥2.1 demonstrated sensitivity of 83% (95% CI: 69-93%), specificity of 96% (95% CI: 80-100%), positive predictive value of 97% (95% CI: 86-100%), negative predictive value of 77% (95% CI; 59-90%) and AUC of 0.95 (95% CI: 0.87-0.99) for the prediction of normal FFR >0.8 (Figure 2B, Table 2).
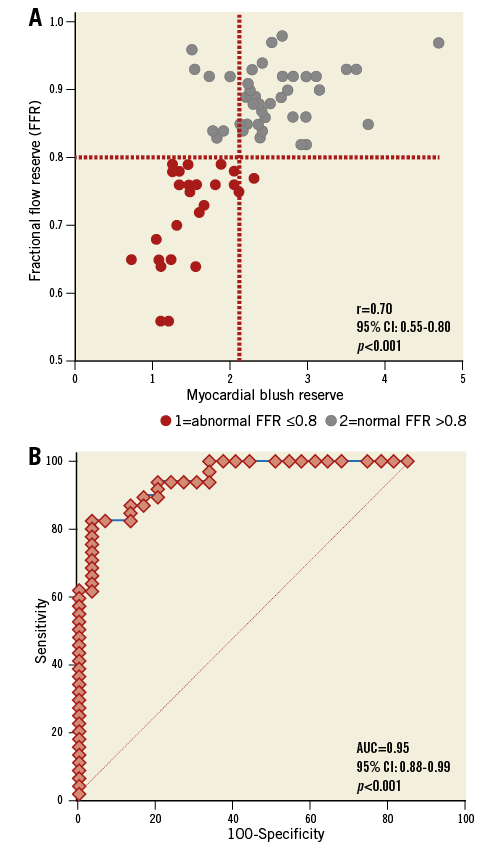
Figure 2. Statistical association, sensitivity and specificity. Significant association between FFR and MBGreserve (r=0.70, 95% CI: 0.55-0.80, p<0.001) (A) and ROC analysis showing the high precision of MBGreserve for the prediction of normal FFR >0.8 (AUC=0.95, 95% CI: 0.88-0.99, p<0.001) (B). FFR and MBG measures after PCI were excluded from analysis.
FFR and MBGreserve were similarly distributed within the three major coronary territories (Appendix Figure 3). The association between FFR and MBGreserve was slightly higher in patients with single-vessel versus multivessel CAD (r=0.76, 95% CI: 0.49-0.90 versus r=0.69, 95% CI: 0.51-0.82), without however reaching statistical significance by z-statistics (z=-0.52, p=ns).
INCREASE OF FFR AND MBGRESERVE AFTER PCI AND STENT PLACEMENT
FFR significantly increased from 0.72±0.07 before PCI to 0.87±0.05 after PCI (n=24, p<0.001), thus reaching values such as those observed in FFR-negative vessels, 0.89±0.04 (p=NS compared to post-PCI lesions) (Figure 3A). Similarly, MBGreserve increased in coronary territories that underwent PCI, reaching similarly high values compared to those observed in FFR-negative lesions (Figure 3B).
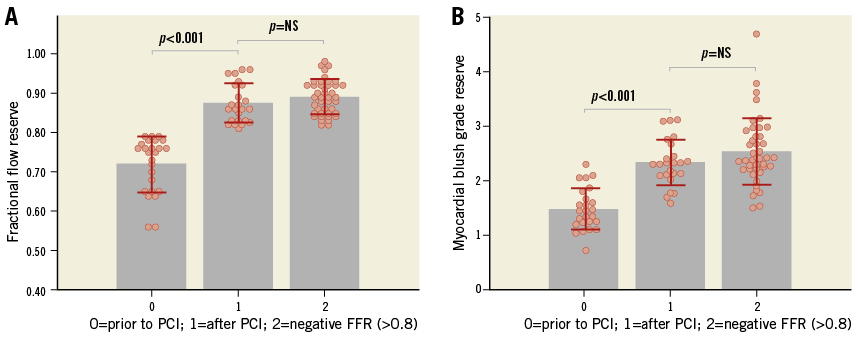
Figure 3. Peri-interventional measures. FFR (A) and MBGreserve (B) are both significantly increased after PCI, reaching similar levels compared to FFR-negative vessels.
Comparing FFR and MBGreserve before and after PCI and stent placement, the relative increase of FFR was related to that of MBGreserve (Figure 4).
An example of a patient with abnormal FFR of 0.64 in the LAD and reduced MBGreserve of 1.1 is demonstrated in Figure 5A at baseline and Figure 5B during hyperaemia. In Moving image 1, the myocardial blush in the distal septal branches can be appreciated during pharmacologic hyperaemia prior to PCI. Note the presence of moderate blush around the distal septal branches. After PCI and placement of two stents, adenosine administration was repeated, exhibiting FFR of 0.86 and markedly increased MBGreserve of 4.12. Increased myocardial blush can be appreciated in Figure 5C and around the mid and septal branches in Moving image 2 during pharmacological hyperaemia after PCI.
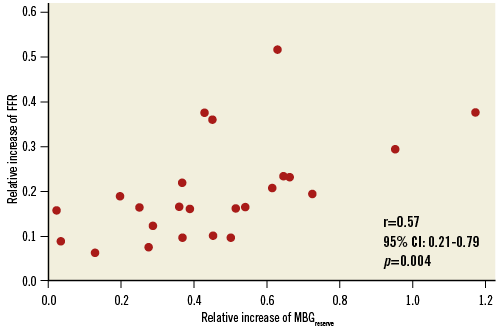
Figure 4. The relative increase of FFR was related to that of MBGreserve after PCI and stent placement (r=0.57, 95% CI: 0.21-0.79, p=0.004).
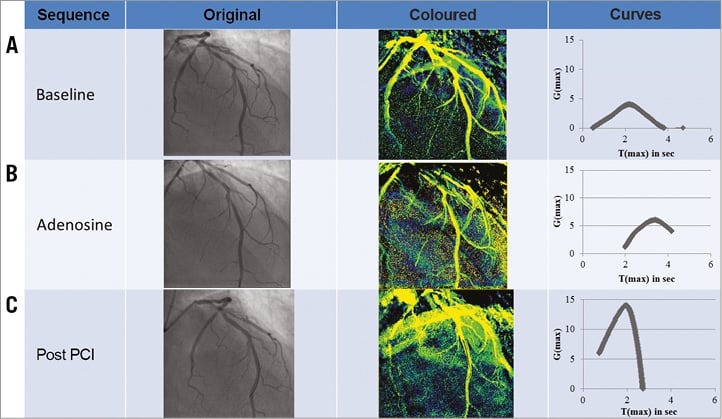
Figure 5. Patient example. Representative case with positive FFR and reduced MBGreserve prior to percutaneous coronary intervention (A & B). Both FFR and MBGreserve subsequently increased after successful revascularisation (C).
INTER- AND INTRA-OBSERVER VARIABILITY
Assessment of Gmax/Tmax at baseline, Gmax/Tmax during adenosine infusion and MBGreserve was highly reproducible with intra- and inter-observer variabilities of 6.5% and 8.2%, 7.6% and 12.1%, and 10.7% and 11.0%, respectively.
Discussion
Our main findings are that:
1. MBG can be assessed during pharmacologic hyperaemia and routine cardiac catheterisation with high reproducibility.
2. MBGreserve is related to FFR. An equal or more than 2.1-fold increase of MBG during adenosine was highly predictive of a normal FFR >0.8.
If this close relation holds true in larger studies, MBGreserve may be an alternative to FFR because of procedural costs and patient safety.
CURRENT EVIDENCE REGARDING PRESSURE WIRE-BASED FFR
FFR is a surrogate marker of inducible regional myocardial ischaemia, which can be measured during routine cardiac catheterisation15. Several large-scale randomised clinical trials have demonstrated that FFR can be used to guide interventional procedures, significantly improving patient outcomes compared to visually guided PCI2-4,16. In addition, FFR-guided PCI was recently shown to improve outcome of patients with stable CAD compared to medical therapy alone within the randomised FAME 2 trial17. Therefore, FFR has in the meantime emerged as a gold standard for the assessment of the functional significance of CAD during routine cardiac catheterisation.
Although FFR measurement is a safe procedure, there is still a low risk of injuring vessels by wire manipulation. Thus, in the recent Nordic-Baltic bifurcation substudy, FFR measurements could not be obtained in 10% of the cases due to side branch dissection by the pressure wire or wiring failure with complex anatomy18. Similarly, FFR assessment was reported not to be feasible in up to 13% of side branches in bifurcation19. In addition, such measures are associated with additional costs. Among other factors, this may contribute to the low adoption rate of FFR measurement in real-world clinical practice, as <10% of intermediate stenoses are currently evaluated by FFR, as reported in the recent US CathPCI Registry20. Thus, the systematic use of FFR seems to be difficult to implement in clinical practice, and decisions during interventions are still most often based on direct visual estimation of coronary stenosis by angiography21. Conversely, assessment of MBG in side branches would be as feasible as measuring myocardial blush in the distal part of main branches, without requiring manipulation with a guidewire. However, caution is needed with MBG measures in such distal diagonal, marginal or septal branches due to superimposition with nearby territories, which may be associated with potential difficulties in distinguishing the territory of interest.
COMPUTATION OF VIRTUAL FFR-BASED 3D CORONARY ANGIOGRAPHY AND CARDIAC CT
Based on computational fluid dynamics, three-dimensional quantitative coronary angiography (QCA) can provide a virtual haemodynamic assessment model using only routine angiography without requiring invasive physiology measurements22 and even without requiring hyperaemia induction23. Cardiac computed tomography angiography (CCTA) on the other hand may represent a non-invasive alternative method with high diagnostic performance for the detection of functionally relevant coronary lesions. An overview of current virtual FFR studies, using pressure-wire FFR as the reference standard, can be seen in Table 3 22-29. Our present results are provided at the bottom of Table 3 for comparison.
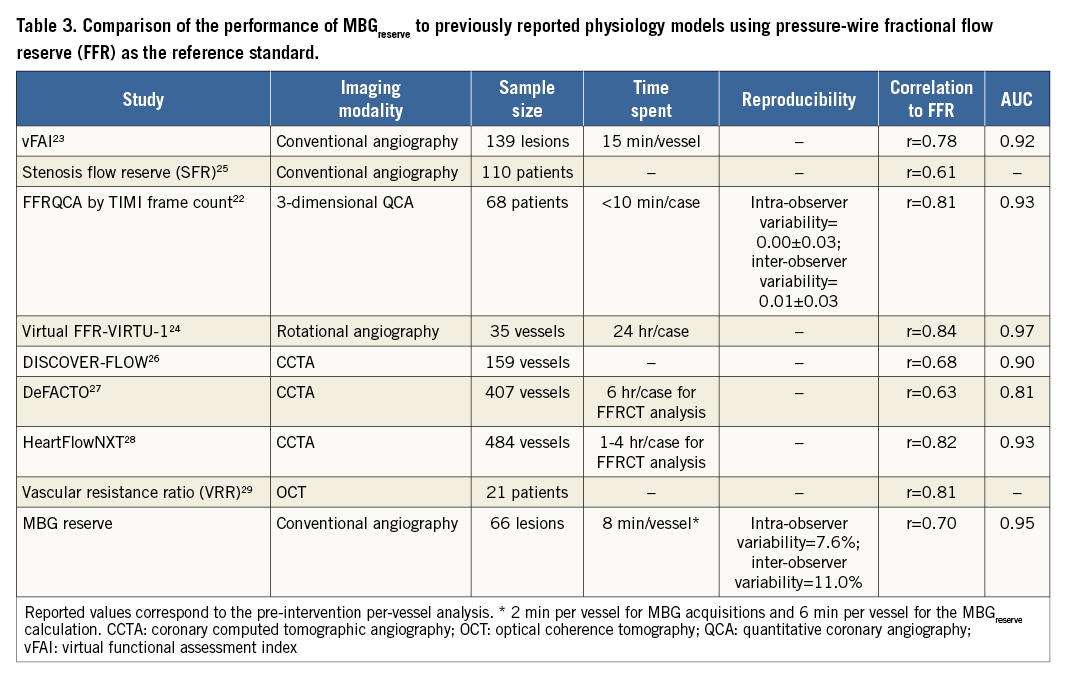
With most current virtual FFR methods, however, the flow used to calculate the FFR is pre-specified and assumed to be equal in all stenoses unless there is large variation in hyperaemic blood flow. This is related to assumptions with computational flow dynamics and may represent a limitation with angiographic or CCTA-based techniques. With CCTA on the other hand, modelling of theoretical coronary artery flow is required to derive the necessary parameters from the shape of the coronary lesions and to calculate CTFFR30. Such modelling, however, may be challenging in patients with heavy coronary calcification and irregular heart rhythm.
QUANTITATIVE MYOCARDIAL BLUSH GRADE AND CURRENT FINDINGS
The assessment of MBG is a simple, fast and cost-effective modality for the prompt diagnosis of microvascular function during routine cardiac catheterisation without the need for additional wires or imaging sequences. Instead of focusing on epicardial anatomy and without theoretical assumptions, MBG can serve as a surrogate marker of myocardial blood flow. Thus, for the first time in the current literature, we present a wire-guided FFR comparison to a computer-assisted method, which enables the direct quantification of microvascular integrity.
In previous studies, we and others demonstrated that the quantification of MBG can be performed on coronary angiograms of either CAD or CAV patients31. In this regard, Gmax/Tmax is a useful surrogate parameter of microvascular integrity, which can estimate clinical outcomes in heart transplant recipients with impaired perfusion reserve but without angiographically evident atherosclerosis7,32. In addition, Gmax/Tmax predicts infarct transmurality and functional recovery in patients with STEMI and NSTEMI6,8,33.
In this study, we found a good correlation between MBGreserve and wire-guided FFR. The high accuracy of MBGreserve for prediction of ischaemic CAD was established without an additional wire or theoretical assumptions for microcirculation and collaterals as with all virtual FFR methods so far. Thus, MBGreserve may be an alternative to FFR because of procedural costs and patient safety. Although MBGreserve ≥2.1 was highly predictive for normal FFR >0.8, some vessels with MBGreserve <2.1 still exhibited normal FFR >0.8. This may be related to increased microvascular resistance due to diabetes, metabolic syndrome or microvascular embolisation after PCI. In this regard, the association of MBGreserve with FFR, coronary flow reserve and microvascular resistance merits further investigation in future studies.
Limitations
Our study has some limitations. MBGreserve is a surrogate marker of the epicardial and microvascular flow within a coronary territory so that, in case of more than one moderate anatomic lesion, a differentiation of which narrowing is more significant may not be possible by this method. In addition, the number of patients included is relatively small and the cut-off value of MBG for the prediction of the physiological significance of coronary lesions by FFR may not be applicable in other patient cohorts. Currently, a commercial software tool is available (namely QuBE [Quantitative Blush Evaluator]; http://qube.sourceforge.net/), which was utilised in the TAPAS trial8, and can be used for MBG assessment. However, it should be noted that a different methodology is used compared to our software tool, which is currently not freely available. In addition, myocardial blood flow reserve by cardiac magnetic resonance was not available in our study, which is closely associated to microvascular function and possibly closely related to MBGreserve. However, the evidence for FFR and prognosis is greater compared to that available for coronary flow reserve. Finally, further studies are needed for the evaluation of MBGreserve in diffuse coronary atherosclerosis and in serial coronary lesions.
Conclusions
Quantification of MBG can be measured simultaneously with FFR during pharmacologic hyperaemia and in the catheterisation laboratory, providing reproducible assessment of the myocardial perfusion reserve (MBGreserve). This parameter is closely related to FFR measures. A more than 2.1-fold increase of myocardial blush was highly predictive of a normal FFR >0.8 in our study population, and thus could be potentially used for deferring PCI procedures. The assessment of MBGreserve during routine cardiac catheterisation may provide an alternative way for a real wireless FFR measurement, increasing patient safety and obviating the need for pressure wire measurements in the interests of time and cost.
| Impact on daily practice The ability of fractional flow reserve (FFR) to guide PCI procedures, leading to improved outcome of patients with stable CAD is now widely appreciated. Although FFR is a widely available procedure, it requires the insertion of a guidewire in the coronary artery, which is associated with some risk for the patient and additional costs. In our study, we demonstrated that quantification of myocardial blush grade (MBG) can be measured simultaneously with FFR. MBG and FFR are closely related to each other. Thus, the assessment of MBG during routine cardiac catheterisation may provide an alternative way to estimate FFR, obviating the need for a pressure wire insertion into the coronary artery, in the interests of patient safety, time and cost. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
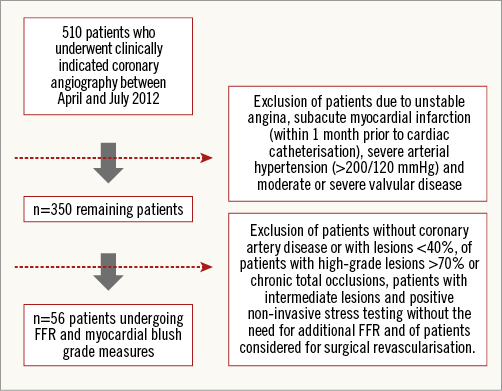
Appendix Figure 1. Study flow chart.
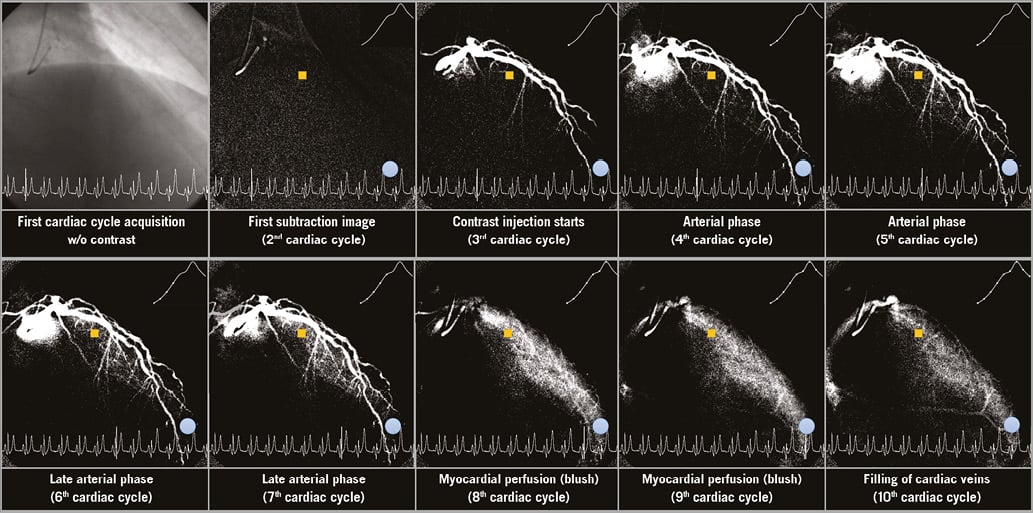
Appendix Figure 2. Image series for MBG intensity rise assessment after background subtraction in the LAD perfusion territory. Measurement of MBG over time is provided by placing a blue ROI in the distal part of the LAD.
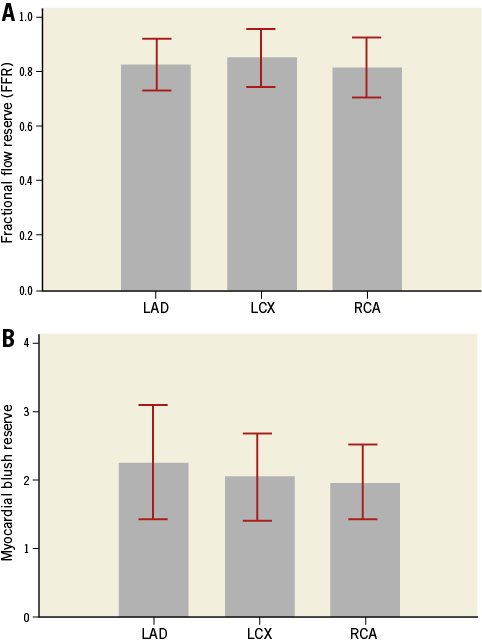
Appendix Figure 3. Distribution of FFR and MBG reserve values within the three major coronary territories.
Moving image 1. The presence of moderate myocardial blush in the distal septal branches can be appreciated during pharmacologic hyperaemia prior to PCI.
Moving image 2. Increased myocardial blush after PCI can be appreciated in the same area.
Supplementary data
To read the full content of this article, please download the PDF.
The presence of moderate myocardial blush in the distal septal branches can be appreciated during pharmacologic hyperaemia prior to PCI.
Increased myocardial blush after PCI can be appreciated in the same area.